Transcription
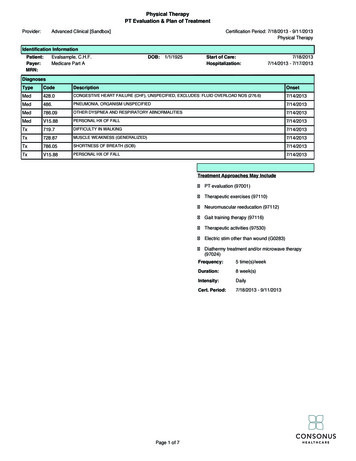
Physical TherapyPT Evaluation & Plan of TreatmentProvider:Advanced Clinical [Sandbox]Certification Period: 7/18/2013 - 9/11/2013Physical TherapyIdentification InformationPatient:Payer:MRN:Evalsample, C.H.F.Medicare Part ADOB:1/1/1925Start of Care:Hospitalization:7/18/20137/14/2013 - CONGESTIVE HEART FAILURE (CHF), UNSPECIFIED, EXCLUDES: FLUID OVERLOAD NOS (276.6)7/14/2013Med486.PNEUMONIA, ORGANISM UNSPECIFIED7/14/2013Med786.09OTHER DYSPNEA AND RESPIRATORY ABNORMALITIES7/14/2013MedV15.88PERSONAL HX OF FALL7/14/2013Tx719.7DIFFICULTY IN WALKING7/14/2013Tx728.87MUSCLE WEAKNESS (GENERALIZED)7/14/2013Tx786.05SHORTNESS OF BREATH (SOB)7/14/2013TxV15.88PERSONAL HX OF FALL7/14/2013Treatment Approaches May IncludePT evaluation (97001)Therapeutic exercises (97110)Neuromuscular reeducation (97112)Gait training therapy (97116)Therapeutic activities (97530)Electric stim other than wound (G0283)Diathermy treatment and/or microwave therapy(97024)Page 1 of 7Frequency:5 time(s)/weekDuration:8 week(s)Intensity:DailyCert. Period:7/18/2013 - 9/11/2013
Physical TherapyPT Evaluation & Plan of TreatmentProvider:Advanced Clinical [Sandbox]Certification Period: 7/18/2013 - 9/11/2013Physical TherapyIdentification InformationPatient:Payer:MRN:Evalsample, C.H.F.Medicare Part ADOB:1/1/1925Plan of TreatmentShort-Term Goals#1.0#2.0#3.0#4.0Patient will safely perform bed mobility with Min (A) with 4-/5 BLE Strengthand 10% tactile cues and 10% verbal cues while maintaining oxygensaturation 90% in order to safely maneuver in/out of bed. (Target:7/31/2013)Patient will increase bilateral hip extension range of motion to 15 degreesto complete sit to stand transfers with 4WW with full standing posture withCGA and 10% verbal cues and 10% tactile cues for proper sequencingand for safety awareness. (Target: 7/31/2013)Patient will decrease risk for falls/injury as evidenced by an increase inscore to 20 seconds (moderate fall risk) on the Timed Up and GoAssessment. (Target: 7/31/2013)Patient will increase bilateral ankle dorsiflexion to 15-20 degrees to exhibitnormalized gait pattern, including heel first contact during initial contactand weight acceptance, while safely ambulating 250 feet with CGA using4WW on level surfaces while maintaining RPE levels at 13 ("somewhathard") and oxygen saturation 90% and w/o abnormal change in vitalsigns post activity. (Target: 7/31/2013)Long-Term Goals#1.0#2.0#3.0#4.0#5.0Patient will safely perform bed mobility tasks with Independence withoutuse of siderails due to improvements in trunk and bilateral LE strength,and 0% verbal cues and 0% tactile cues for proper sequencing and forproper positioning in order to get in/out of bed. (Target: 9/11/2013)Patient will safely perform all transfers with 4WW with ModifiedIndependence using AD due to improvements in hip extension range ofmotion and 0% verbal cues and 0% tactile cues for safety awareness andfor proper sequencing in order to facilitate functional independencemaintaining RPE levels between 11-13 ("light" to "somewhat hard") andoxygen saturations above 90%. (Target: 9/11/2013)Patient will decrease risk for falls/injury as evidenced by an increase inscore to 12 seconds (low fall risk) on the Timed Up and Go Assessment.(Target: 9/11/2013)Patient will demonstrate improved cardiovascular tolerance and responseto exercise, mobility, and self-care, as evidenced by completion of andincrease of Six Minute Walk (6MWT) test results with 4WW to 650 feet in6 minutes with RPE levels maintained at 11-13 ("light" to "somewhathard") and vital signs returning to resting levels after 2-3 minutes followingtest. (Target: 9/11/2013)Patient will safely ambulate on level surfaces Unlimited Distances using4WW with Modified Independence with adequate toe clearance,normalized gait pattern, functional dynamic balance and functional speedand amplitude 100% of the time due to increased ankle dorsiflexion, whilemaintaining oxygen saturation 90% and w/o abnormal change in vitalsigns post activity to increase independence within home, to increaseindependence within community and to return to prior living setting andsupervision level maintaining RPE levels at 11-13 ("light" to "somewhathard"). (Target: 9/11/2013)Patient Goals: "To not get so tired when I move around". "To be able to go out intomy garden and take care of my granddaughter".Potential for Achieving Goals: Patient demonstrates good rehab potential asevidenced by high PLOF, motivated to participate, motivation to return to PLOF,insight regarding functional deficits, ability to follow 2-step directions, strong familysupport and ability to retain new information over time.Participation Patient/Caregiver participated in establishing POTPage 2 of 7Start of Care:Hospitalization:7/18/20137/14/2013 - 7/17/2013
Physical TherapyPT Evaluation & Plan of TreatmentProvider:Advanced Clinical [Sandbox]Certification Period: 7/18/2013 - 9/11/2013Physical TherapyIdentification InformationPatient:Payer:MRN:Evalsample, C.H.F.Medicare Part AOriginal Signature:DOB:1/1/1925Start of Care:Hospitalization:Electronically signed by Sarah Shearer-Smith, PT7/18/20137/14/2013 - 7/17/20137/24/2013 11:09:13 AM PDTDateI certify the need for these medically necessary services furnished under this plan of treatment while under my care from7/18/2013 through 9/11/2013.Physician Signature Not RequiredPhysician Signature:Date:Dr SoosInitial Assessment / Current Level of Function & Underlying ImpairmentsFactors Supporting Medical NecessityReferralMedical HxReason for Referral: Patient referred to PT due to new onset of decrease in strength, reduced functional activitytolerance, reduced static and dynamic balance, reduced ADL participation, decrease in functional mobility andincreased need for assistance from others placing patient at risk for compromised general health, falls, further declinein function, inability to safely return to PLOF and decreased leisure task participation. Due to medical complexity,patient is unlikely to recover function without therapy monitoring and intervention.Current: Patient admitted to hospital on 7/14 following decline of strength and increasing shortness of breath over theprevious week, resulting in a fall on the a.m. of 7/14. Patient reports that she had increasing levels of fatigue with allactivities prior to hospitalization and fell while walking outside her home due to feeling "exhausted" and tripping onuneven surface. Patient admitted to hospital w/ diagnoses of: acute on chronic CHF exacerbation, pneumonia,dyspnea/shortness of breath, and s/p fall.Prior: Rt hip fx with ORIF 2011, A-fib, HTNComplexitiesPrior TxPrior LivingCo-Morbidities Impacting Tx: RUG level is appropriate due to: need for multiple therapies, medical complexityrequiring therapy to be broken into multiple shorter sessions to reach goal, requires use of physical agent modalitiesfor multiple impairments, significant impairments to multiple areas of the body which require treatment and medicallynecessary rest periods require extended monitoring of O2 sats, HR, blood pressure.Outcome: Was seen by PT last year for Rt hip fx and ORIF. Participated well and met goals to return home althoughmedical complications required extra time to reach goals.Environment Patient lived alone at home, requiring outside assistance.D/C PlanAnticipated Plan Patient to live at home w/support/(A) from others.Prior LevelPLOF: Bed Mobility (I); Transfers MI; Level Surfaces MI; Distance Level Surfaces Unlimited Distances;Assistive Device Four-Wheeled Walker; Patient lived alone in one-story family home with two steps at front doorand garage door. Modified independent with all household and community mobility with 4WW. Requires assistancewith heavy household tasks provided by hired help. Daughter drove her to shop 1x/wk. Patient enjoys gardening andcared for 4 y/o granddaughter 1 day/wk.Background AssessmentPrecautionsIncludes: Pulse-ox fluctuations, O2 PRN, Anxious and Fall risk.Directives / Code Status DNRRespiratory Status Patient exhibits congestion,Patient presents with productive cough; Vision Patient wears glasses 24 hr. ; Hearing WFL; Hand Dominance Patient is right-handed.Page 3 of 7
Physical TherapyPT Evaluation & Plan of TreatmentProvider:Advanced Clinical [Sandbox]Certification Period: 7/18/2013 - 9/11/2013Physical TherapyIdentification InformationPatient:Payer:MRN:Evalsample, C.H.F.Medicare Part ADOB:1/1/1925Start of Care:Hospitalization:7/18/20137/14/2013 - 7/17/2013Initial Assessment / Current Level of Function & Underlying ImpairmentsJoint ROM/Goniometric MeasurementsJointsRight Hip Impaired; Right Knee WNL; Ankle ImpairedAROM - Right HipFlexion (120 ) WNL; Extension (30 ) 0 - 10 (10 range); Abduction (45 ) WNL; Internal Rotation (45 ) WNL;External Rotation (45 ) WNLAROM - RightAnkleJointsAROM - Left HipDorsiflexion (20 ) 0 - 10 (10 range); Plantar Flexion (50 ) 0 - 40 (40 range); Inversion (35 ) 0 - 30 (30 range); Eversion (15 ) 0 - 10 (10 range)Hip Impaired; Knee WNL; Ankle ImpairedFlexion (120 ) WNL; Extension (30 ) 0 - 10 (10 range); Abduction (45 ) WNL; Internal Rotation (45 ) WNL;External Rotation (45 ) WNLAROM - Left Ankle Dorsiflexion (20 ) 0 - 10 (10 range); Plantar Flexion (50 ) 0 - 40 (40 range); Inversion (35 ) 0 - 30 (30 range)LE ROMRLE ROM Impaired (Rt LE lacks both passive and active full hip extension and full ankle dorsiflexion needed todecrease fall risk and improve standing balance/gait quality.); LLE ROM Impaired (Lt LE lacks both passive andactive full hip extension and full ankle dorsiflexion needed to decrease fall risk and improve standing balance/gaitquality.)Strength / Manual Muscle TestingRLEHip Impaired; Knee Impaired; Ankle ImpairedStrength - RightHipFlexion 4-/5; Extension 3 /5; Abduction 3 /5; Adduction 4-/5Strength - RightKneeStrength - RightAnkleLLEFlexion 4-/5; Extension 4-/5Dorsiflexion 3 /5; Plantar Flexion 3 /5; Inversion 3 /5; Eversion 3 /5Hip Impaired; Knee Impaired; Ankle ImpairedStrength - Left Hip Flexion 4-/5; Extension 3 /5; Abduction 3 /5; Adduction 4-/5Strength - LeftKneeStrength - LeftAnkleLE StrengthBalanceFlexion 4-/5; Extension 4-/5Dorsiflexion 3 /5; Plantar Flexion 3 /5; Inversion 3 /5; Eversion 3 /5BLE Strength 3 /5 (Bt LE strength 3 to 4-/5Bt ankles 3 /5Bt hips and knees 4-/5)Sitting BalanceStatic Sitting SBA; Dynamic Sitting Min (A)Standing BalanceStatic Standing Min (A); Dynamic Standing Mod (A) (For correction of loss of balance)Balance LossDirection of Loss RetrogradeReactions &StrategiesRighting Reactions Present but delayed; Protective Extension Present but delayed; Ankle Strategy Present butdelayed; Anticipatory Reactions Present but delayedPage 4 of 7
Physical TherapyPT Evaluation & Plan of TreatmentProvider:Advanced Clinical [Sandbox]Certification Period: 7/18/2013 - 9/11/2013Physical TherapyIdentification InformationPatient:Payer:MRN:Evalsample, C.H.F.Medicare Part ADOB:1/1/1925Start of Care:Hospitalization:7/18/20137/14/2013 - 7/17/2013Initial Assessment / Current Level of Function & Underlying ImpairmentsAdditional Abilities/Underlying ImpairmentsCardioPulmonaryFunctionTone and PosturePain and EdemaCoordinationSensory TestFindingsCognitionVisual AssessmentHistory andAnalysisTestingO2 Sats At Rest: 94%; O2 Sats w/Activity: 85%; Type Needed Oxygen; O2 Amount Needed 2 liters per minuteBP at Rest (Systolic/Diastolic): 160/90; Heart Rate at Rest 80 beats/min; BP with Activity (Systolic/Diastolic):165/85; Heart Rate w/Activity 130 beats/min; Activity Duration 30 - 60 secondsPosture Symmetrical posture throughoutPain at Rest 0/10; Pain With Movement 0/10; Edema 1 edema (Edema present in Bt lower legs (ankles andcalves). Bt LE swelling increases if legs kept in dependent position greater than 60 minutes. Edema currentlymanaged with medications, positioning, active movement, and ted hose stockings.)Gross Motor Coordination ImpairedLight Touch Intact; Deep Touch / Pressure Intact; Vibration IntactOriented To Person,Place,Temporal Concepts; Follows Directions Two-step w/o (A); Safety Awareness Min (A);New Learning Capacity Impaired (Per OT eval, able to learn new tasks but needs memory aides and strategies withmore complex tasks.)Medical History WFL; Eyes Aligned YesStatic Visual Acuity 20/25; Smooth Pursuits Intact; Saccades Intact; Visual Field IntactFunctional AssessmentBed MobilityTransfersGaitGait AnalysisOther AreasBed Mobility Mod (A); Underlying Impairments: Decreased strength, Decreased trunk and motor control, Assistrequired for lifting LE up onto bed for sit to supine, Assist required for lifting shoulders/trunk up from bed for supine tosit.Transfers Min (A) (RPE level 15); Sit -- Stand Min (A); Stand Pivot Min (A); Underlying Impairments:Limitations in ROM, Decreased strength, Gross motor coordination and Static and dynamic balance.Level Surfaces Min (A) (Moderate assist for correction of loss of balances which occur with direction changes,stepping backwards, or when patient is distracted or performaning dual-activities. RPE scale of 15. Patient requires5 minutes for vital signs and RPE levels to return to resting levels following activity.); Distance Level Surfaces 100feet; Assistive Device Four-Wheeled Walker; Rest Breaks 2; Time to Achieve Distance 3 - 5 mins; NegotiatingObstacles Min (A)Deviations/Patterns: Patient exhibits flat foot during weight acceptance, inadequate hip extension, forward lean oftrunk, wide base of support, decreased velocity and shuffling gait which are associated with the underlying causes ofinadequate ankle dorsiflexion, inadequate hip extension, poor postural control, lack of/impaired coordination, muscleparesis/weakness and reduced functional activity tolerance.Fall Predictors: History of fall(s), Decreased ankle dorsiflexor strength, Decreased ankle plantar flexion strength,Impaired ankle strategy and Delayed anticipatory reactions.Residential Mobility MIObjective Tests/Measures & Additional AnalysisAssessmentsOtherAdditionalAnalysisTimed Up and Go 30 seconds (very high fall risk) (10 foot TUG Avg score of three trials is 32 seconds.Performed with 4WW.)Home Exercise Program Patient does not currently have a HEP and requires the skills of a therapist to establish anappropriate program. (Patient does not currently have a HEP and requires the skills of a therapist to establish andtrain an appropriate program.)Other : Trunk strength:Abdominals/Flexors - 3 /5Extensors - 3 5Page 5 of 7
Physical TherapyPT Evaluation & Plan of TreatmentProvider:Advanced Clinical [Sandbox]Certification Period: 7/18/2013 - 9/11/2013Physical TherapyIdentification InformationPatient:Payer:MRN:Evalsample, C.H.F.Medicare Part ADOB:1/1/1925Start of Care:Hospitalization:7/18/20137/14/2013 - 7/17/2013Initial Assessment / Current Level of Function & Underlying ImpairmentsClinical ImpressionsClinical Impressions: Expect progress towards goals to be slow due to compromised cardiovascular status, as well as compromised vitalsign response to activity and exercise. Patient self-reports RPE (exertion) levels above normal and prescribed levels during and followingactivity, and requires 5 or more to return to resting levels of vital signs. Patient has good rehab potential to return home at prior level offunction with skilled PT intervention including training in recognizing and monitoring RPE/exertion levels, instruction in pacing/pursed lipbreathing/and energy conservation techniques, instruction in relaxation strategies, monitoring of vital signs and response to activity/exerciseand adjustment of treatment approaches as needed, as well as progressive strength training for trunk extensors, ankledorsiflexors/plantarflexors, and hip extensors/abductors. Skilled PT also required for stretching/joint mobilizations to gain needed hip andankle ROM and neuro re-ed to improve static/dynamic balance, coordination, and ankle strategy to decrease fall risk. Will benefit fromNMES to improve muscle strength and timing.Page 6 of 7
Physical TherapyPT Evaluation & Plan of TreatmentProvider:Advanced Clinical [Sandbox]Certification Period: 7/18/2013 - 9/11/2013Physical TherapyIdentification InformationPatient:Payer:MRN:Evalsample, C.H.F.Medicare Part ADOB:1/1/1925Tests/Measures and OutcomesPage 7 of 7Start of Care:Hospitalization:7/18/20137/14/2013 - 7/17/2013
Gait training therapy (97116) Therapeutic activities (97530) Electric stim other than wound (G0283) Diathermy treatment and/or microwave therapy (97024) Frequency: 5 time(s)/week Duration: 8 week(s) Intensity: Daily Cert. Period: 7/18/2013 - 9/11/2013 Page 1 of 7 PT Evaluation & Plan of Treatment