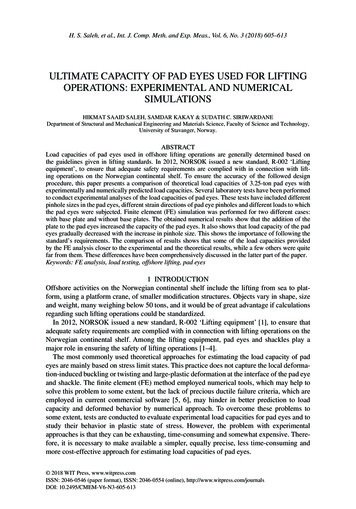
Transcription
THE HEALTH CLUSTERCAPACITYDEVELOPMENT STRATEGY2016 – 2019Photo credit: WHO
TABLE OF CONTENTSForew ord.3Acknow ledgements .4Executiv e Summary .42. The Vision - What w ill w e have achieved four years from now ?.63. The Aim .64. The Scope .75. The Strategic Objectiv es .76. Learning Needs, Gaps and Priorities .97. Capacity Development Activ ities .118. I mplementing the Strategy .139. The risks and assumptions and how they w ill be identified,addressed and mitigated .1310. Funding and Resourcing the Strategy .1511. Monitoring and Ev aluating the I mpact of the Strategy .15Annex 1: Health Cluster Professional Dev elopment I nitial Findingsand Recommendations 2014 (DRAFT) - By Perry Seymour andSandro Colombo .17Annex 2: Learning Needs Analysis (LNA) Report 16 November 2015 . 39Annex 3: Health Cluster Competency Framew ork .48Annex 4: The Log Frame .572
FOREWORDThe number, scale and severity of protracted humanitarian crisisshows an increasing trend in recent years while the humanitariansystem has never been so challenged as of now. Effective leadershipand good coordination in health plays a vital role in addressing thesechallenges. The Global Health Cluster has identified a number ofcrucial functions such as in coordination and health informationmanagement, which needs to be strengthened and furtherdeveloped and will be part of the current W HO reform process underits ‘one single program approach’.The overall aim of the Health Cluster Capacity Development strategyis to reduce death and vulnerability by building effective leadershipand coordination mechanisms to address future epidemics of largescale and continue to address chronic and protracted crisis andstrengthen health systems in fragile and vulnerable countries,effectively and in a cost-efficient manner. This will be achieved bydeveloping a cadre of high performing personnel to effectively leadand coordinate the cluster to deliver an effective response to achievebetter health outcomes. Synergies will be built with other roles underthe Global Health Emergency W orkforce such as the StandbyPartners, the Emergency Medical Teams and GOARN.This requires financial commitment and support, human resources andtechnical expertise with a profound set up and structure. In order toaddress those, the Health Cluster Capacity Development Strategy2016-2019 was developed to provide a clear framework andguidance.The strategy and framework sums up the ideas and views which havebeen studied during the training needs analysis and the last trainingcourse and experiences by people in the field but it also provides theagenda for future work. There is still much to do. The strategy and therelated competency framework will enable us to improve the healthcare for affected populations by identifying the right personnel andbuild up high level performers for the health clusters globally.The Global Health Cluster Strategic Advisory Group are delighted thatthe W HO and its partners, under the Global Health Cluster hasproduced this collaborative work, and we look forward to followingthe impact of this strategy.3
ACKNOWLEDGEMENTSThe Global Health Cluster would like to thank the members of theGlobal Health Cluster Capacity Development Task Team and PeerReviewers who have contributed, by means of their feedback,reflections, ideas and conversations, to the thinking behind thedevelopment and writing of this StrategyBetween 2008 and 2015 nine Health Cluster Coordinator Trainings andthree Tri Cluster Coordinator Trainings (Health, Nutrition and W ASH)took place in: Tunisia, Tanzania, Ecuador, Egypt, Indonesia,Switzerland, El Salvador and France. The Global Health Cluster wouldalso like to thank the Participants, Trainers, Facilitators and Donors whotook part or supported these trainings; this Strategy is based on thelearning and experience which came from all of these events.4
EXECUTIVE SUMMARYThe Health Cluster Capacity Development Strategy 2016 – 2019 hasbeen developed in order to ensure high quality and effectiveleadership and coordination in all heath responses to acute andprotracted humanitarian crisis. The strategy provides the basis forstrengthening the recruitment, learning and performance of currentand potential health cluster personnel and for providing them withopportunities for continuous professional development.The Strategy was developed by the Global Health Cluster CapacityDevelopment Task Team with further input and feedback from PeerReviewers drawn from Global Health Cluster partners.The Learning Needs and GAPs which are addressed by the strategywere identified by means of two Learning Needs Analysis, which wereconducted in 2014 and 2015 respectively. But needs change overtime, so the strategy will ensure that these needs are refreshed andreprioritised at least once during the life of the strategy.The Strategy will ensure that there is a blended and competencybased approach to learning and development, in which a variety oflearning and training activities and access to high quality learningresources will be provided, and it also recognises and supports thecritical role played by Line Managers in ensuring that learning takesplace in a timely manner, is acted upon and is part of a Health ClusterProfessional Development Plan.The strategy proposes nine strategic objectives and it will beimplemented by means of the Log frame in Annex 4 which will beunderpinned by an Annual Plan and budget for each year of thestrategy.5
1. The Vision - What will we have achieved four yearsfrom now?A cadre of high performing health cluster coordination personnel willhave been established in order to ensure that the leadership andcoordination of all health responses to an acute or protractedhumanitarian crisis is responsive, accountable, consistent, predictable,and efficient and provides Value for Money 1. The coordination of theresponse will build national capacity, resilience and preparednessand be delivered in support of the response efforts of nationalauthorities, and in collaboration with other partners and clusters, inorder to meet the needs and the rights of the affected populationand lay the foundations for recovery.2. The AimTo establish a systematic and structured approach to high quality,blended and impactful capacity development that responds to theincreased need and expectation for health clusters to demonstrateeffective health response leadership and coordination in all types ofemergencies.The Strategy addresses the need to identify and develop high performing, dynamic and adaptable health cluster coordinationpersonnel and teams that:1. Have the required combination of skills, knowledge and attitudesneeded to lead and coordinate an effective health response thatmeets the needs of the affected population.2. Are ready to be deployed to crisis-affected countries3. Are able to stay in their role for the time required4. Are continuously supported at all levels (by the Global Health ClusterUnit, W HO HQ, ROs, W COs, cluster partners and other stakeholders)5. Are able to transfer knowledge and build the capacity of localcounterparts6. Have professional development incentives, career paths and jobstability.Value for M oney (VFM) is defined as ensuring that an input is provided at the right time, to the required qualitystandard and at the right cost.16
3. The ScopeThe specific target audience for this Capacity Development Strategyis all health cluster coordination personnel at both national and subnational levels who have identified capacity gaps. This includes, but isnot exclusive to, the roles of Health Cluster Coordinators, InformationManagement Officers, Public Health Officers and any other identifiedpersonnel.Since personnel come to the health cluster through a variety ofrecruitment and management mechanisms, the strategy is notspecific to any agency. Rather, it includes all health cluster personnelwho come to their roles through the W HO’s Division of HumanResources, surge mechanisms, partner organisations, globallymanaged stand-by partner rosters or recruitment at country level. Atpresent, this includes an estimated national level 24 Health ClusterCoordinators, 12 public health information officers, as well as co-leads,surge support and other public health officers working across the 71sub-national hubs.4. The Strategic ObjectivesOver the four years of the Strategy the following Strategic Objectiveswill be achieved:YEAR 1 - 20164.1. A modular and competency based blended learningprogramme2, using a variety of knowledge and skills based learningand training activities for Health Cluster Coordination and HealthCluster Teams is developed and implementation commences, and issupported by the Health Cluster at global, regional and nationallevels.The 2014/15 Learning Needs Analyses strongly suggests the followingtraining programmes: Health Cluster Coordination Training: aimed at Health Cluster Teamsand emphasising the strategic, coordination and informationrequirements of a health response, the core skills (such as leadership,communications, advocacy and partnership building) and thecollective deliverables of the Humanitarian Programme Cycle.When fully developed the blended learning programme w ill consist of induction, direct training, on linelearning, mentoring, coaching and a Community of Practice27
Public Health Information System Training, specifically emphasisingthe information requirements of a health response and the tools thatsupport them.Existing and future relevant training courses and programmes will alsobe mapped out and personal placed on them if appropriate.4.2. The Health Cluster Capacity Development Task Team is fullyoperational and its’ outputs are fully harmonised with other GHC TaskTeams, and informed by the capacity development activities of otherclusters.4.3. Access to high quality blended learning materials and the use ofconsistent and effective learning approaches/methodologies isestablished, by means of: An online learning resource bank containing contextualised learningresources and training materials, case studies, examples of bestpractice, work based assignments, detailed sessions plans andevaluation tools, feedback and impact assessment tools. A pool of high quality facilitators /trainers and resource people whomeet the criteria established by the GHC Capacity Development TaskTeam identified from GHC Partners, appropriate regional and nationalagencies and authorities and other appropriate stakeholders. Ensuring that all learning and training events and activities areinformed by best practice from other clusters, consortiums andpartners4.4. The critical role of partner agencies and Line Managers inidentifying and supporting individual learning and team performanceis strengthened and supported, and all Health Cluster personnelregularly participate in performance management reviews that arealigned with the Health Cluster Capacity Development Strategy andCompetency Framework and form part of a Health ClusterProfessional Development Plan.4.5. All Health Cluster partner agencies have the policies andprocesses in place in order to be able to induct and train personnelon how they can actively contribute to Health Cluster activities duringhealth emergencies.YEAR 2 - 20174.6. Effective mechanisms are in place to facilitate the integration offeedback from Health Cluster and inter-Cluster lessons learned,8
debriefs of personnel and end of mission reports into Health Clustercapacity development activities and the production anddissemination of follow up reports,.4.7. A learning culture is firmly established throughout the HealthCluster in which all personnel, and their Line Managers, are jointlyresponsible and accountable for ensuring that they have the requisitecompetencies for their role in a response, and in which thosepersonnel who have the potential for professional development inHealth Cluster roles are identified, supported, mentored, coachedand developed in preparation for taking up these roles.YEAR 3 - 20184.8. A modular Health Cluster coordination programme provides acareer pathway to a professional award through accreditation by aninternationally recognised academic institution. This will include theaccreditation of “on the job” and prior learning. 3YEAR 4 - 20194.9. Effective capacity development forums, protocols andmechanisms for engaging with and working with national and sub national health authorities and regional and national institutions arefully established and operational in order to ensure effective exitstrategies and to build national response coordination capacity andcommunity engagement.5. Learning Needs, Gaps and PrioritiesThe learning needs which will be addressed by this strategy wereidentified by means of two learning needs analyses (LNA). The first LNAwas completed in November 2014, and reported in the Health ClusterProfessional Development Initial Findings and Recommendations(Annex 1).A second LNA was conducted by the Capacity Development TaskTeam in November 2015. The findings of the combined LNAs areshown in Table 1:3The institution will need to be scoped out9
The combined LNAs showed that the following learning needs/gapsare a high and urgent priority and will be the focus of activities in 2016and beyond. The learning needs/gaps are in priority order:PRIORITY ORDERLEARNING NEEDS/GAPS1Information Management2Leadership3Communication3Strategy Formulation and Planning5Inter Cluster Needs Assessment6Advocacy6Role of Coordination and its Core FunctionsThe following learning needs/gaps were also identified as priorities butare less urgent: Diplomacy Knowledge of the contextThe LNA conducted in 2015 also identified role-specific learningneeds/gaps which will be taken into account in the design anddevelopment of appropriate training and learning materials.For a copy of the full Learning Needs Analysis (LNA) Report November2015 see Annex 2.10
At the Global Health Cluster Meeting in December 2015 the followingneeds were also identified as priorities by partners and participants: W orking remotely in hard to reach and insecure contextsPrioritisationNegotiationThe learning needs and gaps on which this Strategy is based will bereviewed annually by the Health Cluster Capacity Development TaskTeam and incorporated into Annual Plans.6. Capacity Development ActivitiesThe learning activities which will be provided under the auspices ofthe Health Cluster Capacity Development Strategy will follow the 7020-10 rule which is the foundation for blended learning. This rulesuggests that successful capacity development takes place withinthree clusters of learning experience: challenging “on the job ”assignments (70%), developmental relationships such as coaching,mentoring and peer exchange (20%), and direct/formal training(10%). Most organisations now acknowledge that reliance on formaltraining alone restricts the impact of learning on performance.The approach to capacity development will also be innovative,based on best practice in the humanitarian sector and makeeffective use of current and future technology.The Health Cluster Capacity Development Task Teamwill provide the guidance and stewardship needed to:6.1. Ensure the effective implementation of the Strategic Objectives6.2. Develop and implement a Health Cluster CoordinationCompetency Framework for Health Cluster Personnel. (See Annex 3 forthe Final Draft).6.3. Produce an annual W ork Plan and budget with costed activities6.4. Provide detailed guidance to individuals and their Line Managerson how to use the Competency framework in order to identifylearning needs and link to agency performance review processes.11
6.5. Develop the tools and guidance needed to incorporate HealthCluster coordination competencies into all Health Cluster partners’selection and recruitment processes6.6. Produce annual training plans, based on the log frame andcontaining the planned programme of all training events, workshopsand learning activities. The plan will also contain the eligibility criteriafor participants and the process for accessing places6.7. Provide the curriculum, training design, methodology andevaluation tools advice and guidelines for all Health Cluster Personneltraining.6.8. Provide an online learning portal with access to high qualitylearning materials and resources, information about planned capacitydevelopment events and links to eLearning, webinars andCommunities of Practice and other online peer exchange platforms.6.9. Identify a pool of high quality trainers and facilitators from HealthCluster partners and other Clusters, and provide them withpedagogical guidance and support.6.10. Strengthen the induction and orientation for all personnel inhealth cluster coordination related roles.6.11. Provide access to structured coaching, mentoring andshadowing based on learning needs which are linked to needs andpriorities6.12. Provide the tools and guidance to develop professionaldevelopment pathways for all personnel in Health Clustercoordination related roles6.13. Provide guidance for the minimum criteria for acceptance ontodeployment rosters and deployment to a response6.14. Identify and establish a link with appropriate academicinstitutions6.15. Refresh and update the Learning Needs Analysis bi-annually12
7. Implementing the StrategyThe implementation of the Strategy will be by means of the Log Framein Annex 4 and Annual Plans and budgets which will be reviewed biannually by the Health Cluster Capacity Development Task Team.The strategy identifies in broad terms when the strategic objectives willbe achieved. The Log Frame in Annex 4 specifies further in whichquarters certain activities should take place. These broad outlinesserve as a framework to develop detailed annual plans, includingassociated detailed budget plans.Milestones have been incorporated in the log frame so that progresstowards strategic objectives can be measured. Progress reports will bepresented during GHC partner meetings in which the partners canprovide feedback and suggestions, where the strategy has to beadjusted on taking the strategy forward.8. The Risks and Assumptions and How They Will BeIdentified, Addressed and Mitigated8.1. GHC members agree on the competency framework.The competency framework will be shared with the partners forconsultation, so they can provide input and get a sense of ownershipof the framework.8.2. Partners can be found to engage with the trainingPartners with a comparative advantage will be approached with aconcrete ask to provide support. For example, some organisationsand institutions are specialised in information handling and could beapproached to cover these specific sessions. The partner capacitysurvey mapping implemented in 2015 will also be used for this.8.3. HC personnel can access learning materials in field locationsW hile the internet is generally improving, the platform through whiche-learning material is being made available should be designed insuch a way that small bandwidth can still be accessed.8.4. The GHC is able to influence the performance review of WHO staffThe GHC should advocate with W HO HR, which manages thecontracts of HC staff, for cluster coordination specific essentials to beincluded in the performance review formats, clearly stating the needfor this.13
8.5. All Line Managers conduct performance reviews periodicallywhich are aligned to the Health Cluster Competency Framework andthey accurately identify and capture Health Cluster learning needs.All Line Managers will receive a copy of the Competency Framework,and written guidelines will be provided on how to incorporate these inthe performance reviews. Partner organisations who second/surgestaff to the Health Cluster will also could receive a copy of thesedocuments. .8.6. All Line managers are willing to engage with learning needsResults from Learning Needs Assessments and training reports of theHCC training and other learning activities will be widely distributed torelevant ROs, W COs and all Health Cluster partners to provideinformation to Line Managers on the advantages of investing in HealthCluster staff development. .8.7. Priority is not given to ensuring that the requisite legal frameworksthat enable rapid deployment of partner staff are in placeThe W HO and GHC partners must find appropriate legal solutions fordeploying staff through partnership arrangements.8.8. Partners are willing to make staff available for deploymentResults from pilot projects and various cluster research reports highlightthe advantages of agencies making staff available to fill HealthCluster positions in acute and protracted humanitarian crises. Thesereports also provide guidance on good practice and policiesdeveloped within partners to address and resolve this challenge.8.9. National health authorities are able to express concrete capacitybuilding needsStandardised tools and approaches for capacity needs identificationwill be developed and disseminated to enable national healthauthorities to identify concrete needs and gaps14
9.Funding and Resourcing the Strategy9.1. Donors will be approached to fund specific elements of thestrategy, such as covering the costs of trainings, setting up andmaintaining databases and underwriting posts9.2. Partners will be expected to mainstream and embed HealthCluster activities and to contribute to the implementation of thisstrategy by supporting those parts of the strategy where they have acomparative advantage in a certain area, e.g. delivering tra ining.9.3. It is also expected that Health Cluster strategic partners willcommit their own agencies funds to making personnel/humanresources available to the cluster for a health response.9.4. The W HO (as cluster lead agency) and cluster partners will ensurethat appropriate learning and development expertise is available tosupport quality implementation of this strategy.9.5. As the development of this strategy is taken forward andadjustments are made to the strategy based on the findings ofmonitoring and evaluation reports yearly budgets will be made tospecify the associated costs.10. Monitoring and Evaluating the Impact of the Strategy10.1. The implementation of the strategy will be monitored byreporting on the milestones set in the log frame. Regular progress willbe monitored through quarterly reports by the Capacity DevelopmentTask Team to the Global Health Cluster Coordinator, reporting onachievements made towards milestones and identifying lessons totake forward and make adjustments to the strategy where necessary.10.2. After year two (2017) and year four (2019), external mid-term andfinal evaluations4 respectively will establish the extent to which thegoals and targets have been achieved. The findings from monitoringreports and evaluations will be shared with the CapacityDevelopment Task Team and the SAG. At the end of eachdeployment, Health Cluster staff will be debriefed, and their collectivefeedback may be used to adapt the strategy.4Funding w ill need to be identified for these evaluations15
10.3. The ultimate goal of the strategy is to significantly improve thequality of health cluster coordination when responding to an acute orprotracted humanitarian crisis.The performance of the Health Cluster response will be monitored bymeans of: Health Cluster Progress Reports based on the HRP and KPIsand other specific standard deliverables Country Cluster Performance Monitoring Joint Health Sector Reviews Health Sector EvaluationsThe lessons learned from these reviews will be evaluated by the HealthCluster Capacity Development Task Team and addressed in HealthCluster capacity development activities.16
ANNEX 1:Health Cluster Professional Development Initial Findings andRecommendations 2014 - By Perry Seymour and SandroColomboTABLE OF CONTENTS:1. Introduction .182. Objectives and scope of the report.193. Methodology and Findings.213. Health Cluster Professional Development Recommendations.23A. Selecting Candidates .241. Health Cluster Coordination Team composition, Job Profiles and PersonSpecifications.242. Health Cluster Competency Framework .243. Health Cluster team candidate identification process, particularly forHCCs.28B. Supporting Health Cluster teams.311. Revision of the Global Health Cluster Guide .312. An Online Global Health Cluster Portal .313. Staff Capacity Building.32C. Ongoing Assessment Of Staff L&D Needs .36D. Performance assessment.36E. Retention and Career Development.371. Job Security .372. Support and Development .383. Career Development Opportunities.38Annex A: Learning Needs Assessment and Consultation Interview Findings.40Annex B. Proposed workplan .45References .3817
1. INTRODUCTIONSince its establishment in 2005, the Global Health Cluster (GHC)partnership has had a solid history in humanitarian action. Memberorganisations and partners have collaborated in a manyemergencies, striving together globally and at the country level tobring about more effective, efficient and predictable healthinterventions in emergencies.Moreover, the W HO, as the Cluster Lead Agency, has instituted anumber of recent measures that have moved the work of the GHCforward, including the adoption of the W orld Health Assemblyresolution on humanitarian health (resolution 65.20 of May 2012) andthe introduction of the Emergency Response Framework (ERF). Thesechanges have come into place at the same time as other significantchanges in the humanitarian system, particularly the reforms of theInter-Agency Standing Committee and the Transformative Agenda(TA).At the same time, the number, scale, and severity of humanitariancrises shows an increasing trend, due to a combination of factors. Thehumanitarian system has never been so challenged as now, with fourL3 crises, the Ebola epidemic and several protracted emergencieswith no end on sight. Moreover, the changing nature of humanitariancrises (such as overlapping of natural disasters and complexemergencies, trans-border crises like in the DRC/CAR region orcurrently in the Ebola crisis) and the shrinking humanitarian space(such as in Syria and Iraq) pose new challenges to health workers.As the number and complexity of such emergencies has grown, thehuman and technical capacity to effectively coordinate the healthresponse of diverse actors has not evolved proportionally: there is anoverall shortage of skilled Health Cluster Coordinators (HCCs) withbroad public health competence and the right mix of leadership andcommunication skills, supported by a competent coordination teams,able to mobilise additional technical expertise and financialresources, available to be deployed at short notice and to remain inposition for extended periods. The Health Cluster CoordinationPerformance 2013 report highlighted the fact that staffing of HealthCluster teams was sub-optimal in many countries.18
There are currently around 24 countries with active clusters, some withsub-national hubs. Considering the staffing needs for coordinationteams working in large-scale crises, the need for replacing HealthCluster staff on leave or R&R, natural attrition, etc. the number of staffrequired for health coordination ranges conservatively between 50-70professionals. At the estimated cost of 10-15M USD5 per year, whichrepresents a very small share of total humanitarian funding for h
Annex 1: Health Cluster Professional Development Initial Findings and Recommendations 2014 (DRAFT) - By Perry Seymour and . learning and experience which came from all of these events. 5 EXECUTIVE SUMMAR