Transcription
Medicaid Specialty Plan for Individualswith Serious Mental IllnessProvider Orientation2014
Agenda Welcome and Introductions Model Of Care Member Eligibility and Enrollment Assignment Member Benefits Magellan Complete Care Network Customer Service Center Claims and Billing – Do and Don'ts - Elements of a Clean Claim Fraud Waste and Abuse Clinical Team – Authorizations Magellan Complete Care Purpose and Goals of Orientation2Provider Orientation2014
Welcome and Introductions
Magellan Complete Care of Florida Magellan Complete Care of Florida is a specialty health plandesigned specifically for members with serious and persistentmental illness who are eligible for Medicaid benefits. It promotes a fully integrated and coordinated behavioralhealth and physical health approach that spans the continuumof care.Medicaid Our goal is to ensure that all membersreceive personalized, high-qualityhealth care tailored to their medical,mental health, and social needs.CompleteCare ofFloridaChronicHealthCondition4Provider Orientation2014SeriousMentalIllness
Our Goals Improve the overall health, longevity and well-being of members with SMI Lower the cost of care by providing better access and care coordination for thisspecial population Decrease overutilization of institutional /facility-based care and increase communitytenure for these individuals. Create system transparency and accountability through data sharing and outcometracking.5Provider Orientation2014
Recovery PhilosophyMCCFL believes that all individuals are capable of achieving recovery andresiliency outcomesWe hold firmly that individuals who rely on publicly fundedhealth and human services can live and work successfully incommunity settings when appropriate treatment andsupport are accessible and available.6Provider Orientation2014
Model of CareMedical Management & Care Coordination
Model of Care Elements Model of Care has 11 key elements:Target PopulationProvider Networkwith Special Expertiseand Use of ClinicalPractice Guidelines andProtocolsMeasurable GoalsStaff Structure &CareManagementRolesInterdisciplinaryCare Team (ICT)Model of CareTrainingHealth RiskAssessment(HRA)IndividualizedCare PlanCommunicationNetwork8Provider Orientation2014CareManagement forthe mostvulnerablepopulationPerformance &Health OutcomeMeasurement
Model of Care for Dual Eligible MembersRated 100% by CMSMemberand ICTmeet tocreate CCP360 member riskassessment completed360 Member Risk Assessment: Nursing Assessment CHI (functional status) HRA (medical/behavioral) Mental Status Exam (cognitive status)Care Plancreated onproviderportalCare Coordination Plan (CCP): BH and PH Assessment Short term goals Long term goals Interventions Team noteswww.magellancompletecareoffl.com9Provider Orientation2014Health Guide andSMI CM overseeimplementation ofplanKey clinical components occur atBehavioral Health Home: HRA within 90 days Chronic condition support Health Guides monitor progressthrough administrative reports
What does an Interdisciplinary Care Team do? Interdisciplinary Care Team is the foundationof the program. Ensures the appropriateness of the plan of care based uponmember assessments Team ensures integration of all medical and behavioralhealth needed by the memberAnalyze and incorporatethe results of the initialand annual Health RiskAssessment into the careplanCollaborate to developand annually update anindividualized care planfor each memberCommunicate tocoordinate themember’s care10Provider Orientation2014Manage the medical,cognitive, psychosocial,cultural and functionalneeds of membersEngage the member andtheir family orrepresentative in theplan of care
Primary Members of Interdisciplinary Care TeamProvides supportto the member intreatment andrecovery.Emphasizeseducation formembers andtheir family abouttheir care and thetreatmentoptionsPCPFamilyandSupportsAssess and coordinatetransitions of care: Care coordinatorsfocus on highest riskmembers Case Managersprovide behavioralhealth support andoversee the recoveryplan for each memberincluding home visitsProvider OrientationBHProviderincludingBHMPMemberSMI CaseManager11Co-Leads ICT asappropriate and isresponsible foroverall ccountable for engagingmembers in their care andsupporting recovery-basedapproaches.2014Co-Leads ICT and isresponsible foroverall clinicaldirection whenprimary diagnosis isSMIWelcomes the member,encourages activeparticipation in their care.Supports member innavigating the healthcaredelivery system.
Field Positions and their ResponsibilitiesNetwork Team Owns providercontractingrelationships Monitors Provideraccess Contracts withProviders InitiatesCredentialingProcess Processes signedagreements Responsible forprovider InServices activities Identifies andresolves providerissues Adds providers tothe CAP claimsystem HandlesAdd/Changes andDeletes forproviders Memberengagement andretentionactivitiesProviderSupportSpecialists Builds andmaintains positiverelationships withproviders Partners withotherdepartments Supports processthat addressesprovidercomplaints,claims,credentialing Orientation,training,education toproviders toimprove quality,outcomes andefficiencies andadoption of bestpractices Brokersrelationshipsbetweenbehavioral healthand physicalhealth providers Performs Medicalrecord reviewProviderSupportSpecialistscont. Assess readinessfor IntegratedHealth Homes Facilitates thetraining requiredto plan andimplement qualityimprovementprocesses andinitiatives Link practices withtools that helpthem engage inimprovementactivities: e.g.process mapping,protocols, anddecision support Provideappropriate datafrom performancereports, audits,and/or outsidesources and sharewith providers Memberengagement andretentionactivities Assess practicereadiness forworking withmembersProvider Orientation Serves as theliaison tocommunity basedorganization Expert onMedicaidprograms andbenefits Establishes arelationship withthe enrollee, thecare coordinationteam, and his/herproviders Completecommunityassessments toidentify strengths,needs andpossiblepartnerships Build andmaintaincommunityresources for theenrollees Tracks andcoordinates careto ensure memberis receivingservices Planning andparticipation incommunity eventsand health fairs Makes referrals tocase managersand communityprograms andservices, asneeded Presentationsregardingcommunityresources Memberengagement andretentionactivities2014Health Guides Completesindividualmemberassessment (suchas Health andWellnessQuestionnaire(HWQ), NewEnrolleeInterview) Follow MedicaidMarketingguidelines Rolls out lists Memberengagement andretentionactivitiesPeer SupportSpecialists Accountable forengagingmembers in theircare andsupportingrecovery-basedapproaches Acts as a rolemodel for healthybehaviors andlifestyles acrossthe membershipby sharing livedexperience withrecovery,resiliency, andself-directed care Leads WellnessRecovery ActionPlan (WRAP)groups,collaborates inimplementing allhealth servicesprograms, andprovidesperspective as amember of thecare coordinationteam Memberengagement andretentionactivitiesIntegratedCare CaseManagers Maintains acaseload of highlycomplex enrolleesin the casemanagementprogram Responsible forproviding bothbehavioral andphysical casemanagementservices tomembers,providing clinicalexpertise for carecoordinationteams, andfacilitating anintegratedapproach to caredelivery withproviders, healthhomes, enrollees,their families, andcommunityagencies andservices Coordinatescomplex carearrangements toensure quality andefficiency of careand achieve bestpossibleoutcomes Memberengagement andretentionactivitiesWellnessSpecialists Works withmembers ondeveloping skillsand confidence inself managementof chronicconditions andhealthy lifestyles(tobacco orhealthy eating, forexample) Oversees diseasemanagementplans formembers with atargeted chroniccondition Motivatesenrollees to learnand adopt selfmanagementtechniques tomaintain theirhealth andwellness Designs andconducts groupprograms andworkshops forenrollees, theirfamilies andsupports Memberengagement andretentionactivitiesCare Workers Facilitates HealthServicesdepartmentworkflow Locatescommunityservices and otherreferral locationsfor enrollees,arranges access tocare Supportscorrespondence,othercommunications Memberengagement andretentionactivities
Health ServicesResponsible for oversight of medical, dental and supplemental services provided toComplete Care members including:– utilization management,– care coordination– chronic condition support, and– nurse support for membersOur goal is to ensure consistent delivery of high-quality, affordable healthcare services to our members through Magellan Complete Care of Floridaaffiliated providers.13Provider Orientation2014
MCCFL: Addressing Barriers to Care Our core care team’shigh-touch managementhelps members makeappointments, arrangetransportation toappointments, andadhere to treatmentregimens. Our peersupport programs canhelp support themember’s health andwellness betweenappointments.14Provider Orientation2014The net result is improvementto the member’s overallhealth – mental and physical.
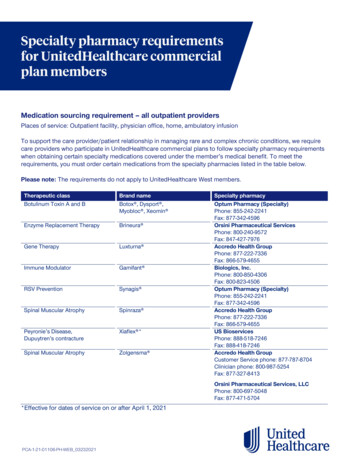
Pharmacy Claims and ReimbursementMost drugs on the Preferred Drug List(PDL) are available without priorauthorization. For drugs not on the PDL,a prior authorization is required.Medicaid Pharmacy Wrap benefit isprocessed through MMA– MMA Pharmacy Helpdesk (providers)1-800-327-8613In order for the member to have 0 copay, the pharmacy must processthe claim through both the MedImpactbenefit and the MMA benefit15Provider Orientation2014
Member Eligibility
Eligibility for Complete Care of FloridaIn order to be eligible for enrollment inMCCFL, applicants must have Medicaidbenefits and a Serious Mental Illness(SMI):– Psychotic Disorders– Bipolar Disorders– Major Depression– Schizo-affective Disorder– Delusional Disorder– Obsessive-compulsive DisorderTo verifyeligibility, theprovider canaccess ourwebsite, orcontactMemberServices at:800-327-8613 .Individuals can call the Florida Medicaid Choice Counselors at877-711-3662 / 866-467-4970 (TDD) or visit the Agency forHealth Care Administration to enroll in Magellan Complete Care.17Provider Orientation2014
Member Eligibility and ID CardMagellan Complete Care requires thatour members keep their ID card withthem at all times.If a member loses their ID card, pleasehave them contact Customer Service, tollfree, at 800-327-8613.If the member is hearing impaired, calltoll free at 800-424-1694 TTY.Magellan Complete Care will sendthem a replacement ID card within 5business days18Provider Orientation2014Please remember that a member ID cardis not a guarantee of payment forservices rendered.The provider’s office is responsible forverifying eligibility at the time of eachoffice visit.The provider can access the followingmethods to verify eligibility: Call 24-hour Eligibility Line at 800-3278613 Online at MMCofFL.com
Member Eligibility and ID Card Continued 19Provider Orientation2014
Member Benefits
Magellan Complete Care of Florida Member BenefitsMedicalBehavioral HealthPrescription ogramsPreventionProgramsPlus, Enhanced Benefits, where members can earn creditfor participation in specific health activities. The credit canthen be applied to cover costs not traditionally coveredby Medicaid, like over the counter vitamins.21Provider Orientation2014
Summary of BenefitsVisit our website to learn more about the benefits available to members, at:www.MagellanCompleteCareofFL.com22Provider Orientation2014
Magellan Complete Care Network
Magellan Complete Care Network PODS – Provider Optimization Delivery Systems Contract Coordinator Field Network Coordinator/Sr. Field Network Coordinator Contracting Manager Network management Director Provider Responsibilities Complete care of his/her enrollees– Appropriate care– Referring enrollees to behavioral health, specialty or ancillary care providers– Coordinating care with the Health Plan– Coordination of Care with other providers– Access and Availability– Referrals24Provider Orientation2014
Magellan Complete CarePartners Network Providers Claims and Billing – Hand Out Health Services/Utilization Management– Medical/behavioral; Imaging, cardiac procedures, sleep, pain (National Imaging Associates)– Magellan Pharmacy Solutions– ICORE – Specialty Medications Other––––––25Transportation - LogisticareDentaQuestVision – Florida Eye Care, Premier EyeAll-MedHearUSAILS – Post Discharged meals – Expanded BenefitProvider Orientation2014
Magellan Complete Care Trainings Initial New Provider/Office Staff On-going and as requested– Fraud Waste and Abuse– Claims– Holistic Care for Specialty populations– Behavioral Health Conditions Annual26Provider Orientation2014
Network of Specialized ExpertiseMCCFL has created a providernetwork: Of qualified providers who arelicensed and competent and havecompleted a formal credentialingreview That will use nationally recognizedclinical practice guidelines whenavailable Provide geographic coveragethroughout Florida County’s in allspecialties27Provider Orientation2014
MCCFL Provider NetworkSERVICES Outpatient CarePROVIDER TYPES Behavioral Health and MentalHealth Specialists Primary Care Providers Medical Specialists such asnephrologists, surgeons,pulmonologists, cardiologists, etc. Inpatient Care Emergency Services Durable Medical EquipmentSuppliers and Repair Laboratories Medications Radiology/Imaging Rehabilitative Services Dentists Healthy Lifestyles and Wellness Home Health Wellness and Prevention Vision28Provider Orientation2014
Benefits of Contracting with MCCFL Complete Care supports providers with services that help coordinate care,implement self-care practices, and improve adherence to treatment plans formembers. We offer a fully integrated service model. We have established a shared continuityof-care record, supported by communication across all channels. Complete Care focuses on the right program for the condition. We then implementa specialized chronic care improvement program for the diagnosed condition of themember. We practice prevention and early intervention, routine screenings, and wholehealth peer support to keep members healthy.29Provider Orientation2014
Magellan Complete CareCustomer Service
Magellan Complete CareCustomer Service CenterThe following are examples of information that can be obtained from accessing theMagellan Complete Care Website or by contacting the Customer Service Center; Eligibility Prior Authorization Lists, Authorization request forms, Electronic Web Authorizationsubmission Claims Benefits Member and Provider handbooks PCP and provider information Interpretation Services31Provider Orientation2014
Magellan Complete CareAfter Hours Access What services are offered – 24 hour access to staff– Nurse Line for members– Authorization (non-routine)– Notification of emergency care– Transition of care support – service settings and levels of care– Case management support including home care set-ups, non-emergency transportation– Contact information32Provider Orientation2014
Magellan Complete Care Linguistic and Cultural Services What services are available– TTY– Assistance for visually impaired PCP Changes Member can call and request– When the change is effective Provider– Reassignment of a member– When the change is effective33Provider Orientation2014
Provider Complaints There are three types of provider complaints with different filing requirementsPolicy -Related Complaints Filing Process - Oral orWritten Timeliness – 45 calendardays from the date theprovider becomes awareof the issue generatingthe complaint. Forms can be found inthe; 2014 MagellanComplete Care ProviderHandbook34Provider Orientation2014Utilization ManagementRelated Complaints Filing Process- Must befiled in writing. Timeliness – Providershave 45 days from theoriginal utilizationmanagement decision Forms can be found inthe; 2014 MagellanComplete Care ProviderHandbookClaims - Related Disputes Filing Process – Must befiled in writing Timeliness - Providershave 90 calendar daysfrom the time of a claimdenial to file a providercomplaint or submitadditional information ordocumentation.Complaints filed afterthat time will be deniedfor untimely filing. Thereis no second levelconsideration for casesdenied for untimelyfiling. Forms can be found inthe; 2014 MagellanComplete Care ProviderHandbook
Claims and Reimbursement
Claims Submission Process and WorkflowProvidersparticipating inMagellan CompleteCare of Florida’snetwork mustcomply with all CMSguidelines regardingcoding, claimssubmission, andreimbursementrules.36Provider Orientation2014
Claims and ReimbursementRefer to the Magellan Complete Care of Florida Complete Care ProviderOperating Manual for information of the following:Billing GuidelinesFiling Claims forPayment Medicaid ClaimsManual National CorrectCoding Initiative(NCCI) Official ICD 9CM/ICD-10Guidelines for Codingand Reporting Claims filingdeadlines Clean/Uncleanclaims Codes and modifiers ClaimsReconsiderations Non-CoveredServices37Provider Orientation2014Reimbursements Payment for CoveredServices Refunds Returned checks Offsets/AutomatedRecoveriesCoordination ofBenefits Potential payerscould include: Private healthinsurance Employmentrelated healthinsurance Medical supportfrom non-custodialparents Court judgments orsettlements from aliability insurer State worker’scompensation First party probateestate recoveries Long-term carecoverage Other federalprograms.Provider Payment andDispute Resolution Filing a claimsdispute Mailing address Timelines for filing aclaims dispute MCCFL’s processafter receiving aclaims dispute
EDI Claim SubmissionEDI Payor ID: 01260.Magellan also requires a secondary ID equal to the claims PO Box: 2097.Electronic claims are the fastest and most efficient method for you to get paid. Please consider submitting yourclaims electronically. We are pleased to offer claims submission through additional clearinghouses.The payor ID above is valid for:EmdeonCaparioAvailityOffice AllyPayerpath (Allscripts)Trizetto Provider Solutions (Gateway EDI)Relay Health (McKesson)HealthEC (IGI Health LLC)Want faster payment? Sign up today for Electronic Funds Transfer (EFT) – a secure andefficient method to receive your payments. Visit the EFT page of our provider website,www.MagellanHealth.com/provider, for the simple steps on how to register.38Provider Orientation2014
Complete Care Advantage Contact InformationPhysical and behavioral health providers can reach Magellan Complete Care of Floridaby calling provider services at:1-800-327-8613 (TTY 1-800-424-1694)Access additional resources and self-service tools on our website at:www.MagellanCompleteCareofFL.comPhysical Health Authorizations can be faxed to:1-888-656- 489439Provider Orientation2014
Fraud Waste and Abuse
Magellan Complete Care Fraud Waste and Abuse Definition of fraud, Waste, Abuse, [FWA] and Overpayments–Exclusion and Debarment From Medicaid, Medicare, and other Federal Health Care Programs Provider Roles and Responsibilities – What You Can Do–We encourage all of our providers to implement a comprehensive compliance plan to detect, prevent, monitor,and report suspected cases of fraud, waste and abuse. The U. S. Department of Health and Human Services’ Officeof the Inspector General has developed Compliance Plan guidance for a number of different health care providertypes. These guidelines can be accessed via the Internet at: http://oig.hhs.gov/fraud/complianceguidance.asp. How to Report fraud, Waste, Abuse, [FWA] and Overpayments–Bureau of Medicaid Program Integrity - 1-888-419-3456 or complete a Medicaid Fraud and Abuse Complaint Form, which is available onlineat: raud complaintform.aspx–Florida Office of the Attorney General Medicaid Fraud Control Unit at 1-866-966-7226.–Florida Department of Financial Services - Division of Insurance Fraud: 1-800- 378-0445.–U.S. Department of Health & Human Services Office of Inspector General: U.S. Department of Health & Human Services Office of Inspector GeneralATTN: OIG HOTLINE OPERATIONSPO Box 23489, Washington, DC 20026 41Telephone: 1-800-HHS-TIPS (1-800-447-8477); Fax: 1-800-223-8164; Email: HHSTips@oig.hhs.govProvider Orientation2014
Magellan Complete Care What Magellan Will Do – Magellan’s Responsibilities– Implement and regularly conduct fraud, waste and abuse prevention activities that includes but is not limited toprovider education, audits, and checking the GSA SAM, HHS-OIG LEIE, and Florida Sanction & Terminated Providersexclusion lists during credentialing/recredentialing, prior to contracting, and monthly thereafter.– Magellan’s policies contain detailed information regarding Magellan’s procedures to detect, deter, monitor, and toreport fraud, waste, abuse, and overpayments. These policies and Magellan’s Deficit Reduction Act of 2005Compliance Statement are available online at nce/compliance/dra-compliance-statement.aspx . Our policies and procedures are also available upon request.Please contact your Network Development Staff at 800.327.8613.42Provider Orientation2014
Compliance Standards
Compliance ProgramOur Compliance Program is organized to be consistent with core elements of aneffective compliance program in accordance with The Centers for Medicare &Medicaid Services (CMS) standards. The program includes, but is not limited to, thefollowing elements:Written Policies and ProceduresCompliance Officer and ComplianceCommitteeTraining and Education–––––44Fraud, Waste & AbuseGeneral ComplianceCode of ConductPrivacy & SecurityModel of CareProvider Orientation Effective Lines of Communication Enforcement Standards through Wellpublicized Disciplinary Guidelines Monitoring and Auditing Corrective Action Procedures2014
Measurements of Program SuccessMCCFL will monitor process metrics and gather baseline data in the first year of thedemonstration. Measures of success will be in the following domains:Access andAvailabilityCareCoordinationHealth and WellBeingMental andBehavioral HealthPatient/CaregiverExperienceScreening andPreventionCost of Care45Provider Orientation2014Health Outcomes(HEDIS)Quality of Life
Resources
Provider Website This website is continually updated to provide easy access to information andgreater convenience and speed in exchanging information with Magellan. Visit ourwebsite at: www.magellancompletecareoffl.comAvailable resources include:Provider handbooksClaims forms and submission tipsCompliance informationPharmacy directoryMedication formularyServices/medications requiring prior authorizationProvider network informationCMS Best Available Evidence policyLIS (Low Income Subsidy) ProgramClinical and administrative formsOnline provider education resourcesAnswers to frequently asked questions (FAQs)Access to Interpretive and Translation Services47Provider Orientation2014
Secure Provider PortalVisit the secure provider portal to access member care coordination informationat: www.magellancompletecareoffl.comMember Profiles Demographic Information Recent Medications Condition and Diagnoses Recent Authorizations Recent Claims48Provider Orientation2014Health Risk AssessmentResults Living Situation Hospital/Office Visit History Substance Use History Lab Results Vitals Social Activity Physical Activity Preventative Test History Chronic Conditions HistoryCare Coordination Tools Care Coordination Plan (CCP) Continuity of Care Document Ability to upload documents
Confidentiality Statement for ProvidersThe information presented in this presentation is confidential and expected to be used solely in support of thedelivery of services to Magellan members. By receipt of this presentation, each recipient agrees that theinformation contained herein will be kept confidential and that the information will not be photocopied,reproduced, or distributed to or disclosed to others at any time without the prior written consent of MagellanHealth Services, Inc.*If the presentation includes legal information (e.g., an explanation of parity or HIPAA), add this: Theinformation contained in this presentation is intended for educational purposes only and should not beconsidered legal advice. Recipients are encouraged to obtain legal guidance from their own legal advisors.49Provider Orientation2014
THANK YOU FOR ATTENDINGPLEASE COMPLETE YOURMAGELLAN COMPLETE CAREPROVIDER ORIENTATION SURVEY
Providers Initiates Credentialing Process Processes signed agreements . care services to our members through Magellan Complete Care of Florida affiliated providers. 13 Provider Orientation 2014 . MCCFL: Addressing Barriers to Care . – DentaQuest – Vision – Florida E