Transcription
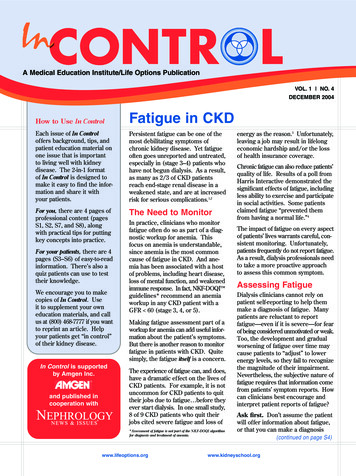
A Medical Education Institute/Life Options PublicationVOL. 1 NO. 4DECEMBER 2004How to UseIn ControlFatigue in CKDEach issue of In Controloffers background, tips, andpatient education material onone issue that is importantto living well with kidneydisease. The 2-in-1 formatof In Control is designed tomake it easy to find the information and share it withyour patients.Persistent fatigue can be one of themost debilitating symptoms ofchronic kidney disease. Yet fatigueoften goes unreported and untreated,especially in (stage 3–4) patients whohave not begun dialysis. As a result,as many as 2/3 of CKD patientsreach end-stage renal disease in aweakened state, and are at increasedrisk for serious complications.1,2For you, there are 4 pages ofThe Need to Monitorprofessional content (pagesS1, S2, S7, and S8), alongwith practical tips for puttingkey concepts into practice.For your patients, there are 4pages (S3–S6) of easy-to-readinformation. There’s also aquiz patients can use to testtheir knowledge.We encourage you to makecopies of In Control. Useit to supplement your owneducation materials, and callus at (800) 468-7777 if you wantto reprint an article. Helpyour patients get “in control”of their kidney disease.In Control is supportedby Amgen Inc.and published incooperation withIn practice, clinicians who monitorfatigue often do so as part of a diagnostic workup for anemia. Thisfocus on anemia is understandable,since anemia is the most commoncause of fatigue in CKD. And anemia has been associated with a hostof problems, including heart disease,loss of mental function, and weakenedimmune response. In fact, NKF-DOQI guidelines* recommend an anemiaworkup in any CKD patient with aGFR 60 (stage 3, 4, or 5).Making fatigue assessment part of aworkup for anemia can add useful information about the patient’s symptoms.But there is another reason to monitorfatigue in patients with CKD. Quitesimply, the fatigue itself is a concern.The experience of fatigue can, and does,have a dramatic effect on the lives ofCKD patients. For example, it is notuncommon for CKD patients to quittheir jobs due to fatigue before theyever start dialysis. In one small study,8 of 9 CKD patients who quit theirjobs cited severe fatigue and loss of*Assessment of fatigue is not part of the NKF-DOQI algorithmfor diagnosis and treatment of anemia.www.lifeoptions.orgenergy as the reason.3 Unfortunately,leaving a job may result in lifelongeconomic hardship and/or the lossof health insurance coverage.Chronic fatigue can also reduce patients’quality of life. Results of a poll fromHarris Interactive demonstrated thesignificant effects of fatigue, includingless ability to exercise and participatein social activities. Some patientsclaimed fatigue “prevented themfrom having a normal life.”4The impact of fatigue on every aspectof patients’ lives warrants careful, consistent monitoring. Unfortunately,patients frequently do not report fatigue.As a result, dialysis professionals needto take a more proactive approachto assess this common symptom.Assessing FatigueDialysis clinicians cannot rely onpatient self-reporting to help themmake a diagnosis of fatigue. Manypatients are reluctant to reportfatigue—even if it is severe—for fearof being considered unmotivated or weak.Too, the development and gradualworsening of fatigue over time maycause patients to “adjust” to lowerenergy levels, so they fail to recognizethe magnitude of their impairment.Nevertheless, the subjective nature offatigue requires that information comefrom patients’ symptom reports. Howcan clinicians best encourage andinterpret patient reports of fatigue?Ask first. Don’t assume the patientwill offer information about fatigue,or that you can make a diagnosis(continued on page S4)www.kidneyschool.org
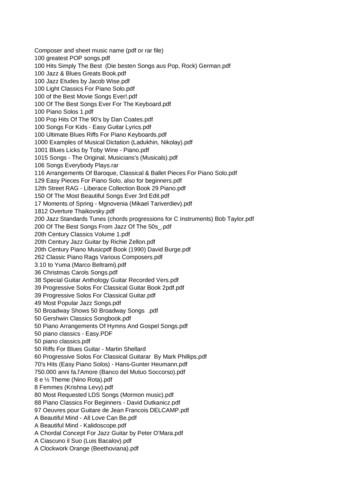
The Role of Deconditioning in Fatigue“There’s an important component offatigue that is largely unrecognized inCKD patients,” claims Dr. BrentMiller, assistant professor of medicineat Washington University in St. Louis.It’s deconditioning. “In spite of thefact that [Dr.]Trish Painter and othershave been writing about the effects ofdeconditioning in dialysis patientsfor decades, the same phenomenonis just not on the radar screen inCKD,” says Miller. “And we needto address it if we want to help ourpatients return to active lifestyles.”Hidden ProblemWhat is deconditioning? It is themuscle atrophy and related weaknessthat result from a prolonged periodof inactivity. “It’s insidious andgradual,” says Miller, “and it definitely starts in CKD.”Deconditioning can make patients soweak that they are not able to do muchphysical activity. Their inactivity, inturn, allows more deconditioning,setting off a downward spiral thatcan result in serious disability.So, why doesn’t deconditioningget more attention? “There are somany things that must come firstin CKD,” says Miller. “Cliniciansmust identify and treat the medicalcauses of fatigue, like anemia, electrolyte imbalance, hypertension,acidosis, etc., and that takes time.”Next, physicians need to rule outany side effects of medication, aswell as uremia. “The effects ofdeconditioning are hidden by somany other things,” says Miller,“we often don’t get around tocorrecting muscle weakness.”Action PlanMiller and his colleagues at the CKDclinic of Washington University inSt. Louis would like to see a greateremphasis on preventing deconditioning in CKD patients. “We’re takingthe first ‘baby steps,’” says Miller,“by just identifying the need.”(continued on page S4)Using a Fatigue Rating ScaleRecognizing and assessing fatigue are needed toprovide treatment. For CKD patients, fatigueassessment is often informal, but there are severalwell-developed fatigue rating scales available.Fatigue scales attempt to measure either: Intensity of fatigue (perceived) Functional limits caused by fatigue (perceived)Although there is no “gold standard” assessment tool,because fatigue is subjective and difficult to define,the following fatigue scales may be useful.Brief Fatigue Inventor y – 6 questions scored usinga scale of 0–10, with 0 being “no fatigue” and 10 being“as bad as you can imagine.” Although the test wasoriginally developed for use in cancer patients, thistool measures the impact of fatigue on activities ofdaily living. It was developed by the University ofTexas, M.D. Anderson Cancer Center. For moreinformation and permission to use the survey, go tothe M.D. Anderson website at www.mdanderson.org.Fatigue Severity Scale – 9 items scored using a numericalscale of 1–7. Patients rate how each of the 9 statementsapplies to their fatigue during the past week; higher scoresmean the statement is more accurate. This scale has beenused to differentiate between clinical depression andfatigue and was developed for use in patients with multipleS2www.lifeoptions.orgsclerosis and other conditions associated with chronicfatigue. (Krupp LB, et al. Arch Neurol 46:1121-3, 1989).Multidimensional Assessment of Fatigue (MAF)Scale – 16 items scored using a numerical scale of 1–10;2 items have multiple-choice responses. The MAF scaleis designed for use in patients with chronic illness, andattempts to assess the impact of fatigue on activities ofdaily living. Translations are available in several languages.The MAF is copyrighted by Basia Belza, PhD, RN,University of Washington–Seattle. To obtain permissionto use the MAF, complete the permission form on thewebsite at www.son.washington.edu/research/maf/.The scales listed here represent just a sample of the manyfatigue assessment scales available. The decision touse a formal fatigue scale must be based on practicalconsiderations in the individual clinical setting. Recognizingthe need to assess fatigue is the critical factor.Recently, work has been done on a comprehensiveassessment tool that attempts to identify dialysis patientsat risk for poor outcomes. The 16-item tool, called theRisk for Outcomes Adverse to Dialysis (ROAD) includesa question about fatigue. Preliminary testing indicatesthat the ROAD may help clinicians identify hemodialysispatients who are at risk for hospitalization and poor qualityof life. (Lamb, et al. Neph Nurs J 31:267-282, 2004.)www.kidneyschool.org
Q & A:Ask the ExpertsAn interview with Charlotte Szromba, MSN, CNN, APRN, BCNurse Practitioner, Section of Nephrology, University of Chicago, Chicago, ILCharlotte Szromba is a nurse practitioner at the University of Chicago Nephrology/Transplant Outpatient Clinic.The target population served in this clinic are patients with chronic kidney disease stages 2–4.Charlotte has a case load of patients and manages the anemia treatment program at the clinic. She has20 years of experience in nephrology nursing.Q: In your experience,how well do CKDpatients self-reporttheir symptoms,especially fatigue?A: Patient self-reporting of fatigueis quite variable. In some cases,fatigue is the primary presentingsymptom—the reason a patientseeks medical help. These patientsrecognize that their fatigue is aproblem and are very ready to talkabout it. At the other end of thespectrum are patients who don’tmention fatigue at all. They don’tthink it is “serious,” because theydon’t realize it can be a sign of amedical problem. They tend toworry about other, more specificsymptoms, and don’t think fatigueis a cause for concern. In fact, manythink fatigue is just a normal partof getting older and don’t want toappear to be complaining about it.We know as health care providersthat fatigue can impact quality of life,preventing patients from doing thingsthey want to do, or having energy tointeract with family and friends.Q. What do you do inyour clinic to evaluatepatients for fatigue?A: As a specialty clinic, weinclude evaluation of fatigue inthe initial patient assessment.Every patient is asked about hisor her energy level. I have foundthat I can get a good sense ofwhether fatigue is a problemby asking: “Are you able to doeverything you want to do?” Thisworks much better than asking,“How’s your energy level?”I listen carefully to patient responses.If they report restricted activity, orstarting things they can’t finish,I consider fatigue. If they say,“I can’t do anything,” and reportthat they don’t even try, I inquireabout depression, too. I simply ask,“I’m wondering if you’re feelingdepressed.” You’d be surprised athow readily patients will admit todepression; just asking opens thedoor. Finally, I always ask aboutsleep patterns. Daytime sleepinessis often a sign of fatigue and mayalso indicate progression of theirkidney disease.At follow-up, I continue to askabout activity levels. We seestage 2 patients every 6 months.By stage 4, we are seeingpatients monthly. If patients arereceiving treatment for anemia, Ilook for them to report that theyfeel less tired and are able to domore of their regular activitiesabout 6–8 weeks after startingtreatment.www.lifeoptions.orgQ. Do you useany formal fatigueassessment tools?A: There are many different toolsfor assessing fatigue, physicaland social functioning, but we donot use specific tools at this time.However, if patients are experiencingfatigue I may ask that they keepa daily log to help me evaluate theimpact of fatigue in their lives.It may seem like a lot of paperwork,but it can help patients rememberbetter and be more specific whenthey come in for their visits.Several tests are also available toevaluate or rule out depression.Most recently, we have used theSF-36 to get a baseline measureof functioning and well-being,then we re-do the test at the3–4 month follow-up visit. Othervaluable tools recommended inthe K/DOQI Clinical PracticeGuidelines on chronic kidneydisease include the DartmouthCOOP Functional HealthAssessment Chart, the DukeHealth Profile, and the KidneyDisease Quality of Life Tool,which is specific to kidneydisease. By carefully listeningto our patients and asking questions, we can help them managetheir fatigue and improve theirquality of life.www.kidneyschool.orgS3
Fatigue in CKD(continued from page S1)from observations or lab reports. Severe fatiguecan exist even if lab values are “normal”; onlypatients can tell you how they are really feeling.Be specific. Different patients will use different wordsto talk about fatigue, including tired, weak, lack of energy,or exhausted. The varied vocabulary makes it difficultto interpret patient reports. Instead, ask about howthe fatigue is affecting specific activities of daily living.Educate. Patients need to understand that severefatigue is not “normal,” and that there are treatmentoptions for fatigue. Knowing help is available mayencourage more honest reports.Tr y tools. Consider using a formal assessment toolto measure and evaluate fatigue. There are severalavailable. (See sidebar on page S2 for examples.)Rule out depression. The symptoms of depressionmay mimic the symptoms of severe fatigue. Considera psychological evaluation to rule out depression.The effects of fatigueon CKD patients can bedevastating. Clinicianswho are prepared towork with their CKDpatients to diagnoseand assess fatigue canhelp them maintaintheir quality of life.ReferencesQuiz Answers1. True2. True3. False. It is importantto be very detailedand specific aboutyour symptoms.4. True5. True1. Obrador GT, Ruthazer R,Arora P, et al. Prevalence ofand factors associated with suboptimal care before initiation ofdialysis in the United States. J Am Soc Nephrol 10:1793-1800, 19992. From DOPPS study reports and slide presentations at www.dopps.org3. Schatell D, Ellstrom-Calder A, Alt PS, et al. Survey of CKDpatients reveals significant gaps in knowledge about kidneydisease—Part 1. Nephrol News Issues 17:5:23-6, 20034. Harris Interactive Poll. New survey provides insight into CKD,exhaustion, anemia. Nephrol News Issues 17:2:29-31, 2003(continued from page S2)The Role of Deconditioning in FatigueNext steps include: Asking every CKD patientabout fatigue Educating patients and familiesabout the problem of fatigue Convincing patients that fatigueis not acceptable Providing good clinical carefor all medical problems Promoting increased activityMiller notes. “And you don’t have“In today’s world, anemia should bethe same level of support—the PTs,identified and treated right away. Wetechnicians, etc.—that you’d have in arecognize the need to treat anemia predialysis unit.” Finally, Miller findsdialysis, and it is no longer acceptablethat the patients themselves areto have a patient starting dialysis withslow to get motivated. “Onlya hematocrit of 20.” Similarly, Millerabout 15%–20% of our patients buydoesn’t think it should be acceptableinto the need for exercise,” saysto allow CKD patients to becomeMiller. “So many patients just takesedentary and deconditioned.for granted that fatiguegoes hand in hand withkidney disease.”In Control“We do a good job of getting ourtransplant patients moving,” saysMiller. “We even give them pedometers when they leave the hospital.”Now, it’s time to focus on CKD.Still, Miller hopes that oneday soon promoting activityfor CKD patients to prevent deconditioning will“become as important asanemia management.”Right now, no one reallytakes it seriously, he says,including the governmentor insurers. But Millerhopes that will change.ChallengesMiller admits it is difficult to getCKD patients to exercise. “Forone thing, you only see CKDpatients once every 3 months,”S4www.lifeoptions.orgContact:Life Options Rehabilitation Programc/o Medical Education Institute, Inc.414 D’Onofrio Drive, Ste. 200Madison, WI 53719Tel: (800) 468-7777Fax: ( 608) 833-8366E-mail: kidneyschool.orgwww.kidneyschool.org
PatientsA Medical Education Institute/Life Options PublicationVOL. 1 NO. 4DECEMBER 2004Reporting and Managing FatigueMany people complain of feeling wornout or having less energy and think it’sdue to being out of shape, not gettingenough sleep, or being stressed. All ofthese may be true, but fatigue can also bea symptom of a more serious problem—early chronic kidney disease.Why and How to Report FatigueAnemia 101In healthy people, the kidneys make ahormone called erythropoietin (EPO) thathelps your body make red blood cells.Anemia begins early in kidney disease,when the kidneys are still working atabout 45%, and tends to get worse as thekidneys lose function and produce less EPO.Fatigue can come on slowly and you mightnot know it is a “symptom” worth tellingyour doctor about. But fatigue in CKD ismost often caused by anemia, a shortage ofoxygen-carrying red blood cells. Anemia—and fatigue—can and should be treatedearly to help you feel better and to prevent heart problems down the road.Besides feeling very tired, other symptomsof anemia can include:To report your fatigue, it is key to knowhow to describe exactly what you feel.For example, saying “I feel tired” doesnot tell your doctor as much as if you say,“I am too tired to walk down the drivewayand pick up my newspaper.” Being veryspecific andIn Control is supportedoffering detailby Amgen Inc.can help yourdoctor see thatand published inyour fatigue iscooperation withsevere enoughto limit yourdaily activities. Dizziness/lightheadednesswww.lifeoptions.org Feeling cold all the time Shortness of breath/chest pain Pale skin, gums, and fingernail beds Trouble concentrating HeadachesThe most important reason to reportyour symptoms and get early treatmentis that anemia can cause heart damagecalled left ventricular hypertrophy (theheart muscle grows too big, trying toget more oxygen through your body).LVH is the leading cause of death inpeople with kidney failure. By the timethe kidneys fail, nearly 75% of peoplealready have some degree of LVH.(continued on page P4)www.kidneyschool.orgP1
PatientsReporting Fatigue Allows Early TreatmentFatigue is one of the most common—but often least reported—symptoms ofearly chronic kidney disease; a symptomthat 2-year CKD patient Julie knows alltoo well. Concerned by her long-termlack of energy, Julie saw her doctor,who found her kidney disease andtreated her fatigue.Not Feeling Like HerselfFor a few years, 41-year-old Julie hadnoticed that she was always tired afterwork. “I just thought ‘gosh, I’m so tiredall the time,’” she recalls. “I thought itwas related to my age or weight gain.”It wasn’t for a while that she went toget a full physical.“I started to notice that some thingswith my general health were ‘off’—inaddition to being tired, I had shoulderand back soreness and a swollen lymphnode in my armpit,” says Julie. “Somethingjust seemed to be wrong and I thoughtI should bring it up to my doctor.”Julie saw her family doctor, who ran labtests. “The tests found that I had mildanemia,” recalls Julie. “My doctor saidI should start taking iron pills to helpwith the fatigue.” But besides anemia,tests showed that Julie’s creatinine levelwas too high—a sign of kidney disease.Seven months of tracking her creatininelevels ended in a kidney ultrasound thatshowed scarring. Julie was referredto a nephrologist.P2www.lifeoptions.orgChronic Kidney DiseaseThe nephrologists did a biopsy, whichrevealed that Julie had interstitialnephritis. He believed Julie’s kidneydisease may have been a result ofundiagnosed Sjögren’s syndrome—anautoimmune disease in which whiteblood cells attack moisture-producingglands. “I had the classic symptomof very dry and red eyes, as well asfatigue, but not enough other symptomsto diagnose me,” explains Julie.At first shocked by her kidney disease,Julie tried to learn as much as shecould, for herself and for her family.“My teen-aged daughter needed toknow that I wasn’t going to vanish fromher life any time soon,” says Julie. “So,without painting too rosy of a picture,I told her about my disease and let herask questions.”Treating AnemiaLab tests done during her nephrologistvisit showed that Julie’s hemoglobinlevel was still too low, so he prescribedEPO. “I’m glad EPO exists because notso long ago people with anemia neededto have blood transfusions—and I feellike I’ve been spared the downside ofkidney disease,” says Julie. “I neverwent through severe fatigue, becausemy anemia was caught early enough.”Julie never linked her fatigue and lack ofenergy to anemia. “I felt that the diseasewww.kidneyschool.org
Patientsprocess in my body and the higheramount of waste in my blood could becausing my fatigue,” explains Julie. Sheknew that iron pills were often used totreat mild anemia, but didn’t know therewere prescription drugs that could helpwith fatigue.Staying ActiveJulie’s energy level and sleep needs stillvary, but she has kept working 4 days aweek as a mechanical engineer, keepingher life as active and normal as it can be.“I have so many nephrologist visits thatit’s good to have one day off a week tofit those in,” she notes. “It also helpsto be able to sleep late, since I’ve foundthat I need more sleep now that I havekidney disease.”With changing levels of energy fromday-to-day, Julie takes it easy and sleepsmore when she needs to, but also keepsup with her exercise. “Staying active iskey to good health or you get in a cycleof not doing anything,” she says. “I walkand sometimes go to the gym, but I alsolet myself sit down and put my feet upif I need to.”Tips and LessonsJulie’s kidneys are now working at 15%and she expects to start dialysis in a yearor so, but she feels pretty good, saying,“I know that I need to take it easier andthat I can’t push myself for weeks at atime, but I can do most everything.”www.lifeoptions.orgJulie tracks her hemoglobin and hematocritlevels with her nephrologist, who changesher EPO and iron doses as needed.“Pay attention to how you’re feeling anddon’t ignore it,” advises Julie. “Evenif you think it could be nothing, reportyour symptoms!” Julie did, and it hasled her to early treatment for fatigue andtime to prepare for dialysis. “You needto stay involved in your care and learnas much as you can about yourself andyour disease,” says Julie. “As you learnmore and talk to others with kidneydisease it doesn’t seem so scary.”For More Information.For more information about managing fatigue and reporting symptoms,visit: Kidney School Module 6:Anemia and Kidney Disease,Kidney School Module 7:Understanding Kidney Lab Tests,and Kidney School Module 12:Staying Active with Kidney Disease,at www.kidneyschool.org.www.kidneyschool.orgP3
PatientsReporting and Managing Fatigue (continued from page P1)Your doctor will do blood tests to see ifyou have anemia. These tests include: Hemoglobin (Hgb or Hb) – measures theamount of oxygen in your red blood cells. Hematocrit (Hct, or “crit”) – measuresthe percent of your blood that is madeup of red blood cells.The good news is that anemia can betreated. If you have anemia, your doctormay prescribe EPO to help your bodymake red blood cells. This treatmentwill help give you more energy, a betterappetite, and greater endurance. Yourdoctor may also prescribe iron supplements if your iron levels are too low.Reporting and managing fatigue andother symptoms will help you maintainyour health and lifestyle.With early treatment of fatigue, you can keepdoing the things you did before you hadkidney disease—work, volunteer, exercise.Staying active and involved are key toliving long and well with any chronichealth problem.For More Information Visit Life Options’ Kidney School Module 6: Anemiaand Kidney Disease at www.kidneyschool.org. Take the Continuum Health Partners’ Fatigue Assessmentat www.wehealny.org/healthinfo/index.html. Thisfatigue test is a tool to find the level of your fatigue.After submitting the survey, general fatigue information,tips, and resources are offered. Order The Iron Story from the American Associationof Kidney Patients (AAKP) at (800) 749-2257.ResultsStudies show that if you have to startdialysis, you’ll do much better if yourfatigue and anemia are under control.Fatigue Quiz See the National Kidney Foundation’s Getting the Mostfrom Your Treatment Series: What You Need to Knowabout Anemia at www.kidney.org/general/atoz/.Now that you’ve read about managing and reporting fatigue, let’s see how much you’velearned! See if you can answer the questions below (the answers are on page S8).1. Fatigue is one symptom of early chronickidney disease. True FalseIn ControlContact:2. Treating fatigue early will help you feel betterLife Options Rehabilitation Programdown the road. True Falsec/o Medical Education Institute, Inc.3. “I feel tired” is a good way to describe your414 D’Onofrio Drive, Ste. 200Madison, WI 53719fatigue. True FalseTel: (800) 468-77774. By the time the kidneys fail, most people alreadyFax: ( 608) 833-8366have some heart damage. True FalseE-mail: lifeoptions@meiresearch.org5. EPO is prescribed to help your body makewww.lifeoptions.orgwww.kidneyschool.orgred blood cells. True FalseP4www.lifeoptions.orgwww.kidneyschool.org
to living well with kidney disease. The 2-in-1 format of In Contr ol is designed to make it easy to find the infor-mation and share it with your patients. For you, there are 4 pages of professional content (pages S1, S2, S7, and S8), along with practical tips for putting k