Transcription
A TreATmenT ImprovemenT proTocolImproving CulturalCompetenceTIP 59
A TreATmenT ImprovemenT proTocolImproving CulturalCompetenceTIP 59U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICESSubstance Abuse and Mental Health Services AdministrationCenter for Substance Abuse Treatment1 Choke Cherry RoadRockville, MD 20857
Improving Cultural CompetenceAcknowledgmentsThis publication was produced by The CDM Group, Inc., under the Knowledge ApplicationProgram (KAP) contract numbers 270-99-7072, 270-04-7049, and 270-09-0307 with theSubstance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department ofHealth and Human Services (HHS). Andrea Kopstein, Ph.D., M.P.H., Karl D. White, Ed.D.,and Christina Currier served as the Contracting Officer’s Representatives.DisclaimerThe views, opinions, and content expressed herein are those of the consensus panel and do notnecessarily reflect the views, opinions, or policies of SAMHSA or HHS. No official support ofor endorsement by SAMHSA or HHS for these opinions or for particular instruments, software,or resources is intended or should be inferred.Public Domain NoticeAll materials appearing in this volume except those taken directly from copyrighted sources arein the public domain and may be reproduced or copied without permission from SAMHSA orthe authors. Citation of the source is appreciated. However, this publication may not bereproduced or distributed for a fee without the specific, written authorization of the Office ofCommunications, SAMHSA, HHS.Electronic Access and Copies of PublicationThis publication may be ordered or downloaded from SAMHSA’s Publications Ordering Webpage at http://store.samhsa.gov. Or, please call SAMHSA at 1-877-SAMHSA-7 (1-877-7264727) (English and Español).Recommended CitationSubstance Abuse and Mental Health Services Administration. Improving Cultural Competence.Treatment Improvement Protocol (TIP) Series No. 59. HHS Publication No. (SMA) 14-4849.Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014.Originating OfficeQuality Improvement and Workforce Development Branch, Division of Services Improvement,Center for Substance Abuse Treatment, Substance Abuse and Mental Health ServicesAdministration, 1 Choke Cherry Road, Rockville, MD 20857.HHS Publication No. (SMA) 14-4849First Printed 2014ii
Please share your thoughts about this publication by completing a brief online survey at:https://www.surveymonkey.com/r/KAPPFSThe survey takes about 7 minutes to complete and is anonymous.Your feedback will help SAMHSA develop future products.
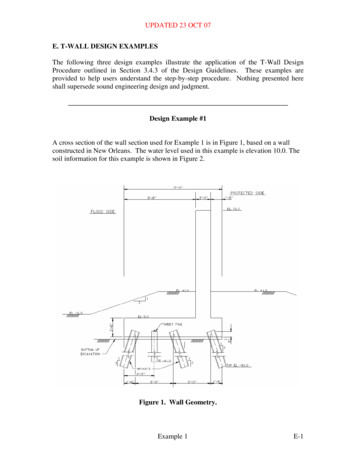
ContentsConsensus Panel. viiKAP Expert Panel and Federal Government Participants .ixWhat Is a TIP? .xiForeword . xiiiExecutive Summary . xvChapter 1—Introduction to Cultural Competence . 1Purpose and Objectives of the TIP. 2Core Assumptions. 4What Is Cultural Competence? . 5Why Is Cultural Competence Important? . 7How Is Cultural Competence Achieved? . 9What Is Culture? . 11What Is Race? . 13What Is Ethnicity? . 15What Is Cultural Identity? . 16What Are the Cross-Cutting Factors in Race, Ethnicity, and Culture? . 16As You Proceed . 33Chapter 2—Core Competencies for Counselors and Other Clinical Staff .35Core Counselor Competencies . 36Self-Assessment for Individual Cultural Competence . 55Chapter 3—Culturally Responsive Evaluation and Treatment Planning.57Step 1: Engage Clients. 59Step 2: Familiarize Clients and Their Families With Treatment and Evaluation Processes . 59Step 3: Endorse Collaboration in Interviews, Assessments, and Treatment Planning. 60Step 4: Integrate Culturally Relevant Information and Themes . 61Step 5: Gather Culturally Relevant Collateral Information . 64Step 6: Select Culturally Appropriate Screening and Assessment Tools. 65Step 7: Determine Readiness and Motivation for Change . 69Step 8: Provide Culturally Responsive Case Management . 70Step 9: Integrate Cultural Factors Into Treatment Planning . 71iii
Improving Cultural CompetenceChapter 4—Pursuing Organizational Cultural Competence .73Cultural Competence at the Organizational Level . 74Organizational Values . 76Governance . 78Planning . 80Evaluation and Monitoring . 84Language Services. 88Workforce and Staff Development . 90Organizational Infrastructure . 96Chapter 5—Behavioral Health Treatment for Major Racial and Ethnic Groups . 101Introduction . 102Counseling for African and Black Americans . 103Counseling for Asian Americans, Native Hawaiians, and Other Pacific Islanders . 116Counseling for Hispanics and Latinos . 128Counseling for Native Americans. 138Counseling for White Americans . 150Chapter 6—Drug Cultures and the Culture of Recovery . 159What Are Drug Cultures? . 161The Role of Drug Cultures in Substance Abuse Treatment . 171Appendix A: Bibliography . 177Appendix B: Instruments To Measure Identity and Acculturation . 253Appendix C: Tools for Assessing Cultural Competence . 259Appendix D: Screening and Assessment Instruments . 277Appendix E: Cultural Formulation in Diagnosis and Cultural Concepts of Distress . 283Appendix F: Cultural Resources . 287Appendix G: Glossary . 295Appendix H: Resource Panel . 299Appendix I: Cultural Competence and Diversity Network Participants . 301Appendix J: Field Reviewers . 303Appendix K: Acknowledgments. 307List of ExhibitsExhibit 1-1: Multidimensional Model for Developing Cultural Competence . 6Exhibit 1-2: The Continuum of Cultural Competence . 10Exhibit 1-3: Common Characteristics of Culture . 12Exhibit 1-4: Education and Culture . 22iv
ContentsExhibit 1-5: Cultural Identification and Cultural Change Terminology . 24Exhibit 1-6: Five Levels of Acculturation . 25Exhibit 1-7: Measuring Acculturation . 27Exhibit 2-1: Stages of Racial and Cultural Identity Development . 40Exhibit 2-2: Counselor Worldview. 43Exhibit 2-3: ACA Counselor Competencies: Counselor s' Awareness of TheirOwn Cultural Values and Biases. 46Exhibit 2-4: ACA Counselor Competencies: Awareness of Clients' Worldviews . 47Exhibit 2-5: Attitudes and Behaviors of Culturally Competent Counselors . 49Exhibit 2-6: ACA Counselor Competencies: Culturally Appropriate InterventionStrategies . 56Exhibit 3-1: Client–Counselor Matching . 71Exhibit 4-1: Requirements for Organizational Cultural Competence . 75Exhibit 4-2: Creating Culturally Responsive Treatment Environments . 75Exhibit 4-3: Hands Across Cultures Mission Statement . 78Exhibit 4-4: Critical Treatment Issues To Consider in Providing Culturally ResponsiveServices . 80Exhibit 4-5: Qualities of Effective Cultural Competence Training . 92Exhibit 4-6: OMH Staff Education and Training Guidelines. 94Exhibit 4-7: Cultural Competence Initiative Across Time in One Organization . 99Exhibit 5-1: Core Culturally Responsive Principles in Counseling African Americans . 110Exhibit 5-2: Lifetime Prevalence of Substance Use Disorders According to EthnicSubgroup and Immigration Status . 130Exhibit 5-3: Native Americans and Community . 143Exhibit 5-4: The Lakota Version of the 12 Steps . 147Exhibit 6-1: How Drug Cultures Differ . 162Exhibit 6-2: The Language of a Drug Culture . 164Exhibit 6-3: The Values and Beliefs of a Heroin Culture . 166Exhibit 6-4: Music and Drug Cultures . 166Exhibit 6-5: The Rituals of Drug Cultures . 168Exhibit 6-6: Questions Regarding Knowledge and Skill Demands of Heroin Use . 168Exhibit 6-7: 12-Step Group Values and the Culture of Recovery . 174v
Consensus PanelNote: Information given indicates each participant’s affiliation during the time the panel wasconvened and may no longer reflect the individual’s current affiliation.ChairWorkgroup LeadersFelipe González Castro, M.S.W., Ph.D.ProfessorDepartment of PsychologyArizona State UniversityTempe, AZVirgil A. Gooding, Sr., M.A., M.S.W.,LISCClinical DirectorFoundation II, Inc.Cedar Rapids, IACo-ChairsFord H. Kuramoto, D.S.W.PresidentNational Asian Pacific American FamiliesAgainst Substance AbuseLos Angeles, CALoretta J. Bradley, M.A., Ph.D.ProfessorDepartment of Educational PsychologyTexas Tech UniversityLubbock, TXJacqueline P. Butler, M.S.W., CCDC,LISWProfessor of Clinical PsychiatrySubstance Abuse DivisionCollege of MedicineUniversity of CincinnatiCincinnati, OHFlanders Byford, M.S.W., LCSWOklahoma City-County Health DepartmentOklahoma City, OKTing-Fun May Lai, M.S.W., CSW,CASACDirectorChinatown Alcoholism CenterHamilton-Madison HouseNew York, NYHarry Montoya, M.A.President/Chief Executive OfficerHands Across CulturesEspañola, NMOnaje M. Salim, M.A., NCAC-II, CCSDirectorCork Institute Southeast AddictionTechnology Transfer CenterMorehouse School of MedicineAtlanta, GAPanelistsBarbara Lee Aragon, M.S.W.Academic FellowDepartment of Health ServicesNorth Highlands, CAvii
Improving Cultural CompetenceDebra A. Claymore, M.Ed.Adm.D. Claymore & Associates, Inc.Loveland, COE. Daniel Edwards, D.S.W.DirectorEthnic Studies ProgramUniversity of UtahSalt Lake City, UTTonda L. Hughes, M.S.N., Ph.D., FAANAssociate ProfessorCollege of NursingUniversity of Illinois at ChicagoChicago, ILDavid Mathews, M.A., Ph.D.Director of Adult ServicesKentucky River Community Care, Inc.Jackson, KYAnthony (Tony) Taiwai Ng, M.D.ConsultantWashington, DCBarry Pilson, Ph.D.Adjunct ProfessorSchool of Social WorkTulane UniversityMetairie, LAviiiRafaela R. Robles, Ed.D.DirectorTechnology Transfer CenterCaribbean Basin/Hispanic AddictionCentro de Estudios en AdicciónUniversidad Central del CaribeBayamon, PRGloria M. Rodriguez, D.S.W.Research ScientistDivision of Addiction ServicesNew Jersey Department of Health and SeniorServicesTrenton, NJAnn S. Yabusaki, M.Ed., M.A., Ph.D.DirectorCoalition for a Drug-Free HawaiiHonolulu, HI
KAP Expert Panel and FederalGovernment ParticipantsNote: Information given indicates each participant’s affiliation during the time the panel wasconvened and may no longer reflect the individual’s current affiliation.Barry S. Brown, Ph.D.Adjunct ProfessorUniversity of North Carolina at WilmingtonCarolina Beach, NCJacqueline Butler, M.S.W., LISW, LPCC,CCDC III, CJSProfessor of Clinical PsychiatryCollege of MedicineUniversity of CincinnatiCincinnati, OHDeion CashExecutive DirectorCommunity Treatment and CorrectionCenter, Inc.Canton, OHDebra A. Claymore, M.Ed.Adm.D. Claymore & Associates, Inc.Loveland, COCarlo C. DiClemente, Ph.D.ChairDepartment of PsychologyUniversity of Maryland Baltimore CountyBaltimore, MDCatherine E. Dube, Ed.D.Independent ConsultantBrown UniversityProvidence, RIJerry P. Flanzer, D.S.W., LCSW, CACChief of ServicesDivision of Clinical and Services ResearchNational Institute on Drug AbuseNational Institutes of HealthBethesda, MDMichael Galer, D.B.A.Independent ConsultantWestminster, MARenata J. Henry, M.Ed.DirectorDivision of Alcoholism, Drug Abuse andMental HealthDelaware Department of Health and SocialServicesNew Castle, DEJoel Hochberg, M.A.PresidentAsher & PartnersLos Angeles, CAJack Hollis, Ph.D.Associate DirectorCenter for Health ResearchKaiser PermanentePortland, ORix
Improving Cultural CompetenceMary Beth Johnson, M.S.W.DirectorAddiction Technology Transfer CenterUniversity of Missouri—Kansas CityKansas City, MOEduardo Lopez, B.S.Executive ProducerEVS CommunicationsWashington, DCHolly A. Massett, Ph.D.Academy for Educational DevelopmentWashington, DCDiane Miller, Ph.D.ChiefScientific Communications BranchNational Institute on Alcohol Abuseand AlcoholismNational Institutes of HealthBethesda, MDHarry B. Montoya, M.A.President/Chief Executive OfficerHands Across CulturesEspañola, NMRichard K. Ries, M.D.Director/ProfessorOutpatient Mental Health ServicesDual Disorder ProgramsSeattle, WAGloria M. Rodriguez, D.S.W.Research ScientistDivision of Addiction ServicesNew Jersey Department of Health and SeniorServicesTrenton, NJEverett Rogers, Ph.D.Center for Communications ProgramsJohns Hopkins UniversityBaltimore, MDJean R. Slutsky, P.A., M.S.P.H.DirectorCenter for Outcomes and EvidenceAgency for Healthcare Research and QualityRockville, MDNedra Klein Weinreich, M.S.PresidentWeinreich CommunicationsCanoga Park, CAClarissa WittenbergDirectorOffice of Communications andPublic LiaisonNational Institute of Mental HealthNational Institutes of HealthBethesda, MDConsulting Members of the KAPExpert PanelPaul Purnell, M.ASocial Solutions, L.L.C.Potomac, MDScott Ratzan, M.D., M.P.A., M.A.Academy for Educational DevelopmentWashington, DCThomas W. Valente, Ph.D.Director, Master of Public Health ProgramDepartment of Preventive MedicineSchool of MedicineUniversity of Southern CaliforniaAlhambra, CAPatricia A. Wright, Ed.D.Independent ConsultantBaltimore, MDx
What Is a TIP?Treatment Improvement Protocols (TIPs) are developed by the Substance Abuse and MentalHealth Services Administration (SAMHSA) within the U.S. Department of Health and HumanServices (HHS). TIPs are best practice guidelines for the treatment of substance use disorders.TIPs draw on the experience and knowledge of clinical, research, and administrative experts toevaluate the quality and appropriateness of various forms of treatment. TIPs are distributed tofacilities and individuals across the country. Published TIPs can be accessed via the Internet athttp://store.samhsa.gov.Although each TIP strives to include an evidence base for the practices it recommends,SAMHSA recognizes that the field of substance abuse treatment is continually evolving, andresearch frequently lags behind the innovations pioneered in the field. A major goal of each TIPis to convey front-line information quickly but responsibly. If research supports a particularapproach, citations are provided.xi
ForewordThe Substance Abuse and Mental Health Services Administration (SAMHSA) is the agencywithin the U.S. Department of Health and Human Services that leads public health efforts toadvance the behavioral health of the nation. SAMHSA’s mission is to reduce the impact ofsubstance abuse and mental illness on America’s communities.The Treatment Improvement Protocol (TIP) series fulfills SAMHSA’s mission to reduce theimpact of substance abuse and mental illness on America’s communities by providing evidencebased and best practice guidance to clinicians, program administrators, and payers. TIPs are theresult of careful consideration of all relevant clinical and health services research findings,demonstration experience, and implementation requirements. A panel of non-federal clinicalresearchers, clinicians, program administrators, and patient advocates debates and discusses theirparticular area of expertise until they reach a consensus on best practices. This panel’s work isthen reviewed and critiqued by field reviewers.The talent, dedication, and hard work that TIPs panelists and reviewers bring to this highlyparticipatory process have helped bridge the gap between the promise of research and the needsof practicing clinicians and administrators to serve, in the most scientifically sound and effectiveways, people in need of behavioral health services. We are grateful to all who have joined with usto contribute to advances in the behavioral health field.Pamela S. Hyde, J.D.AdministratorSubstance Abuse and Mental Health Services AdministrationH. Westley Clark, M.D., J.D., M.P.H., CAS, FASAMDirectorCenter for Substance Abuse TreatmentSubstance Abuse and Mental Health Services Administrationxiii
Executive SummaryThe development of culturally responsiveclinical skills is vital to the effectiveness ofbehavioral health services. According to theU.S. Department of Health and HumanServices (HHS), cultural competence “refers tothe ability to honor and respect the beliefs,languages, interpersonal styles, and behaviors ofindividuals and families receiving services, aswell as staff members who are providing suchservices. Cultural competence is a dynamic,ongoing developmental process that requires along-term commitment and is achieved overtime” (HHS 2003a, p. 12). It has also beencalled “a set of behaviors, attitudes, and policiesthat . . . enable a system, agency, or group ofprofessionals to work effectively in crosscultural situations” (Cross et al. 1989, p. 13).This Treatment Improvement Protocol (TIP)uses Sue’s (2001) multidimensional model fordeveloping cultural competence. Adapted toaddress cultural competence across behavioralhealth settings, this model serves as a framework for targeting three organizational levelsof treatment: individual counselor and staff,clinical and programmatic, and organizationaland administrative. The chapters target specific racial, ethnic, and cultural considerationsalong with the core elements of cultural competence highlighted in the model. These coreelements include cultural awareness, generalcultural knowledge, cultural knowledge ofbehavioral health, and cultural skill development. The primary objective of this TIP is toassist readers in understanding the role ofculture in the delivery of behavioral healthservices (both generally and with reference tospecific cultural groups). This TIP is organizedinto six chapters and begins with an introduction to cultural competence. The followingsubheadings provide a summary of each chapter and an overview of this publication.Introduction to CulturalCompetenceWhy is the development of cultural competence and culturally responsive servicesimportant in the behavioral health field?Culturally responsive skills can improve clientengagement in services, therapeutic relationships between clients and providers, andtreatment retention and outcomes. Culturalcompetence is an essential ingredient in decreasing disparities in behavioral health.The development of cultural competence canhave far-reaching effects not only for clients,but also for providers and communities. Cultural competence improves an organization’ssustainability by reinforcing the value of diversity, flexibility, and responsiveness in addressing the current and changing needs of clients,communities, and the healthcare environment.Culturally responsive organizational strategiesand clinical services can help mitigate organizational risk and provide cost-effective treatment, in part by matching services to clientxv
Improving Cultural Competenceneeds more appropriately from the outset. Sotoo, culturally responsive organizational policies and procedures support staff engagementin culturally responsive care by establishingaccess to training, supervision, and congruentpolicies and procedures that enable staff torespond in a culturally appropriate manner toclients’ psychological, linguistic, and physicalneeds.What is the process of becoming culturallycompetent as a counselor or culturallyresponsive as an organization? Culturalcompetence is not acquired in a limitedtimeframe or by learning a set of facts aboutspecific populations; cultures are diverse andcontinuously evolving. Developing culturalcompetence is an ongoing process that beginswith cultural awareness and a commitment tounderstanding the role that culture plays inbehavioral health services. For counselors, thefirst step is to understand their own cultures asa basis for understanding others. Next, theymust cultivate the willingness and ability toacquire knowledge of their clients’ cultures.This involves learning about and respectingclient worldviews, beliefs, values, and attitudestoward mental health, help-seeking behavior,substance use, and behavioral health services.Behavioral health counselors should incorporate culturally appropriate knowledge, understanding, and attitudes into their actions (e.g.,communication style, verbal messages, treatment policies, services offered), thereby conveying their cultural competence and theirorganizations’ cultural responsiveness duringassessment, treatment planning, and thetreatment process.What is culture? Culture is the conceptualsystem developed by a community or societyto structure the way people view the world. Itinvolves a particular set of beliefs, norms, andvalues that influence ideas about relationships,how people live their lives, and the way peoplexviorganize their world. Culture is not a definableentity to which people belong or do not belong. Within a nation, race, or community,people belong to multiple cultural groups andnegotiate multiple cultural expectations on adaily basis. These expectations, or culturalnorms, are the spoken or unspoken rules orstandards for a given group that indicatewhether a certain social event or behavior isappropriate or inappropriate. The word “culture” is sometimes applied to groups formedon the basis of age, socioeconomic status,disability, sexual orientation, recovery status,common interest, or proximity. Counselorsand administrators should understand thateach client embraces his or her culture(s) in aunique way and that there is considerablediversity within and across races, ethnicities,and culture heritages. Other cultures andsubcultures often exist within larger cultures.What are race and ethnicity? Race is oftenreferred to as a biological category based ongenetic traits like skin color (HHS 2001), butthere are no reliable means of identifying racethrough biological criteria. Despite its limitations, the concept of race is important todiscussions of cultural competence. Race—when defined as a social construct to describepeople with shared physical characteristics—can have tremendous social significance. Theterm ethnicity is often used interchangeablywith race, although by definition, ethnicity—unlike race—implies a certain sense of belonging. It is generally based on shared values,beliefs, and origins rather than shared physicalcharacteristics. With the exception of its finalchapter, which examines drug cultures, thisTIP focuses on the major racial and ethnicgroups identified by the U. S. Census Bureauwithin the United States: African and BlackAmericans, Asian Americans (including Native Hawaiians and other Pacific Islanders),Hispanics and Latinos, Native Americans, andWhite Americans.
Executive SummaryWhat constitutes cultural identity? Culturalidentity, in the simplest terms, involves anaffiliation or identification with a particulargroup or groups. An individual’s culturalidentity reflects the values, norms, andworldview of the larger culture, but it is defined by more than these factors. Culturalidentity includes individual traits and attributes shaped by race, ethnicity, language, lifeexperiences, historical events, acculturation,geographic and other environmental influences, and other forces. Thus, no two individuals will possess exactly the same culturalidentity even if they identify with the samecultural group(s). Cultural identities are notstatic; they develop, evolve, and change acrossthe life cycle.This TIP explores cultural identity and itsinfluence on assessment, treatment planning,and therapeutic and healing practices. Theintroduction it provides to the cross-cuttingfactors of race, ethnicity, and culture will helpcounselors gain knowledge about the manyforces that shape cultures, communities, andthe lives of clients, including, but not limitedto, families and kinships, gender roles, socioeconomic status, religion, education, immigration, and migration.What core assumptions serve as the foundation of this TIP? The consensus paneldeveloped several core assumptions uponwhich to structure the content of this TIP: An understanding of race, ethnicity, andculture (including one’s own) is necessaryto appreciate the diversity of human dynamics and to treat clients effectively. Incorporating cultural competence intotreatment improves therapeutic decisionmaking and offers alternative ways todefine and plan a treatment program firmly directed toward progress and recovery. Organizational commitment to supportingculturally responsive treatment services, including adequate allocation of resources,reinforces the importance of
Improving Cultural Competence . Acknowledgments . This publication was produced by The CDM Group, Inc., under the Knowledge Application Program (KAP) contract n