Transcription
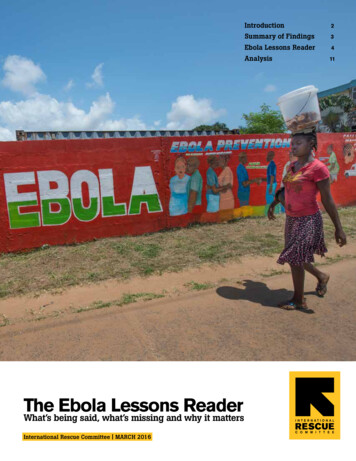
Introduction2Summary of Findings3Ebola Lessons Reader4AnalysisTheEbolaLessonsReaderWhat’s being said, what’s missing and why it mattersInternational Rescue Committee MARCH 201611
IntroductionA comprehensive review of Ebola reports offer valuable solutions, but they also perpetuateproblems by ignoring fundamental realities.The weaknesses of the global response to Ebola in WestAfrica from 2014 to 2016 not only cost tens of thousands of lives; it also hurt the credibility and confidenceof the global health community. So it was encouragingthat universities, think-tanks, the World Health Organization and other institutions took time to explore what wentwrong and how we can all do better.The resulting reports contain valuable, actionable insights. But collectively, their impact falls short of whatcould have been.METHODReport AnalysisWe have selected reflections from key actors involved inthe Ebola response. Our selection includes representatives from academia, think-tanks, NGOs, donors and theUnited Nations. We identified specific top-line recommendations assigned to actors and consolidated similarobservations. Pages 4-9 include our review.Bill Gates. The Next Epidemic – Lessons from Ebola. NewEngland Journal of Medicine 2015. April 9, 2015.World Health Organization. Ebola Interim AssessmentPanel “Stocking Report.” July 2015.Secondly, and more seriously, these reports reflect a persistent weakness of the global conversation about healthsystems: the erasing of politics. This includes the politicsof poor, post-conflict countries, but also the politics of theUN, NGOs and the international aid world. These failuresset the stage for a small Ebola outbreak to evolve into acatastrophic epidemic. The failure to anticipate and adaptto political realities then hobbled the response effort.Overseas Development Institute. Humanitarian PolicyGroup Working Paper. The Ebola Response in West Africa:Exposing the politics and culture of international aid. July10, 2015.The reports—with the notable exception of the workingpaper by the Overseas Development Institute—perpetuate a simplified narrative of the Ebola epidemic. Itfocuses disproportionately on the top levels of the WorldHealth Organization, while giving little to no scrutiny toother key issues and a complex ecosystem of playersthat carried out the bulk of the response.Council on Foreign Relations. Lessons Learned After theEbola Crisis - Darryl G. Behrman Lecture on Africa Policywith Thomas Frieden. November 24, 2015.Thousands of staff of the International Rescue Committee (IRC) participated in the Ebola response in SierraLeone and Liberia, working with everyone from topdecision-makers in WHO to front-line health workers andEbola patients. We reviewed these reports with theseresponders in mind, the vast majority of them citizensof the affected countries. We owe it to them, and to thetens of thousands of people directly affected, to highlightthe realities of the response that are in danger of beingforgotten. We also owe it to the present and future generations that will be faced with the next deadly infectiousdisease epidemic.We chose to respond to the current reports rather thanto start a new conversation. We want to build on thestrong points of these reports and to fill in critical gaps.What’s agreed upon and what’s missing? What shouldthe global community be doing more of or differently?2First, the sheer number and diversity of documentsthreaten to diffuse, rather than intensify, the focus on keyissues. Similar recommendations, articulated differently,risk making consensus sound like cacophony.The Ebola Lessons ReaderTony Blair Africa Governance Initiative. State ofEmergency: How Government Fought Ebola. July 10, 2015.The report of the Harvard-LSHTM Independent Panelon the Global Response to Ebola. Will Ebola change thegame? Ten essential reforms before the next pandemic. TheLancet. November 22, 2015.Médecins Sans Frontières. Epidemics as NeglectedEmergencies. November 25, 2015.Our aim is to make our shared goal of “never again” lesslikely to remain a well-placed intention and more likely tobecome a reality.
Summary of FindingsThe reports we reviewed had strong insight and numerous — 74, by our count — recommendations, many ofwhich are generally agreed upon. We have chosen to focus our attention on key issues that were not addressed.All eyes on the World Health OrganizationThe reviewed reports intensely scrutinize the WorldHealth Organization’s role and performance but fail toaddress basic questions about WHO’s mandate. Mostof the reports assume, in both their diagnosis and theirprescriptions, that WHO is and should be an operationalagency, rather than a norm-setting, coordinating agency.In reality, there are questions about whether it is feasiblefor WHO to be operational at a large scale, even withsignificant reforms. Another weakness of the reflectionsis a focus on the upper tier of the institution. There isalmost no attention given to practices throughout theorganization, such as those related to human resources,which heavily affect WHO’s performance in epidemics.The various high-level committees and oversight bodiesbeing proposed are unlikely to impact these practices.Few eyes on anyone elseThe reports give little scrutiny to other actors who provided the bulk of the response. While the reports primarilyfocus on WHO, other actors — including other UnitedNations agencies, NGOs, local communities and governments, militaries, donors, health workers and governmental public health agencies — played enormous roles,whether in people deployed, cases detected, technicalsupport, coordination, bodies buried or money spent.Their strengths and weaknesses will determine howeffectively we avert the next tragedy.Politics big and smallCollectively, the reports pay inadequate attention to thepolitics of the countries affected and of the internationalresponse. Ebola raised important questions, but missedthe key one: not what governments or aid actors sayor say they are going to do, but what people hear andwhat they do. This is what we call the politics of theresponse. For example, the reports focus on the delayof the response, but overlook the fact that governmentsand other actors were beginning large-scale effortsto respond and educate the public as early as April2014. One of the reasons that these early efforts failedis because the public in affected areas did not trustthe messengers. The reasons for this mistrust arecomplex, involving past and current sins, and political.Alternatively, successes against Ebola—and why theepidemic did not cost hundreds of thousands of lives, asexperts feared at one point—were in large part thanksto actors who took into account political realities andcultural sensitivity, particularly around activities likecommunity engagement and burials. These dimensionsare glossed over in most of the reports. Similarly, severalof the reports recommend health system strengthening,treating the issue as a technical one. Unmentioned arerelevant political realities: weaknesses in governance,unpaid health workers and a decade of health systemstrengthening as an apolitical exercise. Mixing politicsinto public health makes for uncomfortable conversation,but we can’t prevent another catastrophe without havingthat conversation.ANALYSIS OF EBOLA REFLECTIONS: WHO WAS THE FOCUS?Challenges facing the governments of the affected countries were highly noted in the reviewed documents, but mostcritiques focused on technical weaknesses rather than politics or mistrust. Proposed solutions focused on external actors.Altogether, critiques and solutions tended to focus on the World Health Organization.WHOOTHER SALLCRITIQUESSOLUTIONS0%50%The Ebola Lessons Reader 3
THE EBOLA LESSONS READERWHOOTHER UNAGENCIESAFFECTEDGOV’TSDATA,RESEARCH RVATIONSRELATED RECOMMENDATIONSWHOWHO did not have the skilled human resources or capacity to respond to the outbreak.WHO needs improved governance and leadership.WHO should be made fit for emergency response.2,5An independent UN Accountability Commission shouldbe created to do system-wide assessments of worldwide responses to major disease outbreaks.5WHO should be appropriately financed.1,2,5Gov’ts, in exchange for successful reforms, shouldfinance most of the budget with untied funds in a newdeal for a more focused WHO.2,5WHO was overruled by politics, compromising its ability toalert the global community.ALLOUTSTANDING QUESTIONS1,2,5,6WHO should develop a dedicated center for outbreakresponse with strong technical capacity, a protectedbudget and clear lines of accountability.5WHO was not financed to respond to the epidemic.DONORSIs the WHO supposed to be an implementer, a coordinator, a technical leader, or all of the above?Why did a new coordinating mechanism, the UN Missionfor Ebola Emergency Response, have to be set up inSeptember 2014? Was it because the WHO faceddifficulty hiring the right country representatives? Was itbecause the Ebola epidemic should have been immediately treated differently than a health emergency?Can the WHO improve feedback systems to ensure thatfront-line staff are heard and able to make decisions?(See p.11)WHO country-level representatives must have independence and full support.2,7WHO needs a politically protected Standing EmergencyCommittee, which will make declarations.5The Global Health Committee, as part of the UN Security Council, should expedite high-level leadership andelevate political attention to health issues.5Other UNagencies1.2.3.4.4UNMEER was unsuccessful.UNMEER is not the appropriate model mechanism formanaging future large-scale health emergencies.2Bill Gates. The Next Epidemic – Lessons from Ebola. New England Journal of Medicine 2015. April 9, 2015.World Health Organization. Ebola Interim Assessment Panel “Stocking Report.” July 2015.Tony Blair Africa Governance Initiative. State of Emergency: How Government Fought Ebola. July 10, 2015.Overseas Development Institute. HPG Working Paper. The Ebola Response in West Africa: Exposing the politics and cultureof international aid. July 10, 2015.The Ebola Lessons Reader5.6.7.Why was there little to no mention of UNICEF or WFP?(See p.12)The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Will Ebola change the game? Tenessential reforms before the next pandemic. The Lancet. November 22, 2015.Médecins Sans Frontières. Epidemics as Neglected Emergencies. November 25, 2015.Council on Foreign Relations. Lessons Learned After the Ebola Crisis - Darryl G. Behrman Lecture on Africa Policy withThomas Frieden. November 24, 2015.
THE EBOLA LESSONS READERWHOOTHER UNAGENCIESAFFECTEDGOV’TSDATA,RESEARCH QUES/OBSERVATIONSRELATED RECOMMENDATIONSOUTSTANDING QUESTIONSAffectedGovt’sGovernments did not support or enable early warningand detection.WHO needs to incentivize countries to report publichealth risks, i.e. financing mechanisms, lists of countriesthat delay.2,5How can we make International Health Regulations areality? Meeting these regulations will require sustaineddonor funding until governments have sufficient taxbases and functioning accountability mechanisms. Currently, there are no obligations for donors to help poorercountries meet these obligations.WHO members must adhere to the International HealthRegulations (IHR).2,7WHO must improve accountability for countries to identify/As far as IHR, what is or is not currently working instop threats and improve assistance to those that don’t.7countries? For example, we recognize that detection andWHO should cost, and World Bank should finance, a plan response is particularly difficult in low-resource areas.for all countries to develop IHR capacities.2Can we target such areas and determine the buildingblocks and costs needed to improve it?Gov’ts facing an outbreak must put developmental priorities second to saving lives and preventing the spread ofdisease.6Governments required strong political leadership withclear accountability to the people of the country.Gov’ts must put top people in charge, assume responsibility and be seen leading.3Aid organizations should support effective managementsystems that allow gov’ts to make the right decisions.3Governments lacked human, financial or material resources.The global community must mobilize adequate externalsupport for poorer countries.5,7Gov’ts need to demand what is needed from the international community and then use all resources effectively.3A list of necessary supplies to stop an epidemic couldbe developed, and experts could determine which itemswould need to be stockpiled/subject to commandeering.1Are politics a taboo in public health? How did thepolitical economy, both of the affected countries and theinternational global health community, positively and negatively impact the response? (See p.14-15)Why hasn’t a global strategy yet been proposed to fundthese capacities? Where can we strengthen existingresources and mechanisms? Examples of such mechanisms include distribution networks and stockpiles forvaccinations and networks of community health workers.Can existing resources be rationed more effectivelythrough harmonizing structures like consortia?All countries should commit to managing a pool of volunteers in the case of the next epidemic.1All countries could identify trained military resources thatwould be available for epidemics.11.2.3.4.5Bill Gates. The Next Epidemic – Lessons from Ebola. New England Journal of Medicine 2015. April 9, 2015.World Health Organization. Ebola Interim Assessment Panel “Stocking Report.” July 2015.Tony Blair Africa Governance Initiative. State of Emergency: How Government Fought Ebola. July 10, 2015.Overseas Development Institute. HPG Working Paper. The Ebola Response in West Africa: Exposing the politics and cultureof international aid. July 10, 2015.The Ebola Lessons Reader5.6.7.The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Will Ebola change the game? Tenessential reforms before the next pandemic. The Lancet. November 22, 2015.Médecins Sans Frontières. Epidemics as Neglected Emergencies. November 25, 2015.Council on Foreign Relations. Lessons Learned After the Ebola Crisis - Darryl G. Behrman Lecture on Africa Policy withThomas Frieden. November 24, 2015.
THE EBOLA LESSONS READERWHOOTHER UNAGENCIESAFFECTEDGOV’TSDATA,RESEARCH S/OBSERVATIONSRELATED RECOMMENDATIONSOUTSTANDING QUESTIONSAffectedGov’tsGovernments were susceptible, and unable to respond, toEbola due to weak health care systems.Resources need to focus on strengthening healthsystems in low- and middle-income countries for normalsituations and epidemics.1,5,6,7Is it realistic for an improved, but still weak, health systemto handle a lethal infectious disease that challengedfar more wealthy and established systems? Can healthsystems be improved to the required extent withoutaddressing weaknesses in governance? (See p.14-15)The int’l community must ensure that gov’ts invest indetection and response capacities and mobilize externalsupport to supplement efforts in poorer countries.5,6Donors must provide adequate resources to build effective emergency response systems as part of efforts tostrengthen medical infrastructure.6Recovery plans should be contingent on the ability ofUN agencies, NGOs, donors and governments to articulate how they will build health systems differently.4Int’l institutions such as the WHO must target this issue,i.e. financial investments and hands-on support.6Aid actors should help national governments with limitedcapacity to translate contingency plans into reality.6Gov’ts must agree to regular, independent, externalassessment of their core capacities.5Gov’ts must work collaboratively with int’l partners.3Building the technical capacities of health cannotoverlook other targets of capacity, such as politics andpower.41.2.3.4.6ALLBill Gates. The Next Epidemic – Lessons from Ebola. New England Journal of Medicine 2015. April 9, 2015.World Health Organization. Ebola Interim Assessment Panel “Stocking Report.” July 2015.Tony Blair Africa Governance Initiative. State of Emergency: How Government Fought Ebola. July 10, 2015.Overseas Development Institute. HPG Working Paper. The Ebola Response in West Africa: Exposing the politics and cultureof international aid. July 10, 2015.The Ebola Lessons Reader5.6.7.The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Will Ebola change the game? Tenessential reforms before the next pandemic. The Lancet. November 22, 2015.Médecins Sans Frontières. Epidemics as Neglected Emergencies. November 25, 2015.Council on Foreign Relations. Lessons Learned After the Ebola Crisis - Darryl G. Behrman Lecture on Africa Policy withThomas Frieden. November 24, 2015.
THE EBOLA LESSONS READERWHOOTHER UNAGENCIESAFFECTEDGOV’TSDATA,RESEARCH S/OBSERVATIONSRELATED RECOMMENDATIONSNGOsAid organizations failed to acknowledge that context andpolitics mattered for seemingly technical aspects of theresponse.Aid organizations must better understand the culture and Do NGOs fail to adequately consider politics in publicpolitical context for technical aspects of the response.3health programs? (See p.14-15)NGOs coordinated poorly, whether amongst themselvesor with the affected governments.NGOs should support government structures instead ofcreating their own.3NGOs already working in countries are slow to shift from Aid organizations that pledge themselves as emergencydevelopmental approach to an emergency. Their relation- responders need to ensure they have the capacity torapidly deliver services i.e. clinical care.3,6ships with national governments make them less willingto highlight epidemics.NGOs need to be clear about what they can and cannotdo.3OUTSTANDING QUESTIONSIs there too little scrutiny of NGOs and their performance? (See p.12)How did NGOs perform, beyond the delivery of clinicalcare? What difference did having long-term roots inthe countries make? What crucial roles did local NGOstaff play? What advantages did NGOs have over otheractors? (See p.12)Int’l actors in the face of an outbreak need to place developmental priorities second to saving lives and preventing the spread of outbreaks.6NGOs need to be flexible throughout the course of anepidemic to respond to evolving needs.3NGOs need to examine the role of capacity, fear, riskand duty of care within their organizations and mitigatethem.41.2.3.4.7ALLBill Gates. The Next Epidemic – Lessons from Ebola. New England Journal of Medicine 2015. April 9, 2015.World Health Organization. Ebola Interim Assessment Panel “Stocking Report.” July 2015.Tony Blair Africa Governance Initiative. State of Emergency: How Government Fought Ebola. July 10, 2015.Overseas Development Institute. HPG Working Paper. The Ebola Response in West Africa: Exposing the politics and cultureof international aid. July 10, 2015.The Ebola Lessons Reader5.6.7.The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Will Ebola change the game? Tenessential reforms before the next pandemic. The Lancet. November 22, 2015.Médecins Sans Frontières. Epidemics as Neglected Emergencies. November 25, 2015.Council on Foreign Relations. Lessons Learned After the Ebola Crisis - Darryl G. Behrman Lecture on Africa Policy withThomas Frieden. November 24, 2015.
THE EBOLA LESSONS READERWHOOTHER UNAGENCIESAFFECTEDGOV’TSDATA,RESEARCH QUES/OBSERVATIONSRELATED RECOMMENDATIONSOUTSTANDING QUESTIONSData,Research &DevelopmentReliable systems for sharing epidemiological, genomic,and clinical data were not established during the Ebolaoutbreak.Gov’ts, the scientific research community, industry, andNGOs must develop a framework to enable, accelerate,govern and ensure access to R&D.1,5Did the aim for perfect data compromise the timelinessof the response? Should more focus be on working solutions, like minimum datasets? Could the WHO establishrapidly usable and deployable systems for data sharingduring emerging outbreaks? This could include legalagreements, data formats, minimum datasets, standardoperating procedures and baseline standards for ethicalreview.WHO should play a central convening role in R&D inemergencies.2Foundations and tech companies could build an instantlyaccessible digital database.1There was no process for developing accurate or adaptable diagnostic tests, drugs and vaccine platforms. Private sector organizations do not have incentives to shiftresources away from more commercially viable projectsto work on these tools.Regulatory pathways for developing new tools and approaches should be clarified.1Stockpiles or manufacturing capacity for therapies thatmight be effective in an epidemic should be established.1Can organizations be assigned to establish protocolsand ethical parameters for testing drugs and vaccines,when needed?Research funders should establish a financing facilityfor outbreak-relevant drugs, vaccines, diagnostics andnon-pharmaceutical supplies.5OutsideGov’tsOutside governments established unnecessary tradebans and travel restrictions that restricted the movementof humanitarian workers and supplies.The deployment of international military forces securitized the response.Incentives should be strengthened for science-basedjustifications for trade and travel restrictions.2,5Independent flight and medevac capacity should beestablished.4How can the media assist? Strong media endorsementof recommendations, and restraint from exacerbatingfear, is critical to ensuring free movement of humanitarian workers and supplies.More attention is needed to the role of the security sector Where did the military do good and where did they doin health emergencies.4harm? (See p.12)Military support for emergencies must be under civiliancontrol.41.2.3.4.8Bill Gates. The Next Epidemic – Lessons from Ebola. New England Journal of Medicine 2015. April 9, 2015.World Health Organization. Ebola Interim Assessment Panel “Stocking Report.” July 2015.Tony Blair Africa Governance Initiative. State of Emergency: How Government Fought Ebola. July 10, 2015.Overseas Development Institute. HPG Working Paper. The Ebola Response in West Africa: Exposing the politics and cultureof international aid. July 10, 2015.The Ebola Lessons Reader5.6.7.The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Will Ebola change the game? Tenessential reforms before the next pandemic. The Lancet. November 22, 2015.Médecins Sans Frontières. Epidemics as Neglected Emergencies. November 25, 2015.Council on Foreign Relations. Lessons Learned After the Ebola Crisis - Darryl G. Behrman Lecture on Africa Policy withThomas Frieden. November 24, 2015.
THE EBOLA LESSONS READERWHOOTHER UNAGENCIESAFFECTEDGOV’TSDATA,RESEARCH QUES/OBSERVATIONSRELATED RECOMMENDATIONSOUTSTANDING QUESTIONSDonorsDonors allocated funding inflexibly and drove their ownpriorities.Donors should incorporate flexibility into funding mechanisms and contracts.4How did some key donors demonstrate flexibility? Howdid human resources decisions help their effectiveness?(See p.13)Donors severely delayed the disbursement of funding.Donors must develop faster and clearer mechanisms torelease funds in an emergency.6Are there new mechanisms for rapid disbursement torespond to the next epidemic?Top-down communication sidelined the communitieswhose engagement was essential.WHO and partners must ensure that appropriatecommunity engagement is a core function in a healthemergency.2Is effective community engagement possible withoutdeep understanding of the political context and origins ofmistrust? (See p.14-15)AllAnthropological engagement will need to include actionable solutions and recommendations that foster moreculturally acceptable messages and measures.4The response suffered from the lack of an effectivesystems approach that understood and coordinated allcomponents of the response.Systems must be improved through clearly defined roles,objectives and accountability of international partnersand governments.1,3Systems should include mechanisms for information tobe collected and shared; ways for issues to be escalated; and consistent opportunities for experts to engagedecision makers.3The UN and WHO should explore how to strengthen theWHO’s capacity, including which parts of the processit should lead and which should be led by others (i.eWorld Bank, G7 countries, NATO). The final arrangementshould include a reserve corps of experts with the rangeof skills needed in an epidemic.11.2.3.4.9Bill Gates. The Next Epidemic – Lessons from Ebola. New England Journal of Medicine 2015. April 9, 2015.World Health Organization. Ebola Interim Assessment Panel “Stocking Report.” July 2015.Tony Blair Africa Governance Initiative. State of Emergency: How Government Fought Ebola. July 10, 2015.Overseas Development Institute. HPG Working Paper. The Ebola Response in West Africa: Exposing the politics and cultureof international aid. July 10, 2015.The Ebola Lessons Reader5.6.7.Most broadly, we believe that affected countries mustserve as the overall coordinators of action. The WHO andother UN agencies should focus on technical leadershipand setting norms. International and local organizationsshould, in alignment with the broader strategy set by thenational authorities, implement the response and be adequately funded to do so. We found that consortia servedas effective harmonizing structures to improve efficiency,effectiveness, speed and scale of NGO work.The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Will Ebola change the game? Tenessential reforms before the next pandemic. The Lancet. November 22, 2015.Médecins Sans Frontières. Epidemics as Neglected Emergencies. November 25, 2015.Council on Foreign Relations. Lessons Learned After the Ebola Crisis - Darryl G. Behrman Lecture on Africa Policy withThomas Frieden. November 24, 2015.
Road to Foya, where the Ebola virus first crossed into Liberia from Guinea, October 2014. Photo by Peter Biro / The IRC
AnalysisThe global community owes it to those affected by the Ebola epidemic — and those who willface various epidemics to come — to examine gaps in our collective learning.All eyes on the World Health OrganizationOne common point in all the reviewed reports is a focuson the failings of the World Health Organization (WHO).The errors mentioned most often are the delays ingrasping the severity of the epidemic and developing anadequate response. Several of the reports examined theinternational political issues behind those failures: thedifficulty of making public health decisions in the face ofpolitical pressures from WHO’s member states and theimpact of reduced and earmarked funding on WHO’scapacity to respond. The reports offer several solutionsto insulate some key mechanisms from these pressures,which include unrestricted funding and the creation ofdecision-making bodies that are more insulated from political pressures. Unfortunately, for all of this scrutiny, thereports don’t address confusion about WHO’s mandate.Many of the reports criticize WHO for its failure to mountan adequate response itself without addressing onecritical reality: WHO has never been an implementer oflarge-scale public health interventions. This understanding was crucial in this epidemic, as it will be for futureepidemics. Many WHO staff played important roles infighting the outbreak and began implementing in theearly part of the response out of necessity. But it wasMinistries of Health staff, along with local and international NGOs, that led the vast majority of implementation.This included communicating with the public, finding cases and contacts, treating patients and burying the deadsafely. Such activities require large numbers of staff,the ability to hire quickly and hold staff accountable forperformance, a flexible and rapid supply chain and experience with field operations. The WHO was not conceivedas an operational agency to carry out these functions.WHO’s value and strength at its best, and those of manyother UN agencies, actually lies in its authority to settechnical norms and lead coordination. It’s a role thatWHO has taken on, many times successfully, in areasfrom childhood diseases to nutrition, and during emergencies. Why, in this case, did WHO fail at coordinating,to the extent that an entirely different coordinating mechanism, the UN Mission for Ebola Emergency Response,had to be set up in September 2014? Was it because ofthe difficulty in hiring the right country representatives?Was it because Ebola was more than a health emergency? What can be done to improve WHO’s coordinatingrole in epidemics?The Ebola response should also raise questions aboutthe influence of the institution’s human resources practices. Does a para-governmental approach to humanresources, which includes lifetime tenure and generousbenefits, discourage appropriate risk-taking while providing limited accountability for poor performance? Thesequestions have not yet been answered.While the reports reflect many actionable solutions toimprove the WHO, they are disproportionately aimed atthe upper levels of the institution. Most of the reportsadvocate for new committees or other bodies at the toplevels of the WHO. These changes will not address acore problem common to the WHO, other UN agenciesand governments during the Ebola epidemic: the inabilityto get accurate information in real time and the absenceof feedback loops to inform leaders whether interventions were effective.These issues were exacerbated by a reliance on contractual and rotating deployments. Staff couldn’t stay longenough to sustain support for people on the front
THE EBOLA LESSONS READER 1. Bill Gates. The Next Epidemic – Lessons from Ebola. New England Journal of Medicine 2015. April 9, 2015. 2. World Health Organization. Ebola Interim Assessment Panel “Stocking Report.” July 2015. 3. Tony Blair Africa Governance Initiative. State of