Transcription
Fact Sheet - 2021 Part C and D Star RatingsNote: The information included in this Fact Sheet is based on the 2021 Star Ratings published on theMedicare Plan Finder on October 8, 2020. For details on the Medicare Advantage (MA) and Part D StarRatings, please refer to the 2021 Part C & D Star Ratings Technical Notes available ionThe Centers for Medicare & Medicaid Services (CMS) publishes the Medicare Part C and D Star Ratingseach year to measure the quality of health and drug services received by beneficiaries enrolled in MedicareAdvantage (MA) and Prescription Drug Plans (PDPs or Part D plans). The Star Ratings also reflect theexperiences of beneficiaries and assist beneficiaries in finding the best plan for them. The Star Ratingssupport CMS’s efforts to put the patient first in all of our programs. As part of this effort, patients shouldbe empowered to work with their health care providers to make health care decisions that are best for them.An important component of this effort is to provide Medicare beneficiaries and their family members withmeaningful information about quality and cost to assist them in being informed and active health careconsumers.Highlights of Contract Performance in 2021 Star Ratings 1Medicare Advantage with prescription drug coverage (MA-PD) contracts are rated on up to 44 uniquequality and performance measures; MA-only contracts (without prescription drug coverage) are rated on upto 32 measures; and stand-alone PDP contracts are rated on up to 14 measures. Each year, CMS conducts acomprehensive review of the measures that make up the Star Ratings by assessing the reliability of thedata, clinical recommendations, and feedback received from stakeholders. There are no new measuresintroduced for 2021 Star Ratings. CMS increased the weight of patient experience/complaints and accessmeasures from 1.5 to 2 reflecting CMS’s commitment to serve Medicare beneficiaries by putting patientsfirst, including their assessments of the care received by plans. Additional changes made throughrulemaking include moving the All-Cause Readmissions measure to the display page on www.cms.gov dueto a substantive change in the measure specifications and increasing the weight of the Statin Use in Personswith Diabetes (SUPD) measure from a weight of 1 to 3.CMS has been monitoring the impact of the 2019 Novel Coronavirus (COVID-19) public healthemergency (PHE) on Star Ratings and adopted some changes to address the impact of the PHE in theMedicare and Medicaid Programs; Policy and Regulatory Revisions in Response to the COVID–19 PublicHealth Emergency Interim Final Rule with comment period, effective March 31, 2020 (85 FR 19230, April6, 2020) (“March 31st COVID-19 IFC”). The March 31st COVID-19 IFC adopted changes to the 2021Star Ratings to accommodate disruption to data collection posed by the PHE as well as changes to the 2022Star Ratings to account for expected changes in plan performance. The intent of these changes was toeliminate some of the data collection requirements because of the public health and safety concerns withcollecting the data, and to enable plans to focus on the care and safety of Medicare beneficiaries and theiremployees. Given the extraordinary circumstances under which the healthcare system is operating, CMSwanted plans to have some degree of certainty related to Star Ratings program requirements and wanted to1Percentages in the Tables may not sum to 100 due to rounding.This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.1
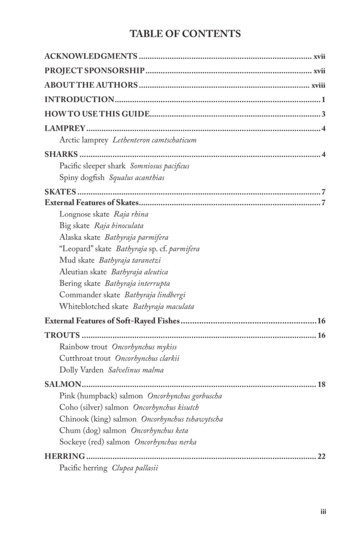
make sure plans were focused on what was most important: ensuring that Medicare beneficiaries receivedthe care and treatment they needed. The issues facing the health care system, including significantdifferences across regions and demographic groups, create unique challenges for the 2021 and 2022 StarRatings calculations. Due to these concerns, CMS eliminated the requirement to submit HealthcareEffectiveness Data and Information Set (HEDIS) and Consumer Assessment of Healthcare Providers andSystems (CAHPS) survey data for the 2021 Star Ratings and used the data from the prior year for the 2021Star Ratings calculations, including carrying forward the measure-level change scores for HEDIS andCAHPS for the Improvement measures. All other measures were updated using the most recent data.Rating DistributionThe last row in Table 1 details the trend in the average overall Star Ratings weighted by enrollment for MAcontracts offering prescription drug coverage (MA-PDs) from 2018 to 2021. Approximately 49 percent of MA-PDs (195 contracts) that will be offered in 2021 earned 4 stars orhigher for their 2021 overall rating.Weighted by enrollment, approximately 77 percent of MA-PD enrollees are currently in contractsthat will have 4 or more stars in 2021.Table 1: 2018 - 2021 Overall Star Rating Distribution for MA-PD Contracts2018 Number 2018 2018 Weighted 2019 Numberof Contracts % by Enrollment of Contracts5 stars16 4.1611.17144.5 stars58 15.0623.52644 stars97 25.1938.19943.5 stars139 36.1022.451243 stars61 15.844.20662.5 stars12 3.120.46142 stars2 0.520.020Total Rated Contracts385 100376Average Star Rating*4.07* The average Star Rating is weighted by enrollment.Overall Rating2019 2019 Weighted 2020 Number% by Enrollment of 7.4113117.557.00553.720.2340.000.0011004014.062020 2020 Weighted 2021 Number% by Enrollment of 15.8214013.722.936110.0540.250.0201004004.162021 2021 Weighted% by .254.1410.06001004.06The last row in Table 2 details the trend in the average Part D Ratings weighted by enrollment for standalone PDPs from 2018 to 2021. Approximately 42 percent of PDPs (23 contracts) that will be active in 2021 received 4 or morestars for their 2020 Part D Rating.Weighted by enrollment, about 17 percent of PDP enrollees are in contracts with 4 or more stars.Another 81 percent of PDP enrollees are in 3.5 star contracts. Close to 98 percent of PDP enrolleesare in contracts with 3.5 or more stars.This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.2
Table 2: 2018 - 2021 Part D Rating Distribution for PDPsOverall Rating5 stars4.5 stars4 stars3.5 stars3 stars2.5 stars2 stars1.5 starsTotal Number of ContractsAverage Star Rating*2018Number 12018 Weighted by Number of 2019 Weighted by Number of 2020 Weighted by Number of 2021 Weighted entContracts%Enrollment12.962.034 7.691.922 3.700.765 9.090.139.260.285 9.620.697 12.961.787 12.732.3829.6345.037 13.460.837 12.9625.0411 20.014.1331.4836.3915 28.8568.6121 38.8942.1219 34.5581.249.268.0016 30.7721.7714 25.9329.459 16.361.013.704.602 3.850.373 5.560.844 7.271.103.703.662 3.855.450 0.000.000 0.000.000.000.001 1.920.350 0.000.000 0.000.0010052 10054 10055 1003.623.343.503.58* The average Star Rating is weighted by enrollment.5-Star ContractsA total of 28 contracts are highlighted on the Medicare Plan Finder with a high performing indicatorindicating they earned 5 stars; 21 are MA-PD contracts (Table 3), two are 1876 Cost contracts (Table 4),and five are PDPs (Table 5). This is an increase from 23 5-star contracts for the 2020 Star Ratings.For 2021, 13 contracts receiving the high performing indicator did not receive it in 2020. The contractsreceiving the high performing indicator in 2021 that did not receive it in 2020 are highlighted, and thecontract number and name are italicized. The tables below show both the Employer Group Health Plan(EGHP) service areas, if applicable, and the non-EGHP service areas.Table 3: MA-PD Contracts Receiving the 2021 High Performing IndicatorContractContract NameH0332KS Plan Administrators, LLCH0524Kaiser Foundation HP, Inc.H0630H0710Kaiser Foundation HP of COSierra Health and Life InsuranceCompany, Inc.H1019CarePlus Health Plans, Inc.H1170Kaiser Foundation HP of GA, Inc.H1230Kaiser Foundation HP, Inc.Care Improvement Plus South CentralInsurance Co.Kaiser Foundation Health Plan of theMid-AtlanticParent OrganizationKelsey-Seybold MedicalGroup, PLLCKaiser Foundation Health Plan,Inc.Kaiser Foundation Health Plan,Inc.Non-EGHP Service AreaEGHP Service AreaSNP38,31813 counties in TX242 counties in TXNo1,258,88632 counties in CANot applicableYes111,17214 counties in CONot applicableYes39,998Most of the U.S.Most of the U.S.YesHumana Inc.Kaiser Foundation Health Plan,Inc.Kaiser Foundation Health Plan,Inc.166,82118 counties in FLNot applicableYes32,23512 counties in GA9 counties in GAYes33,5763 counties in HINot applicableYesUnitedHealth Group, Inc.Kaiser Foundation Health Plan,Inc.2,113Most of the U.S.No77,0531 county in NY1 county in DC, 11 counties inMD, and 12 counties in VANot applicableNoUnitedHealth Group, Inc.19,23310 counties in MANot applicableYesH2256United Healthcare Insurance Co.Tufts Associated Health MaintenanceOrganization103,97010 counties in MANot applicableYesH2422HealthPartners, Inc.4,34312 counties in MNNot applicableYesH5042CDPHP Universal Benefits, Inc.5,287NoQuartz Health Plan Corporation18,54423 counties in NY5 counties in IA, 5 counties inIL, and 27 counties in WI39 counties in NYH5262HealthPartners, Inc.Capital District Physicians'Health Plan, Inc.University of WisconsinHospitals and Clincs AuthoNot applicableNoH5410Healthspring of Florida, Inc.CIGNA56,27920 counties in FL47 counties in FLYesH5431Healthsun Health Plans, Inc.Anthem Inc.52,9063 counties in FLNot applicableYesH1537H2172H2226UnitedHealth Group, Inc.Enrolled10/2020Tufts Health Plan, IncThis communication is printed, published, or produced and disseminated at U.S. taxpayer expense.3
Enrolled10/2020ContractContract NameParent OrganizationH5526HealthNow New York Inc.15,298H5591HealthNow New York Inc.Martin’s Point Generations Advantage,Inc.Martin's Point Health Care, Inc.48,182H5652Serra Health and Life InsuranceCompany, Inc.4,902H9003Kaiser Foundation HP of the NWH9834Quartz Health Plan MN CorporationUnitedHealth Group, Inc.Kaiser Foundation Health Plan,Inc.University of WisconsinHospitals and Clincs Autho98,0352,255Non-EGHP Service AreaEGHP Service AreaSNP18 counties in NY16 counties in ME, 10 countiesin NH1 county in CO, 1 county inFL, 1 county in KS, 2 countiesin MA, 3 counties in MD, 1county in MI, 1 county in NC, 3counties in NJ, 2 counties inPA, 2 counties in TX, and 2counties in VA10 counties in OR and 3counties in WAMost of the U.S.NoNot applicableYesNot applicable1 county in OR and 1county in WAYes4 counties in MNNot applicableNoNoTable 4: 1876 Cost Contracts Receiving the 2021 High Performing Indicator 2ContractContract NameH1651Medical Associates Health Plan,Inc.H5264Dean Health Plan, Inc.ParentOrganizationMedicalAssociates Clinic,P.C.SSM HealthcareCorporationEnrolled10/2020Non-EGHP Service AreaEGHP Service Area13,45552 counties in IA, 13 counties in IL,and 13 counties in NENot applicable17,1758 counties in WINot applicableTable 5: PDP Contracts Receiving the 2021 High Performing IndicatorContractContract NameParent OrganizationS0655Tufts Insurance CompanyTufts Health Plan, IncS1822HealthPartners, Inc.HealthPartners, Inc.S3389UPMC Health Benefits, Inc.S3521S4219Enrolled10/2020Non-EGHPService AreaEGHP Service Area8,713Not applicable35 regions15,240Not applicable35 regionsUPMC Health System1,073Not applicable39 regionsExcellus Health Plan, Inc.Lifetime Healthcare, Inc.7,626Not applicable39 regionsHealth Alliance Medical PlansThe Carle Foundation764Not applicable39 regionsConsistently Low PerformersThere is only one contract identified on the Medicare Plan Finder with a low performance warning forconsistently low quality ratings as detailed in Table 6. This contract is receiving the warning for Part Cand/or Part D summary ratings of 2.5 or fewer stars from at least 2018 through 2021.21876 Cost contracts do not offer SNPs.This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.4
Table 6: 2021 Contract(s) with a Low Performance WarningContractH7680Contract NameParent OrganizationProminence HealthFirst of TexasUniversal Health Services, Inc.Reason forLowPerformanceWarningEnrolled 10/2019SNPPart C or D1,384NoLength of Time in Program and PerformanceOverall, higher Star Ratings are associated with contracts that have more experience in the MA program.MA-PDs with 10 or more years in the program are more than twice as likely to have 4 or more starscompared to contracts with less than 5 years in the program. For PDPs, the relationship is similar in thatPDPs with 10 or more years in the program do better in the Star Ratings relative to contracts with lessexperience. The tables below show the distribution of ratings by the number of years in the program(MA-PDs are shown in Table 7 and PDPs in Table 8).Table 7: Distribution of Overall Star Ratings by Length of Time in Program for MA-PDs2021 Overall Rating5 stars4.5 stars4 stars3.5 stars3 stars2.5 starsTotal Number of ContractsNumber ofContracts withLess than 5Years19930182% Less than 5YearsNumber ofContracts with5 years to Lessthan 10 Years% 5 Years toLess than 10YearsNumber ofContracts with10 or MoreYears% 10 or 022.7800.006972259Table 8: Distribution of Part D Ratings by Length of Time in Program for PDPs2021 Overall RatingNumber ofContracts withLess than 5Years% Less than 5YearsNumber ofContracts with5 Years to Lessthan 10 Years% 5 Years toLess than 10YearsNumber ofContracts with10 or MoreYears% 10 or MoreYears5 stars00.00116.6744.5 stars00.00350.0048.894 stars00.0000.001124.443.5 stars00.00116.671840.003 stars125.00116.67715.562.5 stars375.0000.0012.22Total Number of Contracts468.8945This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.5
Geographic VariationThe following eight maps illustrate the average Star Ratings from 2018 to 2021 weighted by enrollment percounty for MA-PDs and PDPs across the U.S., including territories. 3 These maps exclude EGHPs.Counties shaded in green indicate that the enrollment-weighted mean for the overall Star Rating in thecounty for MA-PDs or Part D Rating for PDPs is 4 or more stars. Similarly, counties shaded in yellowindicate that the enrollment-weighted mean rating is 3 stars, and areas shaded in orange indicate that theenrollment-weighted mean rating is less than 3 stars. Please note that the weight of patientexperience/complaints and access measures increased from the 2020 to the 2021 Star Ratings from 1.5 to 2so some of the changes from the prior year would be from the change in weighting. Areas in gray indicatedata are not available for those counties. Among the changes and updates from previous years are: 3Highly rated (4 stars or greater) MA-PDs continue to be available in the vast majority of regionsacross the country. Between 2020 and 2021, there was a small downward shift in the enrollmentweighted mean rating.In the period from 2018 through 2020, the ratings of PDPs across the country generally increased(evidenced by the greater percentage of green shaded regions on the maps over time).Comparisons of Star Ratings across years do not reflect annual revisions made by CMS to the Star Ratings methodology ormeasure set.This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.6
This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.7
2020 Star Ratings - Enrollment Weighted Average MA-PD Overall Rating in Non-EGHP CountiesThis communication is printed, published, or produced and disseminated at U.S. taxpayer expense.Missing Data1 Star1.5 Stars2 Stars2.5 Stars3 Stars3.5 Stars4 Stars84.5 Stars5 Stars
This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.9
This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.10
This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.11
2020 Star Ratings - Enrollment Weighted Average PDP Part D Rating in Non-EGHP CountiesThis communication is printed, published, or produced and disseminated at U.S. taxpayer expense.Missing Data1 Star1.5 Stars2 Stars2.5 Stars3 Stars3.5 Stars4 Stars124.5 Stars5 Stars
This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.13
This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.14
Average Star Rating for Each MeasureBelow we list the average Star Ratings for 2018, 2019, 2020 and 2021 Part C and D measures (Tables 9, 10and 11) using all measure scores for contracts that are publically reported in a given year. 4 For HEDIS andCAHPS measures, the 2021 average star does not always equal the 2020 average star even though datafrom the 2020 Star Ratings were used for those measures because the set of contracts has changed slightlyfrom last year.Table 9: Average Star Rating by Part C Measure2021 MeasureNumberMeasure2018 Average Star2019 AverageStar2020 AverageStar2021 AverageStarC01Breast Cancer Screening3.13.43.53.5C02Colorectal Cancer Screening3.43.83.83.9C03Annual Flu Vaccine3.23.23.23.2C04Improving or Maintaining Physical Health2.933.23.2C05Improving or Maintaining Mental Health3.73.33.93.3C06Monitoring Physical Activity2.92.83.23.5C07Adult BMI Assessment4.14.44.24.3C08Special Needs Plan (SNP) Care Management3.23.23.13.4C09Care for Older Adults – Medication Review4.14.44.34.3C10Care for Older Adults – Functional Status Assessment44.144C11Care for Older Adults – Pain Assessment4.444.44.5C12Osteoporosis Management in Women who had a Fracture2.62.63.13.1C13Diabetes Care – Eye Exam3.63.73.83.8C14Diabetes Care – Kidney Disease Monitoring3.74.24.14.2C15Diabetes Care – Blood Sugar Controlled4.23.74.24.2C16Rheumatoid Arthritis Management3.433.63.6C17Reducing the Risk of Falling2.532.53C18Improving Bladder Control3.13.13.23.2C19Medication Reconciliation Post-Discharge3.32.933C20Statin Therapy for Patients with Cardiovascular Diseasen/a - new in 20193.33.13.1C21Getting Needed Care3.43.33.33.3C22Getting Appointments and Care Quickly3.33.43.43.4C23Customer Service3.43.43.53.5C24Rating of Health Care Quality3.43.33.33.3C25Rating of Health Plan3.23.33.23.2C26Care Coordination3.33.43.43.4C27Complaints about the Health Plan4.344.94.8C28Members Choosing to Leave the Plan43.93.94C29Health Plan Quality Improvement3.63.43.43.2C30Plan Makes Timely Decisions about Appeals44.24.44.34Changes in the average (mean) measure-level Star Rating do not always reflect changes in performance since for somemeasures there have been significant changes in industry performance and shifts in the distribution of scores.This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.15
2021 MeasureNumberMeasure2018 Average Star2019 AverageStar2020 AverageStar2021 AverageStarC31Reviewing Appeals Decisions43.94.14.5C32Call Center – Foreign Language Interpreter and TTY Availability4.54.34.34.3Table 10: Average Star Rating by Part D Measure for MA-PDs2021 MeasureNumberMeasure2018 MA-PDAverage Star2019 MA-PDAverage Star2020 MA-PDAverage Star2021 MA-PDAverage StarD01Call Center – Foreign Language Interpreter and TTY Availability4.54.34.64.4D02Appeals Auto–Forward4.84.54.74.2D03Appeals Upheld3.93.93.83.6D04Complaints about the Drug Plan4.344.94.8D05Members Choosing to Leave the Plan3.93.93.94D06Drug Plan Quality Improvement3.74.23.73.5D07Rating of Drug Plan3.23.233D08Getting Needed Prescription Drugs3.43.53.53.5D09MPF Price Accuracy4.74.84.84.9D10Medication Adherence for Diabetes Medications3.33.73.93.7D11Medication Adherence for Hypertension (RAS antagonists)3.73.13.33.2D12Medication Adherence for Cholesterol (Statins)3.33.23.43.3D13MTM Program Completion Rate for CMR3.53.33.63.7D14Statin Use in Persons with Diabetes (SUPD)n/a - new in 20193.33.53.1Table 11: Average Star Rating by Part D Measure for PDPs2021 MeasureNumberMeasure2018 PDPAverage Star2019 PDPAverage Star2020 PDPAverage Star2021 PDPAverage StarD01Call Center – Foreign Language Interpreter and TTY Availability3.94.24.14.2D02Appeals Auto–Forward4.44.24.54.1D03Appeals Upheld3.53.13.33.1D04Complaints about the Drug Plan4.23.64.44.9D05Members Choosing to Leave the Plan3.64.13.84.1D06Drug Plan Quality Improvement3.94.23.74.1D07Rating of Drug Plan3.43.33.53.5D08Getting Needed Prescription Drugs3.43.43.53.6D09MPF Price Accuracy4.64.64.84.9D10Medication Adherence for Diabetes Medications3.22.63.33.9D11Medication Adherence for Hypertension (RAS antagonists)3.233.23.1D12Medication Adherence for Cholesterol (Statins)3.33.13.33.6D13MTM Program Completion Rate for CMR2.82.63.33.6D14Statin Use in Persons with Diabetes (SUPD)n/a - new in 20192.933This communication is printed, published, or produced and disseminated at U.S. taxpayer expense.16
Oct 13, 2020 · Number of Contracts 2019 % 2019 Weighted by Enrollment 2020 Number of Contracts 2020 % 2020 Weighted by Enrollment 2021 Number of Contracts 2021 % 2021 Weighted by Enrollment 5 stars 7 12.96 2.03 4 7.69 1.92 2 3.70 0.76 5 9.09 0.13 4.5 stars