Transcription
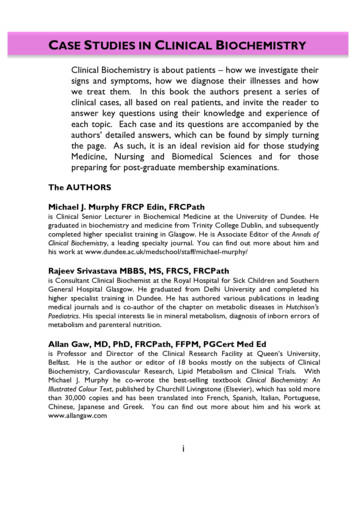
CASE STUDIES IN CLINICAL BIOCHEMISTRYClinical Biochemistry is about patients – how we investigate theirsigns and symptoms, how we diagnose their illnesses and howwe treat them. In this book the authors present a series ofclinical cases, all based on real patients, and invite the reader toanswer key questions using their knowledge and experience ofeach topic. Each case and its questions are accompanied by theauthors’ detailed answers, which can be found by simply turningthe page. As such, it is an ideal revision aid for those studyingMedicine, Nursing and Biomedical Sciences and for thosepreparing for post-graduate membership examinations.The AUTHORSMichael J. Murphy FRCP Edin, FRCPathis Clinical Senior Lecturer in Biochemical Medicine at the University of Dundee. Hegraduated in biochemistry and medicine from Trinity College Dublin, and subsequentlycompleted higher specialist training in Glasgow. He is Associate Editor of the Annals ofClinical Biochemistry, a leading specialty journal. You can find out more about him andhis work at jeev Srivastava MBBS, MS, FRCS, FRCPathis Consultant Clinical Biochemist at the Royal Hospital for Sick Children and SouthernGeneral Hospital Glasgow. He graduated from Delhi University and completed hishigher specialist training in Dundee. He has authored various publications in leadingmedical journals and is co-author of the chapter on metabolic diseases in Hutchison’sPaediatrics. His special interests lie in mineral metabolism, diagnosis of inborn errors ofmetabolism and parenteral nutrition.Allan Gaw, MD, PhD, FRCPath, FFPM, PGCert Med Edis Professor and Director of the Clinical Research Facility at Queen’s University,Belfast. He is the author or editor of 18 books mostly on the subjects of ClinicalBiochemistry, Cardiovascular Research, Lipid Metabolism and Clinical Trials. WithMichael J. Murphy he co-wrote the best-selling textbook Clinical Biochemistry: AnIllustrated Colour Text, published by Churchill Livingstone (Elsevier), which has sold morethan 30,000 copies and has been translated into French, Spanish, Italian, Portuguese,Chinese, Japanese and Greek. You can find out more about him and his work atwww.allangaw.comi
ii
CASE STUDIES INCLINICAL BIOCHEMISTRYMichael J. MurphyRajeev SrivastavaAllan Gawiii
First published 2012By SA PressSAPress42@gmail.comPrinted and bound in the United Kingdom by Clydeside Press 2012 Michael J. Murphy, Rajeev Srivastava and Allan GawAll rights reserved. No part of this book may be reprinted or reproduced or utilisedin any form or by any electronic, mechanical, or other means, now known or hereafterinvented, including photocopying or recording, or in any information retrieval system,without permission in writing from the publishers.British Library Cataloguing in Publication DataA catalogue record for this book is available from the British LibraryISBN 978-0-956-3242-4-5The publisher and the authors have no responsibility for the persistence or accuracy ofURLs for external or third party internet sites referred to in this book, and do notguarantee that any content on such websites is, or will remain, accurate orappropriate.NoteKnowledge in all the areas of medicine described in this book is constantly changingand improving. As new research and experience broaden our knowledge, changes inpractice, investigation, treatment and drug therapy may become necessary orappropriate. Readers are advised to check the most current information provided (i)on procedures featured or (ii) by the manufacturer of each product to beadministered, to verify the recommended dose or formula, the method ofadministration and contraindications. It is the responsibility of the practitioner, relyingon their own experience and knowledge of the patient, to make diagnoses, todetermine dosages and the best treatment for each individual patient, and to take allappropriate safety precautions. To the fullest extent of the law, neither the publishernor the authors assume any liability for any injury and/or damage to persons orproperty arising out of, or related to, any use of the material contained in this book.The Publisheriv
DedicationFor those who taught us –our teachers, our students and our patients.v
CONTENTSDEDICATION . VPREFACE . VIIACKNOWLEDGEMENTS . IXHOW TO USE THIS BOOK . XGLOSSARY. XIFLUID AND ELECTROLYTE DISORDERS . 1ACID-BASE . 9RENAL . 19CALCIUM AND BONE DISEASE . 27LIVER FUNCTION . 35THYROID FUNCTION . 43ADRENAL FUNCTION . 51DIABETES . 59PITUITARY FUNCTION . 69LIPIDS . 73TOXICOLOGY. 79PAEDIATRICS . 83MISCELLANEOUS . 89APPENDIX- ACID BASE STRATEGY . 109SUGGESTIONS FOR FURTHER READING . 110USEFUL WEBSITES. 116vi
PREFACEThis book is for those studying Clinical Biochemistry as part of theirmedical, nursing or biomedical science courses. It will also be an excellentrevision aid for those preparing for post-graduate and professionalexaminations such as the MRCP. What it is not is a textbook of ClinicalBiochemistry – we have already written that and it is now in its 4th edition.Although that book – Clinical Biochemistry: An Illustrated Colour Text –contained clinical case studies many of our readers and our students haveasked for more to use as additional learning aids and for revision inpreparation for examinations.In response, we have prepared acomprehensive set of clinical cases with answers and explanations thatcover a range of topics in our subject.We have assumed throughout that you have already studied each of thetopics and are ready to put your knowledge into practice. ClinicalBiochemistry is about physiology and pathology and, above all, thepractice of medicine. It is a vital component of modern diagnostics andpatient management. Unless we have a thorough understanding of the useof biochemical tests in clinical practice we will ultimately fail to do the bestfor our patients.The clinical cases in this book are all based on real life patients and eachpresents a challenge, just as every patient we encounter in practice may bethought of as a puzzle to be solved. By looking at biochemical results inthe context of a clinical history, examination findings and other diagnosticinformation we can begin to unravel the puzzle before us. If we haveenough information we can propose a differential diagnosis, a treatmentplan and a prognosis.For each case we provide a solution to the problem and we giveexplanations for each of our answers to aid your learning and revision.We have not dwelt on laboratory practices preferring to place our subjectfirmly in the clinical arena where it belongs. Of course, what happens inthe laboratory – how we perform the tests and how we ensure their quality– is of paramount importance, but it need not be the concern of mostclinicians requesting biochemical services. They should be able to take thevii
excellence of the laboratory service for granted, and be able to focus onthe clinical problems for which they are seeking help.As such, in this book, you will not find questions about how to measureblood glucose or plasma cholesterol or urinary creatinine, but you will beasked to interpret the results of such analyses in their clinical context.Finally, if you wish to explore further any of the topics dealt with in thisbook, we have also included a list of useful additional resources (booksand websites) that provide detailed specialist coverage.Michael J. Murphy, Rajeev Srivastava & Allan GawDundee, Glasgow & Belfast, 2012viii
ACKNOWLEDGEMENTSThe idea for this book of case studies in Clinical Biochemistry came outof discussions with colleagues and students over a number of years. Inparticular, we must acknowledge the debts we owe to: Michael Burns and Laura Hughes, who kindly read andcommented on early drafts of the case studies and answers in thisbook. Peter Galloway and Colin Fletcher for their help and advice insourcing appropriate case material. Liz Ronald for her help in taking this manuscript from its firstdrafts to the finished book. David Tolmie for his help with the cover design. Anne Hicks for preparing the Kindle version of the book.Despite their valuable input we emphasise, however, that any factualerrors or pieces of clumsy prose that remain are entirely our own.Finally, we would like to thank our editor at SA Press, Moira Mungall,who with the use of carrots and sticks in equal measure encouraged us tofinish this book.ix
HOW TO USE THIS BOOKThis book is designed to be very simple to use. On each odd-numberedpage you will find a clinical case study. This will usually consist of a shortclinical history, some clinical findings, some biochemical results and somequestions. For each case you are asked to consider your answers and thenyou can compare yours with ours. You do not have to rummage in theback of the book matching case numbers to answers – finding thesolutions is as simple as turning the page, for you will find our solutionsand their explanations overleaf on each even-numbered page.To interpret any biochemical results you will need to have access toappropriate reference ranges. For the results in this book we haveprovided these in brackets after each result. While this is repetitious, itavoids you having to search for a list of reference ranges every time youneed one. Please remember, however, that reference ranges vary fromlaboratory to laboratory. When evaluating biochemical results you shouldalways use the ranges published by the institution performing the analyses.If in doubt contact your local laboratory for further information.We have also used the convention throughout of a capital ‘L’ to denotelitre. This is simply to avoid any confusion with a lower case ‘ l ’ and thenumber ‘ 1 ’. As you can see they are very similar. Unless otherwise statedall results are from analyses of venous blood.x
GLOSSARYA&EAccident and EmergencyACTHAdrenocorticotrophic HormoneADHAnti-diuretic HormoneAlk PhosAlkaline PhosphataseALTAlanine AminotransferaseASTAspartate AminotransferaseAVPArginine VasopressinBMDBone Mineral DensityBMIBody Mass IndexBNFBritish National FormularyBPBlood PressureCA-125Carbohydrate Antigen-125CAHCongenital Adrenal HyperplasiaCBDCommon Bile DuctCKDChronic Kidney DiseaseCOPDChronic Obstructive Pulmonary DiseaseCNSCentral Nervous SystemCRPC-reactive ProteinDDAVPDesmopressin – Synthetic Arginine VasopressinDHADehydroepiandrosteroneeGFREstimated Glomerular Filtration RateE2OestradiolESRErythrocyte Sedimentation RateFAOFatty Acid Oxidationxi
GLOSSARYf T4Free ThyroxineFSHFollicle Stimulating HormoneGGTGamma-glutamyl TranspeptidaseGnRHGonadotrophin Releasing HormoneGPGeneral Practitioner[H ]Hydrogen-ion ConcentrationHbHaemoglobinHGHHuman Growth HormoneIEMInborn Errors of MetabolismIFGImpaired Fasting GlycaemiaIGF-1Insulin-like Growth Factor-1IGTImpaired Glucose ToleranceIMIntramuscularITUIntensive Therapy UnitIVIntravenousK Potassium-ionLFTLiver Function TestsLHLuteinizing HormoneMIBGMeta-iodobenzylguanidineMRIMagnetic Resonance ImagingmmHgMillimetres of MercuryMSHMelanocyte Stimulating HormoneNa Sodium-ionpHNegative Log of Hydrogen-ion Concentrationxii
GLOSSARYPSAProstatic-specific AntigenPTHParathyroid HormonePTHRPPTH-related PeptidePCO2Partial Pressure of Carbon DioxidePO2Partial Pressure of OxygenSDStandard DeviationSHBGSex Hormone Binding GlobulinSIADSyndrome of Inappropriate AntidiuresisT4ThyroxineTFTThyroid Function TestsTRHThyrotrophin Releasing HormoneTSHThyroid Stimulating HormoneU&EUrea and ElectrolytesWCCWhite Cell Countxiii
xiv
FLUID AND ELECTROLYTE DISORDERSCASE 1An 82-year-old woman is discovered by her family, lying on the floor athome. She is found to have a left hemiparesis and a stroke is diagnosed.Clinical assessment of her volume status indicates dehydration: pulse 112beats per minute, blood pressure 95/65 mmHg, lax skin and dry tongue.The following biochemical results were obtained on admission:Na K UreaCreatinineGlucose169 mmol/L3.9 mmol/L23.5 mmol/L160 µmol/L7.6 (a) Describe and comment on the biochemical abnormalities.(b) Give an assessment of the patient’s water status and sodium status.(c) In the light of your answer to the previous question, predict the urineosmolality and urinary sodium concentration.(d) How would you treat her fluid/electrolyte status?1
FLUID AND ELECTROLYTE DISORDERSANSWER 1(a)Severe hypernatraemia; urea and creatinine also raised, urea morethan creatinine. These biochemical abnormalities are frequently seenin clinical scenarios where fluid intake is reduced (as here), or, lessfrequently, when fluid loss is increased. Glucose is raised but mayjust reflect insulin resistance acquired from the stress response,which is associated with increased concentrations of anti-insulinhormones like cortisol and adrenaline.(b)Water status is reduced; the evidence for this is primarily clinical(tachycardia, hypotension), reflecting reduced extracellular fluid(ECF) volume, although the greater rise in urea (compared withcreatinine) is also consistent with dehydration. Patients are often lessclinically dry than expected given the severity of the hypernatraemia.This is because water loss is distributed across all bodycompartments. Na intake will have been reduced for the samereason as water intake. However, some of the homeostaticmechanisms designed to protect blood volume (secondaryhyperaldosteronism) minimise Na loss, even as insensible losses ofpure water from respiration continue. Hence the relative loss ofmore water than Na , as evidenced by high serum Na concentration.(c)Urine osmolality will be high ( 600 mmol/kg), reflecting urineconcentration due to ADH secretion, stimulated by hypovolaemia(non-osmotic stimulus) and hypernatraemia (osmotic stimulus).Urinary Na concentration will be very low ( 10 mmol/L)reflecting sodium retention due to secondary hyperaldosteronism,precipitated again by hypovolaemia.(d)She needs water and was given 5% dextrose IV (she could not drinkinitially). This is isotonic with plasma; pure water would precipitateintravascular haemolysis because of the osmotic difference acrossred cell membranes. Isotonic (0.9%) saline replaces both Na andwater and does not correct a primary water deficiency.2
FLUID AND ELECTROLYTE DISORDERSCASE 2A 64-year-old male smoker presents with unintentional weight loss of 20kg over three months. On review of systems he admits to intermittent drycough. On chest examination he has signs consistent with left lower lobeconsolidation; water (volume) status is unremarkable. Chest X-rayconfirms consolidation and also reveals hilar lymphadenopathy. Lungcancer was provisionally diagnosed. Before bronchoscopy, urea andelectrolytes were measured:Na K UreaCreatinine124 mmol/L3.5 mmol/L5.8 mmol/L110 µmol/L(135-145)(3.4-4.9)(2.5-8.0)(40-130)(a) Describe and explain the biochemical abnormalities.(b) Give your assessment of his water and sodium status.(c) How would you treat his fluid and electrolyte abnormalities?3
FLUID AND ELECTROLYTE DISORDERSANSWER 2(a)The patient has hyponatraemia; potassium is low-normal.Importantly serum urea and creatinine are within the respectivereference ranges, suggesting that glomerular function is normal.(b)Water status is probably increased. Why? The most importantinformation here is his volume status, reportedly ‘unremarkable’ –effectively telling you that he is neither dry nor oedematous – inturn excluding sodium depletion and effective circulating volumedepletion as the basis for his hyponatraemia. In the context of theinformation provided, the syndrome of inappropriate antidiuresis(SIAD) should be suspected. ADH secretion stimulated by nonosmotic stimuli causes water to be retained, causing a ‘dilutional’hyponatraemia. The cause of SIAD here is likely to be lungcancer, although other chest pathologies may also cause it.Volume status may be unremarkable because the water excess isdistributed evenly across all body compartments. He probably hasrelatively normal sodium status – there is no informationsuggesting a reason for this to be altered.(c)Symptoms of hyponatraemia (usually neurological) do not usuallydevelop if sodium is much above 120 mmol/L. If intravenousfluids are required to correct severe hyponatraemia, isotonic(0.9%) saline is preferred; this helps to restore the balance ofsodium and water (reduces relative sodium deficit). Less severehyponatraemia due to SIAD is treated with fluid (water)restriction (usually to less than a litre a day). This effectivelyrequires hospital admission since it is virtually impossible tosupervise elsewhere. In this case it would be reasonable tomonitor sodium and admit for treatment only if sodium fell to 120 mmol/L and/or the patient developed symptoms ofhyponatraemia.4
FLUID AND ELECTROLYTE DISORDERSCASE 3A 25-year-old male cyclist is admitted to a neurosurgical unit aftersustaining severe head injuries in a road traffic accident. He developspolyuria (urine output in excess of 15 L) over the next 24 h. Serum sodiumclimbs from 148 mmol/L on admission, to 168 mmol/L on day 4, atwhich point a spot urine osmolality is 80 mmol/kg.(a) What is the diagnosis?(b) How would you treat his hypernatraemia?5
FLUID AND ELECTROLYTE DISORDERSANSWER 3(a) Cranial diabetes insipidus. This patient has sustained traumatic damageto his posterior pituitary gland (which produces ADH). As a result heis unable to retain water. The diagnosis can effectively be made on thebasis of the history. The urine osmolality simply confirms his inabilityto concentrate urine (urine osmolality should be well in excess of 600mmol/kg in the face of severe hypernatraemia as here).(b) He is losing large amounts of (almost pure) water and requires waterto be replaced. As he is unconscious this cannot be given orally andmust be given intravenously as 5% dextrose. The rate at which thisshould be given will be determined by his urine output. He will alsorequire exogenous ADH since he is unable to produce this himself.This is given as the vasopressin analogue DDAVP (AVP stands forarginine vasopressin, another name for ADH). This can beadministered in a number of ways depending on the clinical context:as nasal drops, orally or by injection (IV or IM).6
FLUID AND ELECTROLYTE DISORDERSCASE 4A 77-year-old woman with a history of stroke attends the hypertensionclinic; she is on four antihypertensive drugs. Ambulatory blood pressuremonitoring confirms refractory hypertension with mean daytime readings172/98 mmHg. Furosemide 40 mg daily is added, and magnetic resonanceangiography requested to exclude renal artery stenosis. Three days afterfurosemide is added, an out-of-hours doctor is called to see her. She isclearly unwell and unable to give a clear history. Her daughter reportsincreasing forgetfulness over the previous few months. On examinationshe is clearly dehydrated with lax skin and dry mucosa. Serum urea andelectrolytes are as follows:Na K UreaCreatinine127 mmol/L3.2 mmol/L15.0 mmol/L140 µmol/L(135-145)(3.4-4.9)(2.5-8.0)(40-130)(a) Describe and comment on the biochemical abnormalities.(b) Give your assessment of the patient’s sodium and water status.(c) How would you treat this patient?7
FLUID AND ELECTROLYTE DISORDERSANSWER 4(a) The patient has hyponatraemia and hypokalaemia and evidence ofreduced glomerular function in the form of raised urea and creatinine.The most likely explanation is that she has inadvertently overdosed onher furosemide, resulting in excessive natriuresis and resultant diuresis.(b) Total body water and sodium are likely to be decreased. This caseillustrates a golden rule of sodium and water balance: water followssodium everywhere. It also illustrates the diagnostic value of clinicaldehydration in the context of hyponatraemia. Where there is clearevidence of decreased water status from clinical dehydration, thefinding of a reduced ratio of sodium to water is diagnostic of sodiumdepletion – it allows for no other interpretation. Furosemide inhibitsreabsorption of sodium and chloride in the ascending loop of Henlé(hence the term: loop diuretic) and distal renal tubule; it also blocks achloride-binding co-transport system. The effect is increased excretionof water, sodium, chloride, magnesium, and calcium.(c) She requires rehydration. Since she is sodium depleted, fluidresuscitation should take the form of intravenous isotonic (0.9%)saline initially.8
ACID-BASECASE 5A 78-year-old man is admitted to hospital as an emergency because ofhaematemesis. On arrival he is clinically shocked with pulse rate 112 beatsper minute and blood pressure 90/65 mmHg. His admission blood resultsare:Urea and ElectrolytesNa K ClHCO3UreaCreatinine143 mmol/L3.6 mmol/L96 mmol/L5 mmol/L13.8 mmol/L130 40-130)Arterial Blood GasesH PCO2PO297 nmol/L2.7 kPa16.1 kPa(35-45)(4.5-5.6)(12-15)(a) Classify the acid-base disorder.(b) Explain the results.(c) Is there anything else you would wish to measure?9
ACID-BASEANSWER 5(a) [H ] is grossly elevated indicating a severe acidosis. Bicarbonate andPCO2 are low, the bicarbonate much more profoundly. A lowbicarbonate is defined as a metabolic acidosis; a low PCO2 defined as arespiratory alkalosis. The metabolic acidosis must therefore beprimary, and the respiratory alkalosis compensatory. So: partiallycompensated metabolic acidosis.(b) The history provides a clear indication of the cause of the metabolicacidosis. The patient is reported to be clinically shocked, indicatinglack of perfusion of his tissues (invariably seen in severe blood loss, aswith haematemesis). This means that the tissues have to metabolisefuel in the absence of oxygen, resulting in production of lactate.Lactate is acidic, dissociating H and thereby releasing an acid loadinto the circulation. The law of mass action results in the followingreaction being driven to the right: H HCO3- H2CO3 H2O CO2. This results in the production of PCO2, which has to be blownoff (hence acidotic or Kussmaul breathing).(c) Only two things cause severe metabolic acidosis with any frequency:ketoacidosis and lactic acidosis. So you need to measure ketones andlactate. Ketoacidosis is mostly associated with diabetes mellitus,especially type 1, but can also be seen in alcoholic patients (alcoholicketoacidosis) and in biochemical starvation. In practice you woulddipstick his urine for ketones, rather than quantifying them in blood(although increasingly clinicians do exactly that in managing diabeticketoacidosis). Do not forget that someone as ill as this patient mayhave slightly raised glucose due to the anti-insulin hormonesassociated with severe physiological stress (cortisol, adrenaline, growthhormone), and indeed might also be mildly ketotic if he had not eatenfor a while. If diabetic ketoacidosis were to explain these results, youwould expect the glucose to be very high and the urine to be stronglypositive for ketones (at least three or four pluses). Practical point:lactate is collected into the same specimen type as glucose. Thispatient’s lactate was 19.0 mmol/L (reference range 2 mmol/L).10
ACID-BASECASE 6A 63-year-old man is brought to Accident and Emergency after he goesinto cardiorespiratory arrest while eating out in a restaurant. On arrivalresuscitation measures are continued and the patient is briefly stabilised;venous and arterial blood samples are collected. The results of the arterialblood gases are shown below.H PCO2HCO3PO2132 nmol/L14.6 kPa8.5 mmol/L9.2 kPa(35-45)(4.5-5.6)(21-28)(12-15)(a) Describe the acid base abnormalities.(b) Discuss the pros and cons of administering bicarbonate to treat aprofound acidosis as here.11
ACID-BASEANSWER 6(a) This set of arterial blood gases is typical of a patient in extremis. [H ] isgrossly elevated (i.e. profound acidosis). The clinical context is ofcardiorespiratory arrest, so logically it does not matter which of PCO2or bicarbonate is examined next. As anticipated in respiratory arrest,the PCO2 is grossly elevated, reflecting severe respiratory acidosis. Thebicarbonate is very low, indicating a severe metabolic acidosis. Thefact that both components of the ratio in the Henderson-Hasselbalchequation have changed in opposite directions indicates that we havetwo primary processes occurring simultaneously. This is therefore amixed acid-base disturbance. This picture is a (profound) mixedrespiratory and metabolic acidosis.(b) An acidosis of this severity is life-threatening, irrespective of itsunderlying cause. It would be logical in this clinical context toadminister IV bicarbonate in an attempt to normalise the [H ].Indeed, this used to be part of the management of acute cardiac arrest.However, its use has been discontinued on the grounds that there isno evidence of clinical benefit; indeed patients treated in such a waymay do worse. This has been postulated to be due to either‘overshoot’ alkalosis (unlikely in this case with severe acidosis) orhypercapnia (due to the increased production of CO2 from [H ] and[HCO3-]), which requires adequate ventilation for elimination.12
ACID-BASECASE 7A 57-year-old man is admitted because of breathlessness and wheezing.He is known to suffer from chronic obstructive pulmonary disease;medications included inhalers and oral prednisolone. He is also a heavysmoker. On examination, he is breathless, cyanosed and pyrexial. His chestis hyper-resonant and he has generally decreased air entry with bilateralwheeze and coarse crepitations on the right side. Chest X-ray showsprobable collapse of the right upper lobe and emphysematous changes.Arterial blood gases on air show:H PCO2HCO3PO256 nmol/L11.3 kPa36 mmol/L7.1 kPa(35-45)(4.5-5.6)(21-28)(12-15)(a) Describe the acid base abnormality.(b) What background acid-base picture might you anticipate if he wasnot acutely breathless?(c) Make up a set of acid-base results that would be consistent with youranswer to part (b).13
ACID-BASEANSWER 7(a)[H ] is raised, indicating an acidosis. PCO2 is raised indicatingrespiratory acidosis. Bicarbonate is elevated indicating metabolicalkalosis. Thus, the respiratory acidosis must be primary and themetabolic alkalosis compensatory. So, partially compensatedrespiratory acidosis.(b)It is worth delving more deeply into his acid-base status. His historyof COPD means that you would expect him to have a backgroundrespiratory acidosis (raised PCO2), and if he was stabilised ontreatment, you would expect this to be completely (or almostcompletely) compensated (raised bicarbonate). So, a compensatedrespiratory acidosis is the most likely background picture.(c)H PCO2HCO3PO244 nmol/L8.0 kPa33 mmol/L7.1 kPa(35-45)(4.5-5.6)(21-28)(12-15)These figures represent a compensated respiratory acidosis. H ,PCO2 and bicarbonate are related mathematically in the HendersonHasselbalch equation, and if the H and PCO2 are measured (whichthey are) then the bicarbonate concentration can be deduced. Thisis exactly what blood gas analysers do; hence the term ‘standardisedbicarbonate’ – it indicates that the machine has calculated, ratherthan measured, the bicarbonate.14
ACID-BASECASE 8An 80-year-old woman is admitted with a myocardial infarction. She isnot shocked or hypotensive. She is on acetazolamide for glaucoma.Urea and ElectrolytesNa 139 mmol/LK 4.5 mmol/LCl116 mmol/LHCO312 mmol/LUrea10 mmol/LCreatinine120 40-130)Arterial Blood GasesH 59 nmol/LPCO23.9 kPaPO210.0 kPa(35-45)(4.5-5.6)(12-15)(a) Define the acid-base abnormality.(b) Why have chloride and bicarbonate been measured?(c) Can you suggest a diagnosis?15
ACID-BASEANSWER 8(a)[H ] is elevated indicating an acidosis. Bicarbonate and PCO2 arelow, the bicarbonate more so. A low bicarbonate is a metabolicacidosis, a low PCO2 is a respiratory alkalosis. So the metabolicacidosis must be primary, and the respiratory alkalosiscompensatory. Partially compensated metabolic acidosis. This caseis similar to, but much less severe than, the example given in Case 5.(b)Chloride and bicarbonate have been measured to allow the aniongap to be calculated. This is a biochemical tool that can be helpful infinding the cause of a metabolic acidosis. Essentially, it is thedifference between the two main cations in the blood (Na and K )and the two main anions (Cl- and bicarbonate): [Na K ] - [Cl- HCO3-]. K is sometimes omitted because it’s present in smallconcentrations. What does the anion gap tell you? If it is high(which it usually is) then not very much. However, if it is normal (816 mmol/L), the list of causes is much smaller, and it is thereforemuch more useful. This list includes renal tubular acidosis andchronic diarrhoea or intestinal fistula.(c)The finding of a normal anion gap, and the knowledge that thepatient was on acetazolamide for her glaucoma, provides theexplanation.
Biochemistry – we have already written that and it is now in its 4th edition. Although that book – Clinical Biochemistry: An Illustrated Colour Text – contained clinical case studies many of our readers and our students have asked for more to use as additional learni