Transcription
U P D A T EI N ENDOCRINOLOGYDear Colleagues,2I am pleased to share our latest edition of Update in Endocrinology! While the mission of our Division issteadfast, we continue to grow both in knowledge and expertise to better serve the clinical andacademic community.Using Telehealth to Transform theCare of Rural Veterans With Diabetes4Psychosocial Aspects of DiabetesManagement Across the Life Span6An Interesting Case of Ataxia and8Sex-Dependent Effect of SteroidOsteosclerotic Bone LesionsHormones on Neurodevelopment,Physiology, and Behavior10Department NewsOpen Faculty Positions: Director, Multidisciplinary Thyroid Center Academic Clinical Endocrinologists Academic Research FacultyFull descriptions and contact informationon back page.CME CreditDisclosures: Drs. Bandi, Challinor, Frahm,Helgeson, Kershaw, Korytkowski, and Mahmudreport no relationships with proprietary entitiesproducing health care goods and services.Instructions: To take the CME evaluation andreceive credit, please visit UPMCPhysicianResources.com/Endocrinology, and click onUPMC Update in Endocrinology Fall 2018.Accreditation Statement: The University ofPittsburgh School of Medicine is accredited bythe Accreditation Council for Continuing MedicalEducation (ACCME) to provide continuingmedical education for physicians. The Universityof Pittsburgh School of Medicine designates thisenduring material for a maximum of .5 AMA PRACategory 1 Credits . Each physician should onlyclaim credit commensurate with the extent oftheir participation in the activity. Other healthcare professionals are awarded .05 continuingeducation units (CEU), which are equivalentto .5 contact hours.Clinically, we continue to make great strides towards improving care of at-risk patients by providingtelehealth services to patients outside the reach of quality endocrine care. In this issue, Archana Bandi, MD,clinical co-leader of the Endocrine Telehealth Unit and director of Telehealth Services at the VeteransAdministration Pittsburgh Healthcare System (VAPHS), highlights our use of innovative telehealthprograms to transform the care of rural veterans with diabetes. Our endocrine fellows, Karla Detoya, MD,and Neha Karajgikar, MD, presented the positive impact of these programs on quality and cost ofdiabetes care at the 2018 Annual Sessions for the Endocrine Society and American Diabetes Association,resulting in a first place award at the 2018 Endocrine Society Presidential Poster Competition.Another way we are improving care of at-risk patients is by better understanding the impact oftransitions of care and relationships on clinical outcomes. Our clinical endocrinologists HussainMahmud, MD, and Mary Korytkowski, MD, in collaboration with Vicki Helgeson, PhD, professor ofPsychology at Carnegie Mellon University, discuss how these important psychosocial factors influencediabetes management across the lifespan.Given the large endocrine catchment area of UPMC, there is never a shortage of complex cases tochallenge our knowledge and expertise. In this issue, our fellow Mihaela Oprea, MD, and her mentor,Sue Challinor, MD, present an interesting case of ataxia and osteosclerotic bone lesions in a patientwith a longstanding history of central diabetes insipidus. Can you guess the diagnosis?We continue to stress the growth of our academic mission through recruitment and development of toptalent. In the last interval, we welcomed two young and very talented tenure-stream assistant professors,Sadeesh Ramakrishnan, DVM, PhD, and Bokai Zhu, PhD. In this issue, we also highlight the researchand career development of Krystle Frahm, PhD, a former postdoctoral scholar on our long-standingNIH T32 training grant, who has recently transitioned to faculty and received an NIH-funded K01 awardto understand sex-dependent effects of steroid hormones on neurodevelopment, physiology, andbehavior. Dr. Frahm recently received the 2018 Endocrine Society Early Investigators Award.We also celebrate many other interval accomplishments of our faculty and trainees. Sann Mon, MD,was promoted to chief of Endocrinology at UPMC McKeesport, where she won the Resident TeachingAward for the third year in a row. Our clinical and research fellows presented their scholarly work at the2018 Annual Sessions of the Endocrine Society and the American Diabetes Association, where severalwon awards as noted above. Likewise, several of our faculty were recently recognized as “Best Doctors,”both locally and nationally. Finally, we enjoyed celebrating with our colleagues, alumni, and friends atour 2018 ADA Annual Reception in Orlando, Florida. We hope to see you at our reception next year!If you would like to be a part of a division that rises to the challenge of providing the best of tomorrow’sendocrine care today, I look forward to hearing from you!Best wishes,Erin E. Kershaw, MDChief, Division of Endocrinology and MetabolismAffiliated with the University of Pittsburgh School of Medicine,UPMC Presbyterian Shadyside is ranked among America’sBest Hospitals by U.S. News & World Report.DIVISION OF ENDOCRINOLOGY AND METABOLISMInside This EditionFA L L 2 0 1 8
Using Telehealth to Transform the Careof Rural Veterans with Diabetes 2 U P DAT E I N E N D O C R I N O L O G Y“Thanks for coordinating care for myfather,” said Rachel, fighting back tearsin her eyes. Rachel is a single momand home health care nurse who hadaccompanied her father, Mr. Smith, to alocal VA clinic in rural Pennsylvania for avideo visit with an endocrinologist locatedover one hundred miles away at the VAPittsburgh Healthcare System (VAPHS).Mr. Smith, a World War II veteran, was83-years-old when his primary careprovider (PCP) from James E. VanZandt VA Medical Center in Altoona,Pennsylvania, first sought assistance froman endocrinologist for his poorly controlleddiabetes. Being the sole caregiver for hiselderly wife, Mr. Smith was unable to travelto Pitts burgh where the endocrinologyteam was located. He was, therefore,offered an initial electronic consultationand telephonic follow-up visits with anendocrinologist at the VAPHS. Theendocrinology team then offered himcontinuity of care via clinical videotele con ferencing, remote blood glucosemonitoring services, and co-managementof his diabetes with his PCP. This real-lifestory highlights the potential of emergingtechnologies and implementation ofnon-traditional collaborative care modelsin diabetes management. Approximately 30.3 million people in theUnited States carry a diagnosis of diabetes,making it the seventh leading cause ofdeath.1 Concurrent with the escalatingprevalence of diabetes, there is an increasingshortage of physicians and other providerswho are specifically trained to care forpatients with diabetes. According to theendocrinology workforce analysis commis sioned by the Endocrine Society in 2012,the shortage of adult endocrinologists isexpected to increase from 1,500 in 2012 to2,700 by 2025.2 Further exacerbating thisproblem, the 2017 National DiabetesStatistics Report produced by the Centersfor Disease Control and Prevention (CDC)indicates that diabetes is 17 percent moreprevalent in rural areas compared to urbanareas, and yet the majority of endocrin ologists serve metropolitan rather thanrural areas. Not surprisingly then, theaverage wait time for a non-urgent newpatient visit with an endocrinologist atthe time of the CDC study was 37 days.Clearly, there is a tremendous need for newmodels of diabetes care, particularly forpatients residing in rural areas.Telehealth has emerged as a solution forthese escalating challenges. While theterm telehealth and telemedicine areoften used interchangeably, telehealthencompasses a wide range of health caredelivery modalities, as well as healthadministrative options such as tumorboards and medical education. Tele medicine refers more specifically tomedical care delivery processes andincludes: 1) asynchronous modalities, suchas remote patient monitoring (RPM) andelectronic consultations (e-consults), or2) synchronous modalities, such as virtualvisits using clinical videoconferencingtechnology (CVT) or telephonic visits.Although telehealth implementationcontinues to face many challenges, patientsare becoming increasingly capable of,and receptive to, these models of care.According to the fact-sheet published inFebruary 2018 by the Pew Research Center,about three-fourths of U.S. adults own adesktop or laptop computer and nearlyhalf own tablet devices.3 Likewise, theproportion of people who own and routinelyuse smartphones has risen from 35 percentin 2011 to 77 percent in 2018.3 Additionally,The Associated Press-NORC Center forPublic Affairs recently conducted a surveyto evaluate attitudes toward telemedicineamong adults over the age of 40. Thissurvey revealed that 88 percent of thosesurveyed would be comfortable usingtelemedicine to receive care, with acomfort level of 87 percent for caregiversand 50 percent for patients.4In addition to the above, evidence supportingthe clinical and cost effectiveness oftelehealth services for diabetes is likewisegrowing. A systematic review of RPM ofstructured self-monitored blood glucoses(SMBG) and its impact on HbA1c showedthat the impact was most significant whencare providers incorporated specificpredefined elements (spanning education,structured SMBG, and feedback) andincorporated computer decision support.5RPM platforms for SMBG provide real-timesupport for improving quality of life (QOL),improving outcomes related to patientsatisfaction, and reducing ED visits andinpatient days of care.6The VAPHS has been providing telehealthdiabetes services for more than a decade.The VAPHS team recently presentedoutcomes data at the 2018 EndocrineSociety Annual Meeting and Expo7 inChicago, IL and the 2018 AmericanDiabetes Association Annual ScientificSessions in Orlando, FL.8 These datademonstrate that, compared to traditionalface-to-face visits, telephone-basede-consultation provides comparablereductions in A1c levels (from a baselineaverage of 10.1 percent to 8.9 percentat six months with sustained benefitsat 12 months), but was able to do so withsub stantially improved access to care(27 days sooner), reduced travel distances(431 fewer miles traveled), and reduced timeengaged in travel/care (9.4 hours less time).7These data demonstrate the potentialbenefits of telehealth in diabetes care.VAPHS is a hub location for specialty carefor veterans enrolled in the western halfof VISN-4 (Veterans Integrated ServiceNetwork) and serves veterans residing inupstate New York, western Pennsylvania,eastern Ohio, and adjoining West Virginiaand Maryland. The majority of theseveterans reside in rural areas and have ahigh prevalence of complex diseases,such as diabetes and obesity.
FA L L 2 0 1 8process efficiency for patients and providersalike. A well-designed telediabetes pro gramshould be nimble and have elements thatserve the unique needs of the populationsbeing served. Such programs will beincreasingly necessary as the gap betweenthe number of available endocrin ologistsand the patients requiring endocrine anddiabetes care continues to rise.References123456Technological advances and the innovativeapplication of telehealth hold promise intransforming care delivery and improvingD I V I S I O N O F E N D O C R I N O L O G Y A N D M E TA B O L I S M8 73Embedding CVT clinics as a part of thespecialty care services allows for continuouscare for stable yet complex needs ofveterans with diabetes who live morethan 50 miles away from the hub. Currently,CVT service at the VAPHS consists of fiveendocrine providers (three endocrinologistsand two nurse practitioners) who servefour remote hospitals and more than 15community-based outpatient clinics. Theseservices are available five half days perweek and serve more than 120 veteransper month. Such robust partnerships led tothe creation of a more specialized InsulinU-500 CVT clinic in Clarksburg, WestVirginia. Complexity of care related toconcentrated insulin results in a hugeburden on PCPs and puts veterans at riskof medication errors, often precipitatinga need for long-distance travel. For thisreason, an additional two half days permonth are dedicated specifically toveterans requiring Insulin U-500. In thisway, endocrinologists located at the hubcan provide direct care via remote teamsthat coordinate the visit and long-term care. Given this acute need, the endocrinologyservice at the VAPHS has undergone atransformation to improve access todiabetes care for veterans closer to theirhomes using a variety of telehealthstrategies. In addition to live, in-personconsultations and follow-up care,endocrinologists at the VAPHS offere-consults, CVT clinics, group telediabeteseducation, and RPM services for SMBG.Incorporation of RPM allows for safe therapymodification between appointments andfor special circumstances, such as beforesurgical procedures, following hospitaldischarge, and/or during steroid use orchemotherapy. Alert guidelines for RPMfor SMBG also are provided for hometelehealth coordinators. Such partnershipshave led to reliable care collaborationbetween primary care teams and eport.pdfVigersky RA, Fish L, Hogan P, Stewart A, Kutler S,Ladenson PW, McDermott M, Hupart KH. TheClinical Endocrinology Workforce: Current Statusand Future Projections of Supply and Demand. JClin Endocrinol Metab. 2014 Sep; 99(9): in-america-increasing-access-to-care/Greenwood DA, Young HM, Quinn CC.Telehealth Remote Monitoring SystematicReview: Structured Self-monitoring of BloodGlucose and Impact on A1c. J Diabetes Sci Technol.2014; 8(2): 378-389.Faruque LI, Wiebe N, Ehteshami-Afshar A, et al.Effect of Telemedicine on Glycated Hemoglobinin Diabetes: A Systematic Review and Metaanalysis of Randomized Trials. CMAJ: Can MedAssoc J. 2017; 189(9): E 341-E364.Detoya K, Karajgikar N, Beattie J, Lutz-McCain S,Bourdeaux-Kelly M, Bandi A, et al. Impact ofElectronic Consultation versus Face-to-faceEncounters on Glycemic Control among Veteranswith Type-2 Diabetes. Abstract presented at theEndo-2018-Endo Society Annual Meeting andExpo 2018, Chicago, IL. *1st Place in PresidentialPoster Competition.Karajgikar N, Detoya K, Beattie J, Lutz-McCain S,Boudreaux-Kelly M, Bandi A, et al. Comparison ofE-consults and face-to-face care on costs andglycemic control among veterans with type-2diabetes mellitus. Abstract presented at 78thScientific Sessions of the American DiabetesAssociation, Orlando, FL. Archana Bandi, MDClinical Director, Telehealth ServicesDirector, E-Consult ServicesDivision of EndocrinologyVA Pittsburgh Healthcare SystemClinical Assistant ProfessorDivision of Endocrinology and MetabolismUniversity of Pittsburgh
Psychosocial Aspects of Diabetes ManagementAcross the Life SpanDiabetes is an incredibly challengingdisease that not only affects those carryingthe diagnosis, but also their family, friends,and others with whom they share closerelationships. These psychosocial aspects ofdiabetes have the potential to dramaticallyinfluence the natural history of the diseasethroughout the lifespan, and yet thepsychosocial factors that most stronglyinfluence outcomes and the interventionsmost likely to improve these outcomesremain poorly understood. 4 U P DAT E I N E N D O C R I N O L O G Y To address these important and complexissues, UPMC endocrinologists havepartnered with Vicki Helgeson, PhD,professor of psychology, and her team ofinvestigators at Carnegie Mellon University(CMU). This collaboration arose almosttwo decades ago when the diabetescommunity recognized the multiplechallenges facing youth with type 1diabetes. Adolescence is a particularlyimportant time to study youth withdiabetes, as self-care behaviors andglycemic control have been observed todecline during this period of time. Thetransition through emerging adulthood isan understudied but important period, asmost youth experience multiple transitionsduring this developmental period, includingchanges in lifestyle (e.g., education,occupation, living situation), changes inhealth care, and shifting relationships withfamily members, friends, and intimateothers. Clinicians and investigators atUPMC and CMU realized the need toestablish working relationships withexperts representing the medical andpsychosocial aspects of care deliveryto better understand how young adultswith type 1 diabetes navigate thesetransitions while also assuming increasingresponsibility for their diabetes careand overall health.In order to study these transitions, youthwith type 1 diabetes and their nondiabeticpeers were recruited and followed until age27 in the Teen Health study, Transition Timesstudy, and Research on Emerging AdultsChanging Health (REACH) study. Theselongitudinal studies revealed that parentalinvolvement in diabetes was a criticaldeterminant of self-care behavior andglycemic control during adolescence —especially for older adolescents. Duringemerging adulthood, the relationship withparents remained an important influenceon health behaviors and psychologicalwell-being. Higher parental support in theyear after high school was associatedwith better adherence, fewer depressivesymptoms, and lower risk behaviors amongemerging adults with diabetes. In addition,parental support buffered the adverseassociation between peer conflict and poorglycemic control among young adults withdiabetes.2 When compared to healthycontrols, those with diabetes did not scorehigher on depressive symptoms, loneliness,or bulimic symptoms, but did report lowerlife satisfaction and lower life purpose overtime.3 An analysis of the transition from thepediatric health care system to the adulthealth care system showed that an earlytransition is associated with worse glycemiccontrol ,as well as a host of psychosocialvariables (lower social status, nonwhiterace, lower likelihood of pursuing collegeafter high school graduation, and lower levelsof parental involvement in their daily lives).4Because individuals with diabetes areexperiencing increasingly longer lifespans,it is imperative to understand how to usesupport resources to enhance diabetesmanagement and quality of life in adultpatients and their families. Self-managementof diabetes during adulthood (involvinggood adherence to medication regimensand behaviors that foster good metaboliccontrol) requires daily self-regulation ofone’s emotions, behaviors, and cognitionsin the face of daily stressful events dealingboth with one’s diabetes (highs and lows inblood glucose) and other domains of life(child-rearing problems, marital conflicts,problems at work, managing other chronicillnesses). Managing daily stress occurs inthe context of important social relationships,most importantly the romantic/maritalrelationship. Romantic partners are likely tobe most strongly affected by the person’sdiabetes and to most strongly influencehow the person with diabetes manages hisor her disease.To study the impact of the social environ ment on adults with type 1 diabetes, ourcollaborative team embarked upon theDiabetes Across Development In Couples(DiADIC) study, which adopted an adultlife-span perspective to examine thestressors that are linked to diabetesmanagement and distress during young,middle-aged, and older adulthood. Thefocus of this study was on the ways thatromantic partners may facilitate diabetesmanagement across time throughcommunal coping. As opposed to thepediatric and adolescent population, fewstudies have been performed to addresshow couples cope with type 1 diabetesduring adulthood. The focus on communalcoping involves appraisals by the personswith diabetes that the illness is shared (i.e.,use of relational language such as “it is ourdisease” rather than an individual’s disease)and collaborative coping efforts to managethe disease. The data collected throughinterviews, behavioral observations, andonline diary assessments has allowed ourinvestigative team to measure communalcoping, diabetes management, distress,stress, and executive function. The studyaim is to identify the daily stressorsexperienced by adults with type 1 diabetesthat are linked to poorer diabetes selfmanagement and distress, to examine thecollaborative processes that are associatedwith better diabetes management andlower levels of distress, and to examinewhether executive function abilitiesmodulate the relation of collaborativeprocesses to diabetes management anddistress. A total of 199 couples have beenrecruited in this study in collaboration withthe University of Utah. The investigatorsare currently in the midst of preparingmanuscripts for publication.
families. Intervention efforts should focuson cultivating emotional support, optimizingmore subtle forms of infor mational supportthat are acceptable to patients, andminimizing controlling behaviors.Program DirectorMary Korytkowski, MDProfessor of Medicine andDirector of Quality ImprovementVicki Helgeson, PhDDirector of Graduate StudiesProfessor of PsychologyCarnegie Mellon University EDM Fellowship AssociateD I V I S I O N O F E N D O C R I N O L O G Y A N D M E TA B O L I S MClinical Assistant Professor of Medicine Hussain Mahmud, MD5Helgeson VS, Reynolds KA, Siminerio L, EscobarO, Becker D. Parent and Adolescent Distributionof Responsibility for Diabetes Self-care: Links toHealth Outcomes. J Pediatric Psych. 2008;33(5): 497-508.2 Helgeson VS, Palladino DK, Reynolds KA, BeckerD, Escobar O, Siminerio L. Relationships andhealth among emerging adults with and withoutType 1 diabetes. Health Psychology. 2014; 33(10):1125–1133.3 Palladino DK, Helgeson VS, Reynolds KA,Becker DJ, Siminerio LM, Escobar O. Emergingadults with type 1 diabetes: A comparison topeers without diabetes. J Pediatric Psych. 2013;38(5): 506–517.4 Helgeson VS, Reynolds KA, Snyder PR,Palladino DK, Becker DJ, Siminerio L, Escobar O.Characterizing the transition from pediatric toadult care among emerging adults with Type 1diabetes. Diabetic Medicine. 2013; 30: 610–615.5 Van Vleet M, Helgeson VS, Seltman HJ,Korytkowski MT, Hausmann LRM. Anexamination of the communal coping processin couples coping with diabetes. J Soc PersonRel. 2018.6 Zajdel M, Helgeson VS, Seltman HJ, KorytkowskiMT, Hausmann LRM. Daily communal coping incouples with type 2 diabetes: Links to mood andself-care. Ann Behavioral Med. 2018; 52: 228-238.7 Helgeson VS, Mascatelli K, Seltman H,Korytkowski M, Hausmann LRM. Implicationsof Supportive and Unsupportive Behavior forCouples with Newly Diagnosed Diabetes. HealthPsychology. 2016; 35(10): 1047-1058.1 From an endocrinologist’s perspective,interdisciplinary collaboration withDr. Helgeson’s team to investigate thepsychosocial aspects of diabetes acrossthe lifespan has been very enlightening.It has given collaborating clinicalendocrinologists a unique perspectiveregarding the psychosocial needs of ourpatient population. This is nicely illustratedby a favorite anecdote from a patient whoreturned for an office visit a few monthsafter participating in the DiADIC study.His hemoglobin A1c had improved by over1 percent, which he ascribed to theinterviews conducted at Dr. Helgeson’s lab.He stated that the interview process madehim and his wife realize that they are in thistogether and need to deal with his diabetesas a team. Insights gleaned from thesestudies will reveal novel insights intohow addressing life stressors, improvingcoping skills, and recruiting others in keyrelationships with patients can improveglycemic control and diabetes outcomesamong our patients. Likewise, the academicenvironment at UPMC is a fertile environ ment for multidisciplinary collaborativerelationships between clinicians andresearchers to create new knowledgethat ultimately improves the health andwell-being of our patients.ReferencesFA L L 2 0 1 8A parallel study is also being conducted,titled Communal Health Interactions inCouples (CHOICE) study, and is lookingat communal coping and diabetesmanagement among adult couples, inwhich one person recently has beendiagnosed with type 2 diabetes, also isbeing conducted. A total of 207 patientswere recruited from the community whohad been diagnosed with type 2 diabeteswithin the past five years, were married orliving with a romantic partner, and whosepartner did not have diabetes. The teaminterviewed couples in person, conducted abehavioral observation of their coping, andhad them complete daily diaries for 14consecutive days. Through all of theseassessments, it was found that patientswho engage in communal coping havebetter psychological and health behavioroutcomes.5,6 In addition, patients who feltunderstood and cared for by their partnersreported a better mood and were morelikely to take care of themselves on a dailybasis, whereas patients whose partnerswere identified as being more controllingon a daily basis reported poorer mood.Furthermore, patients characterized byunmitigated communion (focus on andinvolvement with others to the exclusionof the self) were most affected by partnersupportive and unsupportive behavior.7Given the increasing prevalence of type 2diabetes in the United States and thecritical role that self-care behavior playsin preventing complications, these resultssuggest that early intervention effortsaimed at people who are newly diagnosedwith diabetes ought to target couples and
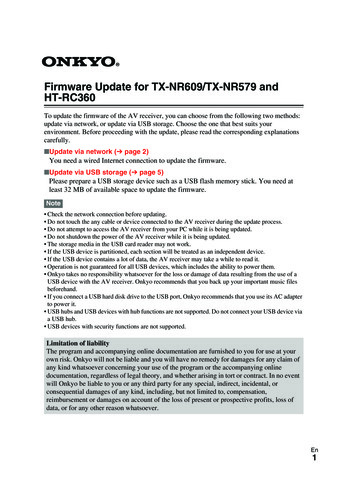
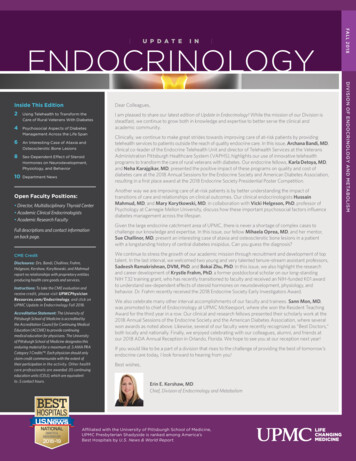
An Interesting Case of Ataxia and Osteosclerotic Bone Lesions in aPatient with a Longstanding History of Central Diabetes InsipidusCase PresentationA 47-year-old male with a prior history ofcentral diabetes insipidus (DI) presentedwith bone pain and ataxia.He was initially referred to an endocrin ologist in 1993 for evaluation of DI. Itwas concluded that he had lymphocyticinfundibulitis based on the finding of athickened pituitary stalk on MRI, whileCSF examination revealed no evidenceof infection or neoplastic disease. Hissymptoms of DI were controlled withDDAVP. He showed no other evidence ofanterior pituitary hormone deficiencies.Although subsequent imaging showedresolution of the pituitary stalk thickening,his DI never resolved. 6 U P DAT E I N E N D O C R I N O L O G Y In 2012, he was admitted to the hospital forevaluation of lethargy, confusion, impairedshort-term memory, and left lower extremityweakness. The altered mental statuswas transient and resolved five days later.A brain MRI was initially interpreted asunremarkable. A few months later, hedeveloped progressive gait instability, slurredspeech, and impaired motor coordination.He could not fully perform his workduties and lost his job. His brain MRIwas reexamined and showed evidenceof significant cerebellar midline atrophy.On exam, he exhibited horizontal nystag mus, dysarthria, gait impairment, andtruncal ataxia greater than limb ataxia.The etiology was unclear.He complained of chronic leg pain since2005, which became progressively moresevere. In 2018, osteosclerotic lesions werefound on x-ray of his tibia, for which heunderwent a bone biopsy with diagnosisof Paget’s disease (PD) at a communityhospital. His calcium, phosphate, 25hydroxy vitamin D, parathyroid hormone,and alkaline phosphatase were normal.Subsequently, he was seen at UPMCfor shoulder pain. X-rays noted lesionsof the pedicle of the left shoulder andpelvis, medullary sclerosis in the humeraldiaphysis (Figure 1), and symmetricallesions in the distal femur and tibiabilaterally. Bone scan and FDG-PET scanshowed increased activity in the lesions.A follow-up brain MRI revealed absenceof the posterior pituitary bright spot,enhancement along the proximal 7thand 8th nerve complex, disproportionatecerebellar atrophy, and enhancementalong the bilateral cerebellar folia that hadprogressed compared to the 2012 MRI. Arepeat right tibial biopsy at UPMC revealedmarrow infiltration with histiocytes (somewere lipid laden), fibrosis, and sclerosisof trabecular bone. The histiocytes werehighlighted by CD163, CD68, CD14, factorXIIIa, and fascin. A few scattered histiocyteswere BRAF V600E immunostain positive.The findings were consistent with adiagnosis of Erdheim-Chester disease(ECD). He will be treated with vemurafenib.Figure 1. Long segment of medullary sclerosis inthe right humeral diaphysis extending up to 15cm in length corresponding with increasedactivity on nuclear medicine bone scan. Nodefinite cortical thickening, periosteal reaction,erosive changes, or other aggressive features areseen. The appearance is compatible withosseous changes in Erdheim-Chester disease.DiscussionWe report a rare case of non-Langerhanscell histiocytosis originally described byJakob Erdheim and William Chester in1930.1 ECD is a rare type of hematopoieticneoplasm that is characterized by abnormalproliferation and infiltration of CD68positive, CD1a-/S100-negative foamyhistiocytes causing xanthogranulomatousinflammation in multiple organs. It is notgenetically inherited. Its incidence isunknown, but 500 cases have beenreported in the literature. Althoughdescribed in all age groups, it is mostcommon in adults with a mean age atdiagnosis of 53 years, with a slight malepredominance. The discovery of BRAFV600E mutation encountered in 50percent of cases is proof of an oncogenicprocess in this disorder.2 Mutations atV600E result in increased kinase activitythat enhances cell proliferation and survivalby activating the RAS/RAF/MEK/MAPKsignaling pathway. Additional mutations inNRAS (Q61R), KRAS, ARAF, PIK3CA, andMAP2K1 have been associated with ECD.3This disease can affect any organ system,but the most common clinical manifestationis multifocal cortical osteosclerotic lesionsof the diaphyseal and metaphyseal part oflong bones (95 percent). Pituitary/orbit(22 percent), central nervous system(41 percent), pulmonary (46 percent), andcardiovascular (57 percent) involvementhave been reported.4 DI is a feature thatoccurs early in the disease process in 25percent of patients. The involvement of thepituitary comm
Chief, Division of Endocrinology and Metabolism Interested candidates should send a cover letter, curriculum vitae, and contact information for three references to Erin E. Kershaw, MD, Chief of Endocrinology and Metabolism, care of Chelsea De