Transcription
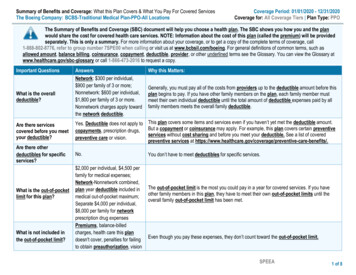
Coverage for preventive careUnderstanding your preventive care coveragePreventive care, like screenings and immunizations, helps you and your familystay healthier and can help lower your overall out-of-pocket medical costs.Talk to your doctor about what types of preventive care are appropriate for you.A guide to preventive services covered at no costAs a result of the health care law, most Independence Blue Cross(Independence) health plans now include coverage for certain designatedin-network preventive services with no cost-sharing. This means that you donot have to pay copays, coinsurance, or deductibles when you receive preventivecare from a participating, in-network provider.As a result of the health carelaw, most IndependenceBlue Cross health plans nowinclude coverage for certaindesignated in-networkpreventive services withno cost-sharing.
What are preventive services?Preventive services typically include yearly check-ups, screenings, andimmunizations that can help you and your family members stay healthyand avoid or delay health problems.Are these services always covered with no cost-sharing?To be covered without any member cost-sharing, the designated preventive tests,examinations, and other medical services you receive must be billed by thein-network provider as preventive care and not be part of a diagnostic procedureor ongoing treatment for an existing condition. If a procedure is consideredpreventive, there is no cost-sharing. If a procedure is not consideredpreventive, or you don’t fall within the coverage guidelines, charges may apply.Examples of preventive and non-preventive services:George receives a blood test to measure cholesterol levels at his annualwellness exam.The office visit and blood test are both preventive proceduresbecause George has no known symptoms, illness, or injury.Jerry makes quarterly visits to his doctor for blood tests to check cholesterollevels and confirm that his medication dosage is appropriate.The quarterly blood tests are not preventive care because they arepart of a treatment regimen for Jerry’s existing condition.Cate visits her in-network doctor for her annual mammogram.This service is covered since all mammograms are covered 100 percent.During his annual wellness exam, Mike tells his doctor that he hasexperienced some unexpected weight loss, which prompts his doctorto send him for a colonoscopy.Mike’s wellness exam is covered, but the colonoscopy is considereda diagnostic service and is subject to cost-sharing.If you receive bothpreventive anddiagnostic servicesduring the same visit,you will pay a shareof the cost for thediagnostic services.
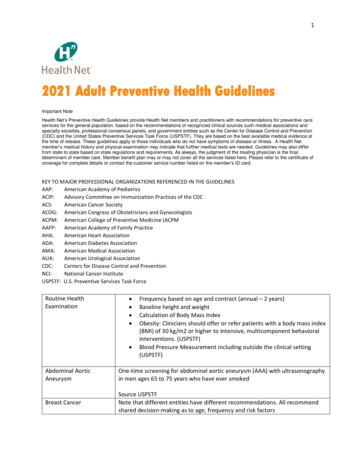
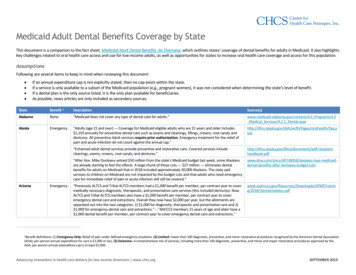
Preventive services for children (newborn to 21 years old)Pediatric preventive exams are covered at no cost. Many of the services listedare included as part of children’s routine preventive visits with a doctor.Preventive serviceIndependence coveragePreventive care for newborns: Screening for heritable (genetic)disorders and congenitalhypothyroidism (to determine if thethyroid is functioning correctly) Eye medication to prevent gonorrhea Hearing loss screening Phenylketonuria (PKU) screening totest for a rare genetic disorder Sickle cell disease screeningAll newbornsAutism screeningAll children at 18 months and 24 monthsCounseling and education toprevent initiation of tobacco useHearing screeningHIV screeningAll school-aged children and adolescentsIron supplements (with prescriptiondrug benefit only)1Major depressive disorders(MDD) screeningObesity screening and counselingOral fluoride supplements (withprescription drug benefit only)Preventive examsAll childrenAll children 15 years and older orhigh-risk adolescentsAll children, 6 months old to 12 months oldAll children, 12 – 18 years oldAll children, 6 years and olderAll children, 6 months to 6 years andwhose primary water source lacksenough fluorideChildren: birth to 36 months, 11 visitsChildren: 3 – 17 yrs once every yearSexually transmittedinfections counselingSexually transmitted infections screeningSkin cancer counseling to minimizeexposure to harmful ultraviolet(UV) radiationVisual impairment screeningChildren: 18 – 21, once every yearAll at-risk childrenAll children, 11 years and olderAll childrenAll children, 5 years old and youngerImmunizations (adults and children) 2 Diphtheria, Tetanus, Pertussis (DTaP) Haemophilus influenzae type b (Hib) Hepatitis A Hepatitis B Herpes zoster (shingles) Human papillomavirus (HPV) Inactivated poliovirus (IPV) Influenza vaccine (flu) Measles, mumps, rubella (MMR) Meningococcal (MCV) Pneumococcal (pneumonia) Rotavirus Varicella (chickenpox)1 Preventive prescription drugs – If your healthplan includes a prescription drug benefit, certainprescription drugs used in preventive care are coveredwith no cost-sharing when the prescription is filled ata participating in-network pharmacy. Refer to yourmember handbook and/or benefit booklet to determineif your plan covers in-network preventive drugs withno cost-sharing.2 More information about recommended immunizations isavailable from the Centers for Disease Control atwww.cdc.gov/vaccines/schedules.
Preventive services for men and women(22 years and older)Adult preventive exams are covered at no cost. Many services listed, such asblood pressure screening, may be included as part of a routine preventivevisit with a doctor.Preventive serviceIndependence coverageAbdominal aortic aneurysm (AAA)screening to detect weakening of theheart’s main arteryMen, 65 – 75 years old, onceper lifetimeAlcohol misuse screening and counselingAspirin use counseling for use of aspirinto prevent heart diseaseBlood pressure screeningCholesterol (lipid) screeningColorectal cancer screening – includesbarium enema, colonoscopy, fecal occultblood testing, and sigmoidoscopy3All adults, once per yearMen, 45 – 79 years old; Women,55 – 79 years oldAll adultsAll adults, 18 and olderFor fecal occult: All adults,50 years and older, once every yearTalk to your doctor aboutpreventive and diagnosticservices you receive todetermine the treatmentthat is best for you.For flexible sigmoidoscopy: all adults,50 years and older, once every 3 yearsFor barium enema: All adults, 50 yearsand older, once every 3 yearsDepression screeningDiabetes (type 2) screeningHealthy diet counselingHepatitis C virus screeningHIV screeningObesity screening and counselingOsteoporosis screeningPrevention of falls/ Vitamin Dsupplementation in older adultsPreventive examsSexually transmittedinfections counselingTobacco use screening and cessationinterventions for tobacco usersSyphilis (sexually transmittedinfection) screeningFor colonoscopy: All adults, 50 yearsand older, once every 10 yearsAll adults, once every yearAll adults with high blood pressureAll adults with risk factors for heartdisease and diet-related chronic conditionAll high-risk adultsAll high-risk adults, including allpregnant womenAll adultsWomen: 60 and older, once every two yearsAll high-risk adults, 65 years and olderAdults: 22 – 39, once every 2 yearsAdults: 40 years and older, once every yearAll at-risk adultsAll adultsAll high-risk adults, includingpregnant women3 Refer to your member handbook and/or benefit bookletto determine whether your health plan includes thePreventive Plus benefit. This benefit has a site-of-servicedifferential, which means that how much you pay isdifferent depending on the location where you receive thecovered service. If your plan includes Preventive Plus,there is 0 cost-sharing — no copayment, deductible,or coinsurance — when you receive a preventivecolonoscopy to screen for colorectal cancer at anin-network freestanding ambulatory surgery center(ASC). A freestanding ASC is an independent healthcare facility — one that is not hospital-based — whereyou can receive surgery and other medical procedures.If, however, you receive a preventive colonoscopy atan outpatient ASC that is hospital-based, you will becharged a copayment of up to 750. Log in atwww.ibxpress.com and use the Find a Doctor tool tofind a Preventive Plus provider. Look for the P icon tochoose a provider where you can take advantage of thePreventive Plus benefit.
Preventive services for women, including pregnant womenWell-woman visits to obtain the recommended preventive services arecovered at no cost. Many services listed may be included as part of a routinewell-woman visit with a doctor.Preventive serviceIndependence coverageAnemia screening (low red blood countcaused by iron deficiency)All pregnant womenBacteriuria urinary tractinfection screeningAll pregnant women at first prenatal visitor at 12 to 16 weeks’ gestationBreast/ovarian cancer genetic riskassessment and BRCA (cancer gene)mutation testingMammogram (breast cancer screening)Breast cancer counseling todiscuss use of medicine to preventcancer (chemoprevention)Breastfeeding support, supplies,and counseling4Cervical cancer screening (Pap test)Chlamydia (sexually transmittedinfection) screeningFDA-approved methodsof contraception5Domestic and interpersonal violencescreening and counselingFolic acid supplementsAll women with family history associatedwith high riskGestational diabetes (diabetes duringpregnancy) screeningGonorrhea (sexually transmittedinfection) screeningHepatitis B screeningHuman papillomavirus (HPV) screeningPreventive gynecological examsRh (D) incompatibility screening(blood type and antibody testing)Sexually transmittedinfections counselingAll adult womenAll women at high risk for breast cancerAll pregnant women, during andafter pregnancyAll adult womenAll adult womenAll adult women who maybecome pregnantAll adult womenAll adult women who maybecome pregnantAll pregnant womenAll adult womenAll pregnant womenAll adult womenAll womenAll pregnant womenSexually active adolescents andhigh-risk adults4 Breastfeeding support, supplies, and counseling –Covered members may rent or purchase one portablemanual or electric breast pump per pregnancy, as well anynecessary supplies, from a participating in-networkdurable medical equipment supplier with no costsharing. Independence will apply reasonable medicalmanagement techniques to determine the frequency,method, treatment, or setting for breast pumps. Coveredmembers have access to comprehensive lactationsupport and counseling by a trained in-network providerduring pregnancy and/or the postpartum period with nocost-sharing.5 FDA-approved methods of contraception – Medicalcontraceptive procedures, including implantablecontraceptive devices and injectable contraceptives,are covered with no cost-sharing when performed byparticipating in-network providers. Certain FDAapproved contraceptives are covered with nocost-sharing when the prescription is filled at aparticipating in-network pharmacy. Other exemptionsmay apply. Refer to your member handbook and/orbenefit booklet to determine if your plan coversin-network preventive services and/or preventive drugswith no cost-sharing.This list of covered preventive services is subject to change based on guidelines from the U.S. Preventive Services Task Forceand other nationally recognized sources.Not all health plans cover certain designated preventive services with no cost-sharing. If your health plan applies membercost-sharing for in-network preventive services, you may be charged a copayment, coinsurance, or deductible amount.Refer to your member handbook and/or benefit booklet to determine your plan’s coverage for preventive services.Independence Blue Cross offers products through its subsidiaries Independence Hospital Indemnity Plan,Keystone Health Plan East and QCC Insurance Company, and with Highmark Blue Shield — independentlicensees of the Blue Cross and Blue Shield Association.2014-2343 1/15
participating in-network providers. Certain FDA-approved contraceptives are covered with no cost-sharing when the prescription is filled at a participating in-network pharmacy. Other exemptions may apply. Refer to your member handbook and/or benefit booklet to determine if your plan cove