Transcription
Massachusetts Association of Medical Staff Services35th Annual Education ConferenceMassHealth / Executive Office of Health &Human ServicesMay 10, 2018Proprietary & Confidential1
Agenda1. Ordering, Referring and Prescribing Requirements2. MassHealth Payment and Care Delivery InnovationsProprietary & Confidential22
Ordering, Referring & Prescribing (ORP) RequirementsBackground ACA Section 6401 (b) States must require: All ordering or referring physicians and other professionals beenrolled under the State [Medicaid] Plan as a participatingprovider; and The NPI of any ordering or referring physician or otherprofessional be specified on any claim for payment that is basedon an order or referral of the physician or other professional These requirements were effective March 25, 2011. Final Rule (42 CFR455.410(b) and 42 CDR 455.440) was published in the FederalRegister on Feb. 2, 2011. Subregulatory guidance was given to stateson December 23, 2011 MassHealth is continuing its implementation efforts. In March 2016 andAugust 2017 we began providing informational messaging on certainimpacted claimsProprietary & Confidential33
ORP RequirementsProvider Types (including interns and residents in those providertypes) authorized to be included on a claim as the ordering, referringor prescribing provider and who must enroll as at least a nonbillingprovider Certified Nurse Midwife Certified Registered NurseAnesthetist Clinical Nurse Specialist Dentist Licensed IndependentClinical Social Worker Certified Nurse Practitioner Pharmacist (if authorized toprescribe) Physician Physician Assistant Podiatrist Psychiatric Clinical NurseSpecialist Psychologist OptometristFillable nonbilling provider applications and contracts are available on theMassHealth ation.htmlProprietary & Confidential44
ORP Requirements State law (Chapter 118 of the Acts of 2012 and Chapter 10 of the Acts of 2015)requires that these provider types must apply to enroll with MassHealth for at leastthe purposes of ORP (i.e., at least as a nonbilling provider) in order to obtain andmaintain state licensure, regardless of practice location (private practice, hospital,CHC, CMHC, etc.) The legislation applies to physician interns and residents but notother types of interns and residents. This law went into effect in November 2017 upon promulgation of MassHealthregulations on ORP enrollment and claims. These regulations: Define a new provider type – nonbilling providers Clarify that for Group Practices, only those providers that see MassHealthpatients must fill out a fully participating application. Providers in GroupPractices that do not see MassHealth patients may choose to fill out either afully participating application or a nonbilling application. Authorize MassHealth to deny claims that do not meet the ORP requirements. Specify requirements for making referrals in order to facilitate claimssubmission by billing providers.Proprietary & Confidential55
O&R Regulations – Where are we Today November 2017 license regulations became law which requires ORPeligible providers to be “known” to MassHealth (minimum as a non-billingO&R provider) in order to apply for or renew a license. Providers mustattest on their license applications that they have submitted anenrollment application to MassHealth. Individual license boards havebecame to implement this within their license board regulations.Professional TypeTotal MALicensedTotal “Known” toMassHealth% “Known” toMassHealthDentist (PT 10)Nurse Midwives (PT 08)7,2594805,21338572%80%Nurse Practitioners (PT 757%Licensed Independent Clinical Social Workers (PT 92)14,5933,78626%Total86,60155,23864%Optometrists (PT 02)Physician (PT 01)Podiatrists (PT 06)Psychologist (PT 05)Psych Nurse (PT 78)CRNA (PT 51)Physician Assistants (PT 39)Clinical Nurse Specialists (PT 57)Proprietary & Confidential66
ORP RequirementsThe services below must be ordered, referred or prescribed. O&Rrequirements apply to fee for service, crossover (where Medicarerequires O&R) and third party liability claims but not to claimssubmitted to MassHealth contracted managed care entities. Any service that requires aPCC referral Adult Day Health Adult Foster Care Durable Medical Equipment Eyeglasses Group Adult Foster Care Home Health Independent Living Independent Nurse Labs and Diagnostic TestsProprietary & Confidential Medications Orthotics Oxygen/RespiratoryEquipment Certain Personal CareAttendant services * Prosthetics Psychological Testing Therapy (PT, OT, ST) Transitional Living* T1019 billed by Fiscal Intermediary and T1020 billedby Transitional Living77
ORP Requirements On 2/26/16 MassHealth posted Provider Bulletin 259 for billing providersregarding the ordering, referring and prescribing provider requirements andthe implementation phases. On 2/18/18 MassHealth posted ProviderBulletin 274 with additional information regarding billing requirementsrelated to ordering/referring/prescribing. MassHealth is providing informational edits on most types of claimsimpacted by the ORP requirements. Impacted claims that do not meet allof the requirements listed below receive informational edits. These are theclaims that will deny once MassHealth begins to deny claims that do notmeet the requirements. The ORP provider’s NPI must be included on the claim The ORP provider must be enrolled with MassHealth, at least asa nonbilling provider The ORP provider must be one of the provider types listed onslide 4Proprietary & Confidential88
ORP Requirements Informational messages if the NPI of the ORP provider is notincluded on the claim:835 Electronic Remittance Advice (log into the POSC to see the applicable detailededit from the list below)HIPAA Claim Adjust Reason Code (CARC)206 – National Provider Identified – missingHIPAA Remark Adjust Reason Code (RARC)N265 – Missing/incomplete/invalid orderingprovider primary identifier POSC version of the remittance advice1080—Ordering Provider Required1081—NPI required for Ordering Provider1200—Referring Provider Required1201—NPI of Provider Required—HDR1202—NPI of Referring Provider Required 2—HDR *1204—NPI of Referring Provider Required 2—DTL * According to federal guidance, Ordering and Referring rules do not require a secondary referring provideridentifier on claims. However, there may be circumstances where the HIPAA V5010 ImplementationGuide situationally requires a second referring provider identifier. In those circumstances, if the secondreferring provider’s NPI is included on the claim, but that provider is not enrolled with MassHealth or is notan authorized ORP provider, relevant informational edits will be included on the remittance advice.Proprietary & Confidential99
ORP Requirements Informational messages if the ORP provider on the claim is not actively enrolledwith MassHealth, at least as a nonbilling provider: 835 Electronic Remittance Advice (log into the POSC to see the applicable detailed edit from the list below)HIPAA Claim Adjust Reason Code (CARC)208 – National Provider Identified –Not matched.HIPAA Remark Adjust Reason Code (RARC)N265 – Missing/incomplete/invalid orderingprovider primary identifier POSC version of the remittance advice1082—Ordering Provider NPI not on file1083—Mult Sak Prov Locs for Ordering Provider 1084—Ordering Provider not actively enrolled1205—Referring Provider NPI not on file – HDR1206—Referring Provider 2 NPI not on file – HDR *1207—Referring Provider NPI not on file – DTL1208—Referring Provider 2 NPI not on file – DTL *1209—Mult Sak Prov Locs for Referring Provider – HDR 1210—Mult Sak Prov Locs for Referring Provider 2 – HDR * 1211—Mult Sak Prov Locs for Referring Provider – DTL 1212—Mult Sak Prov Locs for Referring Provider 2 – DTL * 1213—Referring Provider not actively enrolled – HDR1214—Referring Provider 2 not actively enrolled – HDR *1215—Referring Provider not actively enrolled – DTL1216—Referring Provider 2 not actively enrolled – DTL *This informational edit indicates that there is more than one Provider ID/Service Location listed in the MassHealth MMIS for the NPIof the ORP provider. As a result, the MMIS is unable to confirm enrollment of the ORP provider. If you receive this message, pleasecontact the MassHealth Customer Service Center for assistance.Proprietary & Confidential1010
ORP Requirements Informational messages if the ORP provider on the claim is not an eligibleORP provider type: 835 Electronic Remittance Advice (log into the POSC to see the applicable detailed edit from the listbelow)HIPAA Claim Adjust Reason Code (CARC)183 – The referring provider is not eligible torefer the service billed .type/specialty thatHIPAA Remark Adjust Reason Code (RARC)N574 – Our records indicate the ordering/referring provider is of acannotorder or refer. Please verify that the claimordering/referring provider information is accurateor contact the order/referring provider.184 – The prescribing/ordering provider isnot eligible to prescribe/order the servicebilled.N265 – Missing/incomplete/invalid orderingprovider primary identifier184 – The prescribing/ordering provider isnot eligible to prescribe/order the servicebilled.N574 – Our records indicate the ordering/referring provider is of a type/specialty thatcannot order or refer. Please verify that the claimordering/referring provider information is accurateor contact the order/referring provider. POSC version of the remittance advice1085—Ordering Provider Not Authorized to Order Services1217—Referring Provider Not Authorized to Refer - HDR1218—Referring Provider 2 Not Authorized to Refer – HDR *1219—Referring Provider Not Authorized to Refer - DTL1220—Referring Provider 2 Not Authorized to Refer – DTL *Proprietary & Confidential1111
ORP Requirements Certain types of billing providers are currently receivingsignificant numbers of informational edits, particularly thosenoting that the NPI of the ORP provider is not on the claim. Acute Outpatient HospitalAdult Day HealthAdult Foster CareCertified IndependentLaboratoriesChiropractorsChronic Outpatient HospitalsCommunity Health CentersDurable Medical EquipmentEarly InterventionFiscal Intermediaries in thePersonal Care AttendantProgram Group Adult Foster Care Group PracticeOrganizations Home Care Home Health Agencies Hospital Licensed HealthCenters Pharmacies Renal Dialysis Clinics Special Programs Volume Purchaser(eyeglasses)Billing providers receiving these informational denial edits should updatetheir billing procedures to avoid future claims denials.Proprietary & Confidential1212
O&R Regulations – Where are we Today Informational Claim edit denials are still in place and no actual paymentdenials are happening. Many providers have updated their claimsystems to include the ORP provider’s NPI. However, many have notand MassHealth continues to see numerous edits, especially forservices that are requiring referrals.Proprietary & Confidential1313
ORP Requirements Billing Instructions: Enter the ORP NPI in the Referring Provider field if the claim is for a service that requires a PCC referral (such claims will alsocontinue to require the PCC referral number); or is for a laboratory service or a diagnostic testing service; or is submitted on an 837I or UB-04 (such claims only have aReferring Provider field) Enter the ORP NPI in the Ordering Provider field for all other impactedclaims for services listed on slide 7 Batch Claims – Report the Referring Provider in Loop 2310A forProfessional claims or Loop 2310F for Institutional claims and theOrdering Provider in Loop 2420E. Please adhere to ASCX12 HIPAAV5010 Implementation Guide regarding the inclusion of the referringand ordering provider Loops and Segments. POPS – Submitters should follow the instructions in the POPS BillingGuide related to populating prescriber informationProprietary & Confidential1414
ORP Requirements Direct Data Entry (DDE) Institutional (837I) ORP NPI location is Referring Provider field on the Billing andService Tab. Referring provider is allowed only at the header levelin DDE. If multiple referring providers apply to the claims, servicesfor each referring provider must be billed separately. Professional (837P) PCC Referral/Labs/Tests ORP NPI location is Referring Provider field on the Billingand Service Tab. Referring provider is allowed only at theheader level in DDE. If multiple referring providers apply tothe claims, services for each referring provider must be billedseparately. All other impacted services ORP NPI location is Ordering Provider Field on theProcedure Tab.Proprietary & Confidential1515
Questions?Proprietary & Confidential1616
Payment and Care Delivery Innovation(PCDI)Presented by – Stephen Cairns, Directorof Provider ServicesProprietary & Confidential1717
Important Member Choice DatesBelow are important dates for managed care eligible members with enrollments effective March 1, 2018Update:The fixed enrollmentperiod extended toJuly 1st11/13/17 – 2/28/18: During this time,members can choose to prospectivelyenroll in a new plan effective March 1, 201811/13/17-12/22/17Member Mailing3/1/18Start of Plan Selection PeriodMembers can change health plansfor any reason for 120 days 7/1/18Start of Fixed Enrollment PeriodMembers enrolled in an ACO orMCO can only change their healthplans for certain reasonsAfter March 1, 2018, a new managed care member’s Plan Selection Period will be the first 90 days after the effective date ofenrollment to a new Plan, and Fixed Enrollment will be the remaining 275 days of the year For example, a new managed care eligible member who enrolls into a new Plan effective 6/1/18, will bein their Plan Selection Period from 6/1/18 to 8/29/18, and their Fixed Enrollment Period from 8/30/18 to 5/31/19 All managed care members have a new plan selection and fixed enrollment period every year Member enrollment changes made during the Plan Selection Period will take 2 to 3 days to processProprietary & Confidential1818
New Service Area Exceptions ProcessEffective April 9, 2018, MassHealth is implementing a process toallow members, under certain specific circumstances, to join anAccountable Care Partnership Plan that does not cover the servicearea in which the member lives. MassHealth will allow current andfuture members to request a service area exception to enroll in anout-of-area Accountable Care Partnership Plan by contacting theMassHealth Customer Service Center.Service area exceptions may be granted for the following reasons: The member has an established relationship with a PCP whoparticipates in an Accountable Care Partnership Plan that does notcover the service area in which the member resides; The member is homeless and a specific Accountable CarePartnership Plan can better accommodate the member’s supportneeds; or The member’s enrollment in the Accountable Care PartnershipPlan significantly supports language, communication, or culturalneeds; specialized health care needs; or other accessibility needsProprietary & Confidential1919
Primary Care Participation and Exclusivity Primary care practices and ACO-participating PCPs will be exclusive totheir contracted ACO—they will exclusively provide primary care toMassHealth managed care members enrolled in their ACO. ACO-participating PCPs cannot participate as primary care providers inMCOs or the PCC Plan or any other ACO. This exclusivity is enforced at the practice or entity level rather than atthe individual doctor level. Exclusivity does not apply to other programs, such as MassHealth fee-forservice, Senior Care Options (SCO), One Care, or the Program of Allinclusive Care for the Elderly (PACE). PCPs can continue to provide services to members in the abovementioned plans including fee-for-service members regardless oftheir contracts with ACOs. PCPs who are also specialists can continue to provide specialty servicesacross managed care plans.Proprietary & Confidential2020
Specialist, Hospital, and Other Provider Participation Specialists, hospitals, and other providers may contract withmultiple health plans at the same time and can provide services tomembers in any of the health plans with whom they arecontracted. The managed care assignment of the member to anMCO, ACO, or PCC Plan is crucial for specialists to understand.This will ensure that specialists provide services to members ofplans that they are contracted with. A specialist may see MassHealth members enrolled with the PCCPlan or a Primary Care ACO if the specialist is a MassHealthparticipating provider. For members enrolled in an AccountableCare Partnership Plan or MCO, specialists will need to contractwith each of these health plans to provide services to membersenrolled in these plans. This information can be found in All Provider Bulletin 272.Proprietary & Confidential2121
Accountable Care Partnership Plans (Model A) A network of PCPs who have exclusivelypartnered with an MCO to use the MCO’sprovider network to provide integrated andcoordinated care for members Accountable Care Partnership Plans covera set of service areas where they willoperate. Members must live in the serviceareas covered by the ACO to enroll in thatplanPCP NetworkMCO ProviderNetwork MassHealth has contracted with13Accountable Care Partnership PlansProprietary & Confidential2222
Primary Care ACOs (Model B) A network of PCCs who contract directlywith MassHealth to provide integratedand coordinated care for members Primary Care ACOs work with theentire MassHealth provider networkof specialists and hospitals, andmay have certain providers in their“referral circle” that will not requirea MassHealth referral for the servicePCC Network Primary Care ACOs will use theMassachusetts Behavioral HealthPartnership (MBHP) for behavioralhealth servicesMassHealthProvider Network MassHealth has contracted with 3Primary Care ACO PlansProprietary & Confidential2323
MCO-Administered ACOs (Model C) A network of PCPs who may contractwith one or multiple MCOs, and use theMCO provider networks to provideintegrated and coordinated care formembers MCO-Administered ACOs are notpresented as an enrollment optionfor members because they will beattributed through their relevant MCOMCO Provider NetworkACO PCPNetwork There is one MCO-Administered ACO,Lahey Clinical Performance Network,which is participating with both MCOseffective March 1, 2018: Boston MedicalCenter (BMC) HealthNet Plan, and TuftsHealth TogetherProprietary & Confidential2424
MCOs and the PCC PlanIn addition to ACOs, members will continue to have the following managed care options effective March 1, 2018:Managed Care Organizations (MCOs) MCOs are health plans run by insurancecompanies that provide care through theirown provider network that includes PCPs,specialists, behavioral health providers, andhospitals There are two MCO options: Boston MedicalCenter (BMC) HealthNet Plan, and TuftsHealth TogetherAll Service Areas Southeast RegionBMC HealthNet Plan will operate statewide,and Tufts Health Together will operate inevery region except Southeast, MAPrimary Care Clinician (PCC) Plan The Primary Care Clinician (PCC) Plan is a statewide plan run by MassHealth that uses theMassHealth provider network Behavioral health services for the PCC Plan are provided by the Massachusetts Behavioral HealthPartnership (MBHP) Members must choose a PCC in order to enroll in a PCC PlanProprietary & Confidential2525
MassHealth Health Plan Options Effective March 1, 2018Accountable Care Partnership Plans (Model A)Be Healthy Partnership - Baystate Health Care Alliance with Health New EnglandBerkshire Fallon Health Collaborative - Health Collaborative of the Berkshires with Fallon HealthBMC HealthNet Plan Signature Alliance - Signature Healthcare with BMC HealthNet PlanBMC HealthNet Plan Community Alliance - Boston Accountable Care Organization with BMC HealthNet PlanBMC HealthNet Plan Mercy Alliance - Mercy Medical Center with BMC HealthNet PlanBMC HealthNet Plan Southcoast Alliance - Southcoast Health with BMC HealthNet PlanFallon 365 Care - Reliant Medical Group with Fallon HealthMy Care Family - Merrimack Valley ACO with Neighborhood Health Plan (NHP)Tufts Health Together with Atrius Health - Atrius Health with Tufts Health Plan (THP)Tufts Health Together with BIDCO - Beth Israel Deaconess Care Organization (BIDCO) with Tufts Health Plan (THP)Tufts Health Together with Boston Children's ACO – Boston Children’s ACO with Tufts Health Plan (THP)Tufts Health Together with CHA - Cambridge Health Alliance (CHA) with Tufts Health Plan (THP)Wellforce Care Plan - Wellforce with Fallon HealthMCOsMCO-Administered ACO (Model C)Boston Medical Center(BMC) HealthNet PlanLahey Clinical Performance Network(Participating with Boston Medical CenterHealthNet Plan and Tufts Health Together)Tufts Health TogetherProprietary & ConfidentialPCC PlanPrimary Care ACO Plans (Model B)Community Care Cooperative (C3)Primary careProviders inPartners HealthCare Choicethe MassHealthNetworkSteward Health Choice2626
Payer of Claims Effective March 1, 2018Plan TypePayer of ClaimsPCC PlanMassHealth for non-BH services(MBHP for BH services)Primary Care ACOMassHealth for non-BH services(MBHP for BH services)MCOMCO*MCO-Administered ACOMCO*Accountable Care Partnership PlanPartnership Plan**If an MCO or Accountable Care Partnership Plan uses a Behavioral Health (BH) vendor, providers may be paid through theBH vendor for BH services.Proprietary & Confidential2727
Continuity of Care (CoC)MassHealth is committed to working with all relevant parties to ensure continuity of care for the many members who are movingto new plans, whether they are going to or from an ACO Partnership Plan, a Primary Care ACO, an MCO, or the Primary CareClinician (PCC) Plan.Here are the most important things for you to know:Update:Continuity of care extended formedical care through May 31st. These changes apply to MassHealth managed care members (generally, this includes members under age 65 who do nothave another primary insurer, either commercial or Medicare, and are not in a long-term facility) All members have a minimum 30-day continuity of care period During the continuity of care period all existing prior authorizations for services and for provider referrals will be honored bythe member’s new plan. Members can continue to see their existing providers for at least 30 days, even if those providersare not in their new plan’s network Providers who are not in the new plan’s network must contact the new plan to make appropriate payment arrangements In some cases, the continuity of care period may be extended. For example, members who are pregnant can continueseeing their existing OB/GYN providers throughout their pregnancy and up to six weeks postpartum We are asking all plans, providers, and assisters to support members in receiving all needed health care services duringthis transition Members can contact their new plan now to let them know of any ongoing treatments or scheduled appointments Providers will be able to see new plan information in the MassHealth Eligibility Verification System (EVS) starting March 1.They can contact the new plan at that time for new authorization requests, or with any questions or concerns aboutproviding services MassHealth and all ACOs and MCOs have escalation protocols in place for continuity of care issues that may arisePlease make all efforts to ensure that members continue to have access to all needed health services during this transition.Proprietary & Confidential2828
Continuity of Care (CoC)MassHealth has created a Continuity of Care Homepage whichfeatures helpful information available to view and download for interestedparties regarding Continuity of Care through transitions to new managedcare arrangements. -care Continuity of Care Memo Continuity of Care FAQ'sThis information is also featured on the MassHealth Provider PCDIResources Web Page at roprietary & Confidential2929
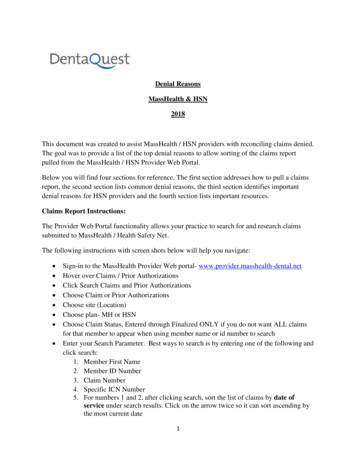
Eligibility Verification System (EVS) Providers should continue to check member enrollment and eligibility using EVS* on the ProviderOnline Service Center (POSC) Providers reduce the risk of denied claims by using EVS to verify member enrollment and eligibilityprior to providing services to MassHealth members There are two types of Restrictive Messages that appear on EVS: Eligibility Restrictive Messages (No Changes) Managed Care Data Restrictive Messages (Enhanced)The Managed Care Data Restrictive Messages have been enhanced to identify which type of health plana member is enrolled in, and their contact information for inquiries regarding: Billing (medical and behavioral health claims) Service authorizations (medical and behavioral health services) Behavioral Health vendors Visit the Provider PCDI Resources page at https://www.mass.gov/lists/provider-pcdi-resources to view and download theMassHealth Quick Reference Guide and screenshot examples of EVS codes and restrictive messages for all 2018managed care health plans. If you have questions about how to check a member’s eligibility, please refer to the Verify Member Eligibility Job Aid tolearn how to access and check member eligibility using EVS on the POSC(URL: ty)*Note: EVS only displays a member’s current eligibility, not future eligibility.Proprietary & Confidential3030
EVS – Eligibility Tab1. To verify thecoverage type amember has,click on theEligibility tab.2. Click on thehyperlink of theDate Range*entered fordetailsregarding themember’scoverage.*Note: EVS only displays a member’s current eligibility, not future eligibility.Proprietary & Confidential3131
Screenshot Examples of New EVS Restrictive Messages for 2018Managed Care Health Plans1. BeHealthy Partnership – Accountable Care Partnership PlanNote: EVS onlydisplays a member’scurrent eligibility, notfuture eligibility.Proprietary & Confidential3232
Common Questions If I am a specialist or hospital contracted with MassHealth can I see members enrolledwith a Primary Care ACO or PCC Plan?o Yes, Primary Care ACOs and the PCC Plan use the MassHealth fee‐for‐service (FFS) network ofspecialists and hospitals.o For more information please refer to the PCDI for Specialist Fact Sheet. Who is responsible for paying claims during the 30 day continuity of care period?o The plan that the member is enrolled with on the date of service is responsible for paying theclaim for the services rendered.o For more information please refer to the Continuity of Care Homepageo ��of‐careWho should providers contact about joining a plan?o Providers should contact the plan directly.o MassHealth has created a 2018 Health Plan Contact Matrix that lists the medical and behavioralhealth contact information, member ID card images, and web links for all 2018 MassHealthmanaged care health plans.o Visit the Provider PCDI Resources page to view and download this document and other helpfulresources.Proprietary & Confidential3333
MassHealth Dentist (PT 10) 7,259 5,213 72% Nurse Midwives (PT 08) 480 385 80% Nurse Practitioners (PT 17) 9,388 6,611 70% Optometrists (PT 02) 1,549 1,039 67% . eligible providers to be “known” to MassHealth (minimum as a non-billing O&R provider) in order to appl