Transcription
Diabetes EducationWorkbookTAKE HOME GUIDE FOREFFECTIVE MANAGEMENT
2
The information contained in this packet isfor MRMC patient education and notintended for distribution. Any and alldissemination of this information, byphotocopy or otherwise, is strictlyprohibited.Produced by Maury Regional Medical CenterNursing Professional DevelopmentAugust 2013Printed with permission
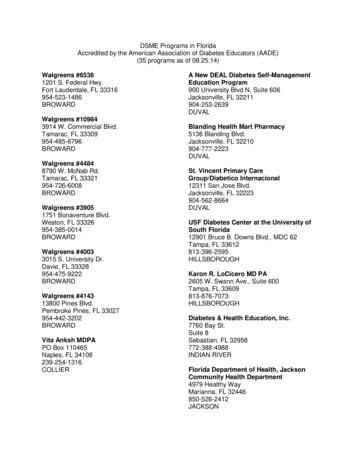
Table of ContentsTopicLong Term ComplicationsPages5-12Hemoglobin A1c12-16What is diabetes?18-23Why check blood glucose?24-25Using a meter26Preparing and giving insulin27-34Low blood sugar symptoms and treatment35-38High blood sugar symptoms and treatment39-41Meal/Carbohydrate plan42-48Why do you need to exercise?49-50Wearing Medical ID51Free Diabetes Medical Alert Coupon53Sick day rules55-56Family Risk Assessment57-63Nutrition Management Plan64-66Outpatient Diabetes Programs67-68Diabetes: 5 ways to be active in yourcare at the hospital69-72Diabetes Medications Fact Sheet73-75Sources764
Long Term Complicationsfrom DiabetesPoorly controlled diabetes will influenceyour quality of life. It will also lead to longterm complications that cannot be reversed. Ifyou experience any of these problems, reportthem to your doctor immediately to preventfurther damage.Blood Vessel DiseasesHeart Disease:Coronary artery disease (CAD) is the termfor the progressive closure of the arterieswhich supply blood to the heart muscle. Whenone or more of these arteries completelycloses, the result is a heart attack. Symptomsof a heart attack can include chest pain; painthat radiates to the arms, neck, and/or jaw;nausea/vomiting; and/or sweating.Cerebrovascular Disease:This is a disease of the arteries5
that supplies the brain with oxygen and othernutrients. If a major artery to the braincompletely closes, the person suffers a stroke.Symptoms of stroke can include one sidednumbness or weakness, sudden confusion,sudden severe headache, trouble speaking,trouble seeing, sudden trouble walking or lossof balance and coordination, and facial droop.Peripheral Vascular Disease (or PVD):The same process thataffects the arteries in the heartand brain can also affect thearteries to the rest of the body.After ten years of diabetes, athird of men and women nolonger feel a pulse in their feetbecause of this disease. Themost common symptom of PVD is pain in thecalves, thighs, or buttocks that begins aftersome walking and stops with rest.If you have any of these symptoms ofblood vessel disease, notify your doctorimmediately. Symptoms of heart disease orcerebral vascular disease are medicalemergencies and need to be treated promptly.6
In order to prevent damage to these bloodvessels it is very important for you to controlyour: blood pressure cholesterol glucose weightYou should also exercise and not smoke or useother tobacco products.To help prevent these complications:have your blood pressure checked eachtime you visit your doctormonitor your blood glucose at home daily;your doctor will do a hemoglobin A1c test(3 month average of blood glucose) every3-6 months to see how well your glucoseis being controlledcheck your weight at every doctor’sappointmentget your cholesterol checked yearlyFoot Care:Diabetes is the leading cause of nontraumatic lower limb amputations.7
Amputations and foot ulcers are the mostcommon consequence of diabetic peripheralneuropathy (nerve damage caused by highblood glucose).Wash your feet daily and dry your feetthoroughly—especially between the toes.Inspect your feet daily by looking at both feet(top, bottom, sides, and between the toes) forredness, swelling, and any other sign of skinproblems. Look for cuts, calluses, blisters, andthick or ingrown toenails. If you’re unable tobend over to see the bottom or sides of yourfeet, use a hand mirror to check for problems.Call your doctor immediately if you notice anyproblems.Cut toenails straight across and file thesharp corners to match the contour of the toe.Make sure your shoes fit well and wear cleansocks every day. Avoid going barefoot or sockfooted. Wear foot wear at the pool or beach.Inspect your shoes daily by feeling inside theshoe for torn linings, cracks, pebbles, nails, orother objects that may irritate the skin.8
Eyes:Diabetes is the leading cause of visual lossin the United States. The eyes are affected bydiabetes over the long term. Althoughglaucoma (high pressure in the eye) andcataracts (a film over the lens in the eye)occur in non-diabetic patients, they appearsooner and more frequently in patients withdiabetes.Retinopathy refers to changes seen on theretina of the eye indicating that the patient hashad high blood glucose over time. If untreated,retinopathy can lead to blindness.High blood pressure, tobacco products, anddrinking alcohol may worsen retinopathy. Seeyour eye doctor at least yearly for a dilated eyeexam. If you notice sudden visual changes,sudden flashes of light in one or both eyes, ashadow or curtain on part of your visual field,or eye pain, contact your eye doctorimmediately.9
Kidneys:Your kidneys have about amillion tiny filters that rid yourbody of harmful waste products.These waste products areeliminated through the urine.The kidneys regulate the salt and watercontent of your body. Glucose is also filteredthrough the kidneys.Several years of high blood glucose willeventually lead to damage to this filteringsystem leading to kidney failure. When kidneydisease (nephropathy) causes your kidneys tofail, you must either have a kidney transplantor go on dialysis.In addition to high blood glucose, otherfactors that will contribute to the continuingdestruction of the kidneys include high bloodpressure, high cholesterol, and family historyof kidney disease. If you experience kidneydisease from diabetes, you increase your riskof developing other complications. These othercomplications include diabetic eye disease,diabetic nerve damage (neuropathy), highblood pressure, and edema.10
To prevent damage (or further damage) toyour kidneys, it is important to keep yourblood glucose, blood pressure, and cholesterolunder control. Your doctor will do a lab testcalled microalbumin every year to check forkidney damage.Teeth:Diabetes is one of the leadingcauses of oral health problemslike dry mouth and gingivitis which isthe result of plaque and tartar buildup and is amajor cause of tooth decay. Plaque and tartarinflame the gums and bacteria causes thegums to become infected, swollen, and tender.If left untreated, gingivitis progresses toperiodontal disease. This is the breakdown ofthe structures that support the teeth—thegums and bone. Regular dental exams—atleast twice a year—should be used asopportunities for prevention, early detection,and treatment of oral health problems.11
Skin:Certain skin ailments,such as bacterial andfungal infections, aremore common in diabetes.Slow wound healing indiabetes is a frequentcause of developinginfections. The besttreatment for management of diabetic skinconditions is to bring blood glucose levelsunder control. Weight loss is also helpful formany of these conditions.Be sure to test the temperature of bathsand showers with an elbow before stepping into avoid burns from water that is too hot.Moisturize dry skin (except between the toes)but avoid lotions that contain alcohol since thiscan dry the skin.Controlling blood glucose, cholesterol, andweight will help to reduce the risk of many ofthese complications. Not using tobaccoproducts is also very important for your longterm health and use of alcohol should belimited.12
Hemoglobin A1cHow does it work?Hemoglobin is found inside red blood cells. Itsjob is to carry oxygen from the lungs to all thecells in the body. When diabetes isuncontrolled, you end up with too muchglucose in the bloodstream. This extra glucoseenters your red blood cells and attaches tohemoglobin. The more excess glucose in yourblood, the higher the hemoglobin A1c testresult will be.Checking your blood glucose at home with ameter tells you what your blood sugar levels isat any one time, but suppose you want toknow how you're doing overall. The A1c testgives you a picture of your average bloodglucose control for the past 2 to 3 months. Theresults give you a good idea of how well yourdiabetes treatment plan is working.In some ways, the A1c test is like a baseballplayer's season batting average, it tells youabout a person's overall success. Neither asingle day's blood test results nor a single13
game's batting record gives the same bigpicture.How does the A1C test look backward?This lab result changes as old red blood cells inyour body die and new red blood cells (withfresh hemoglobin) replace them. The amountof A1c in your blood reflects blood sugarcontrol for about the past 120 days, or thelifespan of a red blood cell.For someone with diabetes and high bloodglucose levels, the A1c level is higher thannormal. How high the A1c level rises dependson what the average blood glucose level wasduring the past weeks and months.You should have your A1c level measuredwhen your diabetes is diagnosed or whentreatment for diabetes was started. To watchyour overall glucose control, your doctorshould measure your A1c level at least twice ayear. There are times when you need to haveyour A1c level tested about every 3 monthssuch as if you change diabetes treatment, starta new medicine, or if you are not meeting yourblood glucose goals. You and your doctor will14
want to keep a close eye on your overallcontrol.What are the limitations?Although the A1c test is an important tool, itcan't replace daily self-testing of blood glucosefor those who need it. A1c tests don't measureyour day-to-day control. You can't adjust yourinsulin on the basis of your A1c tests. That'swhy your blood sugar checks and your log ofresults are so important for staying in effectivecontrol.Points to remember:The A1c test measures your average bloodglucose control for the past 2 to 3 months.Check your A1c twice year at a minimum,or more frequently when necessary.It does not replace daily self-testing ofblood glucose.If your nurse or physician has notcommunicated the results of your most recentA1c, please ask them for that information.15
Hemoglobin A1c results are measured inpercentages. Compare your results to the chartto determine your average blood glucose forthe past 3 months.Your hemoglobin A1c is: %.How does your A1c compare for degree ofcontrol and health risk on the chart below?A1c %Average BloodGlucose (mg/dl)Degree of controlHealth Risk 6135Very excellentVery low789101112 13170205240275310345380ExcellentGoodFairPoorVery poorExtremely poorExtremely poorLowGoodMediumHighVery highExtremely highExtremely highA1c—5.6% or less normalA1c 5.7-6.4% borderline or pre-diabetesA1c 6.5% or higher diabetesIf your A1c is 9%, speak with the physicianwho manages your diabetes about how to getbetter control of your blood glucose to helplower your A1c. The lower your A1c number,the lower the risk for complications fromdiabetes such as kidney failure, blindness,amputations, strokes, and heart attacks.16
10 SURVIVALSKILLSPREPARING YOU TOLIVEWITH DIABETES17
1. What is diabetes?Diabetes is a condition that affects how wellyour body uses food, particularlycarbohydrates.When you eat carbohydrates, your bodybreaks it into a sugar called glucose. Insulin, ahormone made by your pancreascarries the glucose into the cell where it isused for energy.Diabetes is a result of absent or reducedinsulin, or insulin not used well by the body.This causes blood sugar, or glucose, to rise18
above normal. There are three main types ofdiabetes:Type 1:The body does not make any insulin ormakes very little insulin. These peoplemust take 2 or more insulin shotseveryday to live.The cause of type 1 could be a historyof diabetes in the family, a virus thatinjures the pancreas, or the body’simmune system may mistakenly destroythe insulin-producing cells in the pancreas.Type 1, formerly known as “juvenilediabetes,” usually occurs in children andyoung adults.19
Type 2:The body does not make enough insulin orthe body is not using it properly and the cellshave become resistant.Ways to control type 2 diabetes include:dietexerciseoral diabetic medicinesand/or insulin.20
Risk factors include:a family history of type 2being overweight or obesephysical inactivitya history of gestational diabetes ordelivering a baby that weighs greaterthan 9 poundsbeing over 45 years oldcertain high-risk ethnic or racial groupssuch as: African-American Native-American Hispanic21
Children can also have type 2 diabetesbecause of theirdiets,obesity,and/or lack of exercise.Both type 1 and type 2 diabetes cannot becured and do not go away, but both types canbe managed to the point that you can live anormal life.22
Gestational:This is a type of glucose intolerance duringpregnancy. The hormones produced duringpregnancy can cause the body to become lesssensitive to insulin. Usually after delivering thebaby, the blood glucose will return to normalfor the mother.The obstetrician should do a test forgestational diabetes around the 24th-28th weekof pregnancy.Having gestational diabetes can increaseyour risk for developing type 2 diabetes later.23
2. Why check blood glucose?Checking your blood sugar often allows thedoctor to decide if the meal plan, exercise,and/or medications are working together tocontrol your diabetes.You should check blood glucose 2-4 times aday. Best times to check are:“Fasting” is before the first meal of theday—tells how your body has utilized theglucose during the night;2 hours after meals—tells how your body isusing the glucose from the meal just eaten;Sick or strange feeling—could signal a needto treat a high or low blood sugar, or theneed to call your doctor for an illness;Before and after exercise—to see howmuch exercise will decrease your bloodsugar;Before bedtime—blood glucose should bearound 100 before bedtime.24
If the doctor doesn’t give a goal range, usethe ADA's ranges:70-130 fasting(before the first meal of the day) 180—2 hours after eatingYou do not need to use alcohol to cleanyour fingertips at home. Alcohol can cause a“false” reading (this is why we never use thefirst drop of blood in the hospital). Simplywashing your hands with soap and water isadequate.Diabetics have problems with dry skin andusing alcohol at home can cause even drierskin.25
3. Using a meter:Testing with your blood sugar meter isvery important for keeping track of day-to-dayblood sugar levels. Meters are generallyaccurate and precise, but mistakes can comefrom the person doing the blood checks.To avoid variations:Make sure you keep your meterclean.Don’t use strips that are out of date.Keep the meter and strips at roomtemperature.Record blood sugar readings in the logbookincluded in the kit. Take the logbook and meterto every doctor’s visit. The doctor will reviewthe logbook and adjust medicines or treatmentif needed.NEVER re-use a lancet. Staph is a bacteria thatnormally lives on the skin. Repeatedly using a lancet putsyou at risk for this serious skin infection. The needle of thelancet also becomes dull which increases the amount of painyou may experience when sticking your finger to get theblood sample.26
4. Preparing and giving insulin:You cannot live without insulin. If yourbody does not make enough insulin, you willneed to take insulin injections. Give insulinsubcutaneously into fatty tissue just under theskin. Give insulin through an injection with asyringe or insulin pen, or an insulin pump. Youwill measure insulin in units.Insulin is not available in pill form.Insulin affects different people indifferent ways, depending on factorssuch as:Fitness levelInsulin sensitivityActivity levelInjection siteFood and/or beverage intakeOther medicationsEmotions such as stress27
Many different kinds of insulin are availablewith different onsets, peaks, and durations.During your hospital stay, you will receiveteaching for insulin drawing up and injecting.Giving injections into the same spot cancause thickening of the skin. This makes itharder for the body to absorb the injectedinsulin. For this reason, you need to rotate thearea (or site) you use for injection.Sites should be about 1 inch apart. Do notinject into moles or scars. Use these sites forinjections:Do not change the amount of insulin youtake without your doctor’s approval.28
Using an Insulin PenInsulin pens come in different doses and aremade by several different companies. The pensare simple to use, and even young children orpatients with vision problems (such asblindness) can use them with ease. The basicsof using an insulin pen include:1.2.Screw on a new needle each time you givean injection. Remove the needle cover.Prime the pen to remove any air from thepen. Air will not hurt you but you may notget an accurate amount of insulin if you fail29
to prime the pen correctly each time. Asyou’re holding the pen away from yourface, turn the dial (or plunger) on the endof the pen to “2” and press the button (or“dial”) on the end of the pen.You should see a squirt, stream, orperhaps a drip of insulin come from theend of the needle. If you do not see thisafter pressing the button, dial the pen to“2” again and press the button on the endof the pen. Watch for the insulin.3.Now, turn the knob on the end of the pento the number of units that you will beinjecting.30
4.5.6.7.Hold the insulin pen in the palm of yourhand (as seen in the picture) with yourthumb on the ‘dial’ end of the pen.Insert the needle into your injection site.Press the button on the end of the pen. Ifyou hold the pen with the numbers facingtoward you, you will see the pen dial backdown to “0” as you’re giving the injection.Count to five.Remove the pen and dispose of the needlein a container. Most counties now allow theuse of a plastic container with a lid thatscrews on. If you aren’t sure what’sallowed in your area, check with your localhealth department.You will hear a ‘click’ from the pen as you’repriming the pen or dialing up the dose you will31
be taking. This is normal. Each ‘click’ is 1 unitof insulin.After your injection, you may notice aslight amount of dampness on the skin at theinjection site. This will be normal. However ifyou notice a large puddle or if you see insulinrunning down your arm, leg, or abdomen fromthe injection site, you might not have given theinjection correctly. Do not give anotherinjection but realize your blood sugar may behigh or higher than normal the next time youcheck it. If so, make sure you’re following allthe steps listed above. If you continue to havetrouble using the insulin pen, contact eitheryour doctor’s office or the drug store whereyou got your pen for further instructions.Drawing Up Insulin:1. Wash hands with soap and water.2. Wipe the top of the insulin bottle withalcohol.32
3. Fill the empty syringe with air equal to theamount of insulin you will take.4. Push the needle into the bottle. Keep thebottle in an upright position. Push the airfrom the syringe into the insulin bottle.This makes it easier to draw out theinsulin.5. Keep the needle in the bottle. Turn thebottle upside down. Pull the plunger back.Fill the syringe with the number of units ofinsulin you need.6. Look at the insulin in the syringe. If yousee air bubbles, push the insulin back intothe bottle and slowly draw it up again. Pullthe needle out of the bottle.Injecting insulin:1.2.Clean the injection site with soap andwater or an alcohol swab. Let the area dry.Remove the needle cover from the syringe.Hold the syringe like a pencil. Gently pinchup a fold skin at the injection site.33
3.4.5.6.Position the needle at a 90 degree angle(straight up and down). Insert the entirelength of the needle into the fold of skin.Let go of the pinched skin. Push theplunger all the way down.After injecting the insulin, slowly count to 5and pull the needle out.Put your needles in a covered punctureproof container.Check with your local waste authority orhealth department about the proper way todispose of your used needles and lancets.(For more information about diabetes medications,see pages 73-76.)34
5. Low blood sugar (hypoglycemia)symptoms and treatment:Consider a blood sugar of less than 70 toolow. You may feel symptoms before your bloodsugar reaches 70. The reasons for low bloodglucose are:Missed or delayed meal;or eating less than usual.More physical activity than usual.Taking too much insulin or otherdiabetic medications.Early warning symptoms can include:numbness or tingling around themouth or lipssweaty or clammy feeling hunger35
confusion dizziness or shaky feeling faster than normal heartbeat headachenervousness or irritabilityUntreated low blood sugar can lead toseizures, unconsciousness, or coma. If low36
blood sugar occurs more than twice a week,you should notify your doctor.When treating a low blood sugar, rememberthe RULE OF 15.1. Checkthe blood sugar. If less than70, eat or drink 15 grams of fastacting carbohydrates such as:3-4 glucose tablets7-8 Lifesavers4-5 pieces of hard candy(not sugar free)4 ounces of juice or regular softdrink (not diet)2. Wait15 minutes and re-check theblood glucose.37
3. Ifthe symptoms have not gone awayand/or the blood sugar is still less than70, eat or drink another serving fromthe list.4. Repeatuntil blood sugar is more than70.If it is going to be more than 30 minutesbefore your next meal, you need a snack withcarbohydrates and protein, such as ½sandwich or crackers with peanut butter orcheese. Do not give snacks until the bloodsugar is greater than 70 because the bloodsugar will not increase until the snack hasdigested.38
6. High blood sugar(hyperglycemia) symptoms andtreatment:High blood sugar is any number aboveyour target blood sugar range and can occurfor many reasons such as:Lack of exerciseSkipping diabetic medications and/orinsulinNot taking the right amount ofmedicationStressIllnessOver eatingNot following the meal plan39
Because high blood sugar usually happensslowly, the signs are not always easy to notice.Some of the symptoms include:feeling very thirstyhaving to go the bathroom oftenfeeling very tired or weakhaving blurred vision or problemsseeing40
What should you do if you’re having ahigh blood sugar?Call your doctor if:1.Test your blood sugar every couple ofhours.2.Eat your regularly planned meals.3.Keep taking your diabetes medicinesat the usual times.4.Drink plenty of sugar free liquids.Call your doctor if:1.You have vomiting or diarrhea formore than 6 hours.2.Your blood sugar is greater than 240before meals and stays there for morethan 24 hours.3.You have a fever for a couple of daysand aren’t getting any better.4.You just aren’t certain of what to doto take care of yourself.41
7. Meal/Carbohydrate plan:The old suggestions of just limiting foodsthat contain sugar have changed. There are nolonger any forbidden foods for a person withdiabetes.The American Diabetes Associationrecommends an eating plan for diabetes basedon MyPlate (see page 43 for example) for awell-balanced diet. Selecting foods from allfood groups gives you the nutrients needed tostay healthy. The meal plan should work wellwith your lifestyle and routine.When you have diabetes, you need aconsistent carbohydrate diet to maintainblood sugar control. A consistent carbohydratediet means you should have approximately thesame amount of carbohydrates each day.Carbohydrates are the nutrient that affectsthe blood sugar the most. Many of the foods42
you eat contain carbohydrates. They are animportant part of the diet since they give youthe glucose your body and brain need tofunction. Many of these foods also containimportant vitamins and minerals the bodyneeds to work well.Some examples of 1 serving (approximately15 grams) of carbohydrate are:Bread (1 slice)Crackers (4 to 6)Cereals (unsweetened, ¾ cup)Pastas (1/3 cup)Grains (1/2 cup)Milk (1 cup)Fresh fruits (1 small)Fruit juices (1/2 cup)Peas/Corn (1/2 cup)Mashed Potatoes (1/2 cup)Baked Potato (1 small, 3 ounces)All Desserts (portion sizes vary)43
Your weight, age, and activity level help todecide the total number of carbohydrates thatyou will need to eat at a meal or snack.A dietitian can help you decide the amountof carbohydrates that may be right for you. Ageneral rule is that active women need about45 grams of carbohydrates at each meal andactive men need 60 grams at each meal.44
The food label can provide you with theinformation you need for meal planning. Lookat the grams of total carbohydraterather than the grams of sugar. “Totalcarbohydrate” on the label includes sugar,complex carbohydrate, and fiber. If you lookonly at the sugar number, you may end upexcluding healthy foods such as fruits andmilks thinking they are too high in sugar. Youmight also eat too many foods such as cerealsand grains that have no natural or addedsugar, but do contain a lot of carbohydrate.Fiber can help control blood sugar becauseit slows digestion of food. After eating highfiber carbohydrates, there is a gradual increasein blood sugar. A lower fiber carbohydratechoice will cause blood sugar to increase more45
quickly. If a food has 5 grams or more fiber ina serving, subtract half the fiber grams fromthe total grams of carbohydrate for a moreaccurate estimate of the carbohydrate content.Protein is also very important in your diet.Protein takes longer to digest and will preventblood sugars from “spiking” then dropping tooquickly. Some examples of protein are beef,pork, fish, poultry, seafood, eggs, milk,cheese, and peanut butter. It’s best to chooselean and low fat protein foods in order to limitharmful saturated fat and unnecessarycalories.46
Many foods claim to be “sugar free” or“diabetic foods”. Just because foods have theselabels does not mean they don’t containcarbohydrates.Read the food label noting the serving sizeand total carbohydrates for that serving size.People with diabetes were once taught to lookfor the “sugar content” on the label, this isunnecessary because the sugar content isincluded with total carbohydrates.As a guide, use the plate model to makemeals:at least ¾ of the plate with wholegrains, vegetables, and fruit;no more than ¼ of the plate withmeat, poultry, fish, or other sources ofprotein.47
If you notice that a food consistentlycauses a high reading, reduce the portion sizeor omit that food item.Some important tips to remember:Eat 3 meals a dayDo not skip mealsEat at the same time each dayWatch portion sizesLimit high sugar foods and drinksEat meals 4-5 hours apartCheck your blood sugar 2 hoursafter meals48
8. Why do you need to exercise if youhave diabetes?Exercise is important for overall health butfor people with diabetes it can be especiallyhelpful. Usually diabetics have a host of otherproblems along with their high blood glucoseincluding high blood pressure, high cholesterol,obesity, stress, depression, and often timescardiac diseases.Exercise can:Lower and help control blood sugarLower blood pressureHelp to lower LDL cholesterol levelsKeep heart and blood vessels healthyPossibly reduce medicationsHelp with weight lossReduce stress49
Some general suggestions:1. Start slowly, even 5-10 minutes a daycan make a difference.2. Pick an enjoyable activity.3. Check blood sugar before and afterexercise.4. Don’t exercise if blood sugar is over240 or below 100.5. Watch for signs of low blood sugar.50
9.Wearing medical ID:Millions of people have medical conditionswhich medical staff needs to be aware of.Medical alert bracelets can alert health careproviders to any obvious causes ofunresponsiveness or a decreased level ofconsciousness. The benefits of having medicalidentification are:Speaks for you if you’re unable tospeak for yourself.Alerts medical professionals about yourmedical history, helping to speedproper treatment.Can provide notice to your family in anemergency.Provides you and your family peace ofmind.Can save your life!51
52
For the free necklace, fill out this couponRemember to provide a self-addressed stamped envelopeSend to:Free Diabetes NecklaceDiabetes Research and Wellness FoundationP O Box 96046Washington, DC 20090-6046Or you can order online p?cat 10Online orders are charged 2.95 shipping and handling fees to bepaid at time order is placedPlease allow 4-6 weeks for delivery53
54
10. Sick day rule:During illness, diabetes is harder tocontrol. Even a cold can cause blood sugar toget out of control.Some key points to remember are to callthe doctor if you:1. have diarrhea or vomiting that last6 hours or longer;2. have blood sugars greater than 240for 24 hours;3. have fever greater than 100 degrees Ffor 48 hours;4. just aren’t sure about what to do totake care of yourself.55
High blood sugar along with sweating,vomiting, or diarrhea can lead to dehydration.Remember:1.Diabetes medicines are used to lower bloodsugar and are usually given with meals,however if you’re sick, having high bloodsugar, and not eating, call your physicianbefore discontinuing use of these medicines.2.Test your blood sugar more often, perhapsevery 2-4 hours.3.Try to eat the same amount ofcarbohydrates in your meal plan. If vomitingor nauseated, try to drink regular—not diet—sodas, ginger ale, Gatorade, Kool-Aid, orjuices. Even though blood sugars will behigh, you need to continue to take in thesame amount of carbohydrates to mend andkeep up your body.4.Drink plenty of water or non-caffeinatedbeverages to prevent dehydration.56
Family Risk AssessmentCould you have diabetes and not know it?There are almost 26 million Americans withdiabetes—nearly 7 million people havediabetes and don’t know it! Take this test tosee if you are at risk for having diabetes.Diabetes is more common in AfricanAmericans, Latinos, Native Americans, AsianAmericans, and Pacific Islanders. If you are amember of one
blood, the higher the hemoglobin A1c test result will be. Checking your blood glucose at home with a meter tells you what your blood sugar levels is at any one time, but suppose you want to know how you're doing overall. The A1c test gives you a picture of your average blood