Transcription
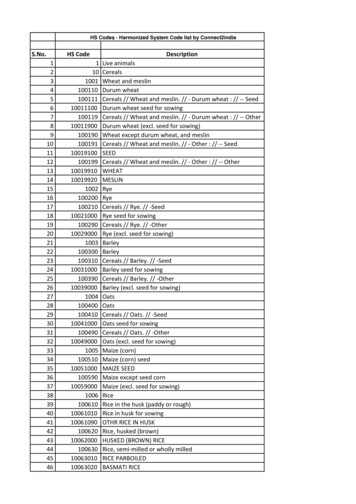
Denial ReasonsMassHealth & HSN2018This document was created to assist MassHealth / HSN providers with reconciling claims denied.The goal was to provide a list of the top denial reasons to allow sorting of the claims reportpulled from the MassHealth / HSN Provider Web Portal.Below you will find four sections for reference. The first section addresses how to pull a claimsreport, the second section lists common denial reasons, the third section identifies importantdenial reasons for HSN providers and the fourth section lists important resources.Claims Report Instructions:The Provider Web Portal functionality allows your practice to search for and research claimssubmitted to MassHealth / Health Safety Net.The following instructions with screen shots below will help you navigate: Sign-in to the MassHealth Provider Web portal- www.provider.masshealth-dental.netHover over Claims / Prior AuthorizationsClick Search Claims and Prior AuthorizationsChoose Claim or Prior AuthorizationsChoose site (Location)Choose plan- MH or HSNChoose Claim Status, Entered through Finalized ONLY if you do not want ALL claimsfor that member to appear when using member name or id number to searchEnter your Search Parameter. Best ways to search is by entering one of the following andclick search:1. Member First Name2. Member ID Number3. Claim Number4. Specific ICN Number5. For numbers 1 and 2, after clicking search, sort the list of claims by date ofservice under search results. Click on the arrow twice so it can sort ascending bythe most current date1
2
You will now have 2 options: The option of clicking on the individual claim number to see claim details, the ServiceLine Information and the Denial Processing Policies, if denied. (see below)3
You also have the option of Downloading the “Claim Report” or using the “PrinterFriendly Format”. *Note: Download all claims on each page before using the printerformat.Common Denial Reasons:Below is a list Common Denial Reasons you may see. Most of these denials can be eliminated byentering the claim on time and correctlty. Please refer to the Office Reference Manual located inthe Document Section of the Provider Web Portal to see a list of Covered MH codes and anyBenefit Limitaions associated with the codes being submitted.Denial Number20012007Denial DescriptionThe patient was covered on thedate(s) of service by anotherinsurance company which is theprimary carrier. After the primecarrier has determined itsliability, resubmit this claim witha copy of the prime carrier'sEOB.The primary insuranceinformation indicated isincomplete. Please submit a4Reconciliation StepsAfter the prime carrier hasdetermined its liability,resubmit this claim with acopy of the prime carrier'sEOB.Submit a primary EOBshowing the procedureslisted, other carrier
2016202020212022202920302035203620402068primary EOB showing theprocedures listed, other carrierpayment, other carrier name andpolicy number and dates ofservice. Please return this EOBwith the correct documentation tocomplete processing.This procedure has beensubmitted after the timely filinglimit.The required tooth number wasnot submitted for this procedurecode. Please submit a correctedclaim with the valid procedureand the valid tooth.The required tooth/quad/arch isinvalid, was not submitted, or isnot included in the member’sbenefit package for this procedurecode. Please refer to your ORMand resubmit a claim with theappropriate information.The required surface(s) is/areinvalid or missing for thisprocedure code. Please submit acorrected claim with the validprocedure and the validsurface(s).This procedure is a duplicate of aservice previously processed.Subscriber is not eligible forservices under this plan.Patient is not eligible for services;coverage is not active.Based on the informationsubmitted, we are unable to locatethis patient in our records. Pleaseverify the patient information.Service is not covered. Pleaserefer to your Office ReferenceManual for definition of coveredteeth/quad/arch, patient ages, andprocedure codes.Service requires priorauthorization. Prior authorizationrequest was found but has5payment, other carriername and policy numberand dates of service.Please return this EOBwith the correctdocumentation to completeprocessing.Resubmit with requiredtooth number.Resubmit the claim withthe requiredtooth/quad/arch.Resubmit with valid toothsurfaces.Verify the memberinformation submitted iscorrect.Verify to be sure that theright code / teeth / quad /arch and procedure codewas submitted.
20692070207120832086209921012209expired.Service requires priorauthorization. A priorauthorization request was foundbut has already applied to asubmitted service.Service requires priorauthorization. No priorauthorization is on file.The prior authorization matchingthis service was denied.Service exceeds maximumbenefit allowance.Service exceeds benefitallowance. Service is limited toone per lifetime per patient.Services provided by an Out-ofNetwork or Non-contractedprovider are not provided underthis benefit program.Service not allowed. Patienthistory record indicates tooth waspreviously extracted.Encounter rates are payable onlywhen submitted with theencounter code withcorresponding fee and at least onevalid dental procedure code. Youeither did not submit theencounter code with fee, anyother procedure codes or thesubmitted procedure code wasdenied.HSN Providers- Important Denial Reason:6Please check to be sure theright tooth number wassubmitted.If so, submit areconsideration includingall information relevant todocument the existence ofthe tooth prior toextraction for review.This denial reason willapply to code D9450.
While it is critical that all denials be reconciled, one core reason for denial is populated on claimswhere MassHealth was the primary that paid and due to the system requirements, a secondaryclaim for HSN was automatically generated and processed.Denial Number2040Denial DescriptionReconciliation StepsService is not covered. Pleaserefer to your Office ReferenceManual for definition of coveredteeth/quad/arch, patient ages, andprocedure codes.For HSN providers, this isthe core denial reason thatis utilized for claims thathave paid underMassHealth and therefore,will not be covered underHSN.Our recommendation is tofilter this denial reason tothe end of your reportsand reconcile thesesecondary to all otherdenials.Other Denial Reasons:20512104210921142116Member enrollment file indicatesother coverage maybe primary.Please submit with primary eob.Service does not meet benefitcriteria.Service denied due to appropriatecare review. Patient history doesnot support service.Sealants not allowed overrestorations.Service has been bundled withother procedure lines to a moreappropriate code. Restorationsperformed on multiple surfaceson the same tooth must be billedwith appropriate procedure code.7Resubmit with primary eobor termination letter
2146Service exceeds benefitallowance. Service is limited toone per date of service.Service exceeds benefitallowance. This service isallowed twice per calendar year.Group allows electronicsubmission only.Missing deductible anniversarydatePlease resubmit with a panorex ora full mouth series of x-rayslabeled with members full name,date film(s) taken and(mm/dd/yyyy), and identify thepatients left and right side.Per Dental Director review thedocumentation submitted doesnot demonstrate the need for theuse of fluoride.Please resubmit with bitewing xrays labeled with members fullname, date film(s) taken and(mm/dd/yyyy), and identify thepatients left and right side.217622502297319834543456Resubmit electronically.Resubmit with deductibleanniversary date.Resubmit with panorex orfull mouth series of xraysand label them.Resubmit with bitewing xrays and label them.Important ResourcesTo locate the MassHealth and HSN Office Reference Manual: Click on Document List on the Provider Web PortalSelect Office Reference Manual on the “File Detail Category” WindowIf your site is a HSN provider you will have both the HSN and MH ORMS available toopen8
9
Valuable documents, newsletters, forms, fee schedules and training documents can befound in the document section. Just click the Search button and all files will appear10
where MassHealth was the primary that paid and due to the system requirements, a secondary claim for HSN was automatically generated and processed. Denial Number Denial Description Reconciliation Steps . 2040 Service is not covered. Please refer to your Office Reference Manual for