Transcription
PBM Toolkit
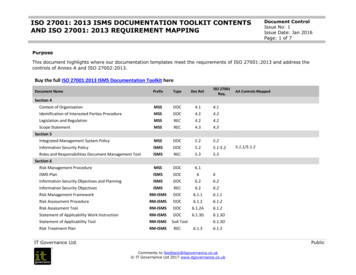
Table Of ContentsWhat is a PBM?Overview: PBM and IBMs. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1Webinar: Insurance and PBM Utilization. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4Overview: ADAPs Contracts with PBM. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10Selection and Implementation of a PBMWebinar: PBM: From RFP to Implementation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15PBM Proposal Template . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20PBM Contact List. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24PBM Contract Language Bank and Things to Consider. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27PBM Request for Proposal Example. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 51All resources and materials in this toolkit have been developed between January 2013 and March 2014. Production of thesematerials and the following cumulative electronic toolkit was funded under a cooperative agreement with Human Resources andServices Administration (HRSA).
What is a PBM?
OVERVIEWPharmacy Benefits Managers (PBMs)and Insurance Benefits Managers (IBMs)1
OVERVIEW: Pharmacy Benefits Managersand Insurance Benefits ManagersPHARMACY BENEFITS MANAGER(PBM) entrally process claims in real time, claimCadjudication, record keeping and reportsto clients, payment to providers and fiscalintermediaries (e.g., processing of co-payments,deductibles for medications; track data requiredto receive rebates; performing electronic splitbilling at pharmacy point of service, paypharmacy invoices, and bill ADAP; handlerebates and discounts with pharmaceuticalcompanies; serve as electronic data transferagent to meet all requirements related toMedicare TrOOP payments [serve as TrOOPcoordinator and prepare reports]; paying HICco-payments and deductibles) ssist with benefit design and business rulesA(covered drugs, exclusions, limits cost-sharingprovisions [differential co-payments for genericor preferred drugs], mail-order dispensing) I nformation management (risk assessment,profiling)The following information is an excerpt from theHRSA/HAB Division of State HIV/AIDS ProgramsAIDS Drug Assistance Program (ADAP) Manual(2012). The Manual can be accessed onlineat: .What is a PBM?A pharmacy benefits manager is an organization orsystem that provides administrative and pharmacyclaim adjudication services, and pharmacy benefitcoverage programs. PBM services can include: Contracting with a network of pharmacies stablishing payment levels for providerEpharmacies Negotiating rebate arrangements eveloping and managing formularies, preferredDdrug lists, and prior authorization programs ontinuous electronic insurance eligibilityCchecking Maintaining patient compliance programs Pharmacoeconomic studies Performing drug utilization review Operating disease management programsAdministrative functions typically include:In addition, PBMs perform a variety of drugutilization functions. These services generallyinvolve “managing” drug utilization to reduce costsand maintain or improve quality. These functionsinclude policies and programs to affect prescribingand dispensing patterns and are targeted towardspharmacists, patients, and prescribers. The rangeof drug utilization functions that a PBM can offerinclude: Many PBMs also operate mail order pharmaciesor have arrangements to include prescriptionavailability through mail order pharmacies. stablishing and maintaining a network ofEproviders (recruit and manage a network ofpharmacies that fill prescriptions for RyanWhite ADAP clients; negotiate prices andpayment terms and contract with pharmacies,monitor/audit performance)2 ormulary and formulary related activitiesF(provider incentives, patient incentives, rebatemanagement, prior authorization therapeuticinterchange)
rug use review (retrospective-drug utilizationDreview (DUR), prospective-DUR [some PBMsuse the term “concurrent-DUR”], DURinterventions, “academic detailing,” providereducation) isease management (therapeutic outcomesDmanagement) atient compliance (patient education, e.g.,Pnewsletters; phone reminders) Negotiation of claims Record keeping Access to provider networks Utilization review Other administrative activitiesAs of January 2013, more than 30 states wereusing a PBM to provide administrative andpharmaceutical claims adjudication services forat least a portion of their traditional ADAP (fullpayment of medications). Of these states, manywere also currently using or exploring the use of anPBM/IBM/TPA to assist in the claims adjudicationprocess for the insurance component of theirprogram, including eligibility screening, enrollment,and payments. ADAPs cite many reasons why theyhave contracted with a PBM and/or IBM/TPA,including:What is an IBM?An insurance benefits manager or third-partyadministrator is an organization or system thatprovides administrative and insurance claimadjudication services. An IBM/TPA is neitherthe insurer nor the insured; it simply handles theadministration of the plan. IBM/TPA functions caninclude:Claims adjudicationEnrollment activitiesADAPS AND PBMS/IBMSINSURANCE BENEFITS MANAGER(IBM) OR THIRD-PARTYADMINISTRATOR (TPA) Examples of IBMsThe following directory can be a useful resource foridentifying IBMs/TPAs that operate within h/CompanySearch.aspx?nid 71Examples of PBMsThe following directory can be a useful resource foridentifying PBMs that operate within your state:http://www.pbmi.com/pbmdir.aspClaims processing/administrationPremium collection/paymentIBMs/TPAs are prominent players in the managedcare industry and have the expertise and capabilityto administer all or a portion of the claims process.PBMs may charge a per transaction administrativefee, depending on the number and extent ofservices that they are contracted to perform. Thefees charged, if any, are dependent on the contractterms negotiated between the ADAP and PBM.ADAPs that contract with a PBM pay for the costof the drug, the pharmacy dispensing fee, and anadditional per claim administrative fee. In somecases, the administrative fee is rolled into thedispensing fee charged per prescription. 3 Reduction in administrative costs I mprovement in the efficiency of servicesprovided to clients ssistance in eligibility screening to ensure payerAof last resort S treamlining of the ADAP prescription andpayment delivery system, including inventorycontrol Management of rebate processing
WEBINARInsurance and PBM UtilizationADAP AND INSURANCE: PURCHASINGCONTINUING INSURANCE ANDUTILIZING PHARMACY BENEFITS MANAGERSINSURANCE BENEFITS MANAGERS4
Insurance and PBM Utilization:Purchasing / Continuing Insurance andUtilizing Pharmacy Benefits Managers /Insurance Benefits Managers2. A DAP programs must be able to accountfor and report on funds used to purchaseand maintain insurance policies for eligibleclients including covering any costsassociated with these policies.The following is the original webinar text. Anonline recording of this webinar is available auncher false&fcsContent true&pbMode normal.3. F unds may only be used to purchasepremiums from health insurance plans thatat a minimum provide prescription coverageequivalent to the Ryan White HIV/AIDSProgram Part B formulary.ADAPS AND INSURANCE e Ryan White Program allows states to useThADAP dollars to purchase health insuranceand pay insurance premiums, co-paymentsand/or deductibles for individuals eligible forADAP, provided the insurance has comparableformulary benefits to that of the ADAP. er HRSA policy notice 07-05, ADAPs arePpermitted to purchase or continue an insurancepolicy for clients. This policy notice serves as anupdate to the previously issued HRSA policynotice 99-01. rior to the use of ADAP funds for the purchasePof health insurance, states must provideHRSA/HAB with notification of intent withthe aforementioned assurances to the GrantsManagement Specialist.4. The total annual amount spent on insurancepremiums cannot be greater than the annualcost of maintaining that same population onthe existing ADAP program.5. F unds may be used to cover any costsassociated with the health insurance policy,including co-payments, deductibles, orpremiums to purchase or maintain insurancepolicies.6. C urrent client eligibility guidelines, setunder Section 2616(b) of the Public HealthService Act, must be followed. The Statesmust maintain their contributions to theirHIV/AIDS care programs as required underSection 2617(b)(7)(E).Funds designated to carry out the provisions ofSection 2616 of the Public Health Service Act maybe used to purchase health insurance whose coverageincludes the full range of HIV treatments and accessto comprehensive primary care services, subject tothe conditions below:7. R yan White HIV/AIDS Program fundsmust be the payers of last resort forpharmaceuticals.8. Th e State must assure that ADAP funds willnot be used to purchase health insurancedeemed inadequate by the State in itsprovision of comprehensive primary careservices.1. F unds must continue to be managed as partof the established ADAP Program.5
S tates are increasingly using ADAP funds forthis purpose.INSURANCE PURCHASING ANDHEALTH REFORM- orty ADAPs reported using funds forFinsurance purchasing/continuation in 2012representing 227 million in estimatedexpenditures in FY2012.- DAPs reported spending over 20.3Amillion on insurance purchasing/continuation in June 2012.-I n June 2012, 46,653 ADAP clients werecovered by such arrangements.- Spending on insurance purchasing/continuation represented an estimated 434 per capita in June 2012, about 59%of the average monthly cost per client formedications purchased by ADAPs, basedon overall drug expenditures, in that month( 1,054).S tates are preparing insurance purchasingprograms for ACA coverage by:- oordinating ADAP eligibility andCapplication processes with the Marketplace,including aligning ADAP income criteriawith Modified Adjusted Gross Income(MAGI).- ssessing ADAP capacity to help clientsAafford Marketplace coverage (for clientsreceiving subsidies as well as those ineligiblefor federal subsidies).- eveloping relationships with MarketplaceDplans and pharmacies.- Assessing scope of coverage and cost ofMarketplace plans.- amping up ADAP benefits counselingRactivities and staff.INSURANCE PURCHASING ANDCONTINUATION CHECKLIST hen considering making any changes,Wdetermine if they are economically feasible andadministratively manageable for the ADAPin light of current staff capacity and internaladministrative processes.NASTAD ADAP Monitoring Project Annual Report, January 20132014 ACA Coverage OptionIncome Eligibility ThresholdMedicaid ExpansionIncome up to 138% FPLAdvance Premium Tax Credit for purchase of privateinsurance through exchanges/marketplacesIncome between 100 and 400% FPL (ineligible forMedicaid or affordable employer-based coverage)Cost-sharing subsidies to offset out-of-pocketcosts of private insurance through exchanges/marketplacesIncome between 100 and 250% FPL(ineligible for Medicaid or affordable employerbased coverage)Unsubsidized private insurance coverage throughexchanges/marketplacesIncome below 100% FPL (ineligible for Medicaid)6
rain case managers on how to enroll clients inTthe insurance program. ducate clients and case managers aboutEthe insurance purchasing and continuationprogram. erify that ADAP pharmacy network or directVpurchase administration can work with thehealth insurance payers. Develop plan assessment tools and procedures. nticipate problems with client participationAin the insurance program that may occurwith implementation and develop proceduresto respond rapidly to address unintendedconsequences – including waivers. ommunicate with your HRSA Project OfficerCand NASTAD when the state is consideringimplementing an insurance program, when andif significant challenges arise, and when anychanges are actually implemented.ADAPS AND PBMS/IBMS onsider the feasibility of electronic applicationCsystems. DAPs cite many reasons why they haveAcontracted with a PBM and/or IBM/TPA,including:-Reduction in administrative costs-I mprovement in the efficiency of servicesprovided to clients- Assistance in eligibility screening to ensurepayer of last resort e familiar with state legislation andBadministrative regulations that may impact yourability to make changes in ADAP.-S treamlining of the ADAP prescriptionand payment delivery system, includinginventory control-Management of rebate processing ollow the internal state agency process forFreview and approval of changes to the ADAP. ommunicate to the community aboutCwhy and when the ADAP will introduce aninsurance purchasing and/or continuationprogram. pharmacy benefits manager is an organizationAor system that provides administrative andpharmacy claim adjudication services, andpharmacy benefit coverage programs. I f Ryan White Part B programs decide to useADAP funds to purchase health insurance,they must submit a Notification of Intent toHRSA that addresses: the methodology that willbe used, an assurance that the pharmaceuticalcomponent of the insurance policy includes aformulary equivalent to the ADAP formulary,and assurance that the cost of providingcoverage to clients through the insuranceprogram is cost neutral in the aggregate. (SeeHAB Policy Notice 07-05.) any PBMs also operate mail order pharmaciesMor have arrangements to include prescriptionavailability through mail order pharmacies. Administrative functions typically include: WHAT IS A PBM?- stablishing and maintaining a network ofEproviders Centrally process claims in real- Assist with benefit design and business rules onsult other ADAPs that have investigatedCand/or adopted an insurance program to findout how they approached it, the results andlessons learned.- Information management- ontinuous electronic insurance eligibilityCchecking- Pharmacoeconomic studies7
I n addition, PBMs perform a variety of drugutilization functions. The range of drugutilization functions that a PBM can offerinclude:the insurer nor the insured; it simply handlesthe administration of the plan. -Formulary and formulary related activities-Drug use review-Disease managementADAPS AND REBATES-Patient complianceREBATES ON DEDUCTIBLES ANDCO-PAYMENTS BMs may charge a per transactionPadministrative fee, depending on the numberand extent of services that they are contracted toperform.- The fees charged, if any, are dependent onthe contract terms negotiated between theADAP and PBM.-- er HRSA program letter dated April 29, 2005,PADAPs are permitted to file for full rebates onpartial payments of health insurance policies. DAP grantees that participate in the 340BAdrug pricing program can claim full rebates onpartial pay claims under one of the followingcircumstances: DAPs that contract with a PBM payAfor the cost of the drug, the pharmacydispensing fee, and an additional per claimadministrative fee.I n some cases, the administrative fee isrolled into the dispensing fee charged perprescription. n insurance benefits manager or third-partyAadministrator is an organization or system thatprovides administrative and insurance claimadjudication services. An IBM/TPA is neitherthe insurer nor the insured; it simply handlesthe administration of the plan.I BMs/TPAs are prominent players in themanaged care industry and have the expertiseand capability to administer all or a portion ofthe claims process.- e ADAP grantee must pay the deductibleThfor the patient’s medication under theinsurance policy, whether or not theprogram also pays the health insurancepremium; or- e ADAP grantee must pay the co-pay forThthe patient’s medication under the insurancepolicy, whether or not the program also paysthe health insurance premium. I n both of the stated circumstances, there is adirect relationship between the ADAP paymentand the patient’s medication. rugs that are fully reimbursed by insuranceDplans, where only the insurance premiums havebeen funded by ADAPs, are not eligible forrebate.- Therefore, payment of the insurancepremium alone does not entitle an ADAPto claim a rebate under the 340B drugpricing program.WHAT IS AN IBM? I BMs/TPAs are prominent players in themanaged care industry and have the expertiseand capability to administer all or a portion ofthe claims process. n insurance benefits manager or third-partyAadministrator is an organization or system thatprovides administrative and insurance claimadjudication services. An IBM/TPA is neither8
-FILING FOR REBATES DAPs should bill for units dispensed or otherAout-lays for prescription costs. o file for rebates, ADAPs must bill drugTmanufacturers for the 340B and ACTF UnitRebate Amount (URA) for the number of unitsdispensed. NDC Drug name Quantity dispensed Number of prescriptions o do so, ADAPs should submit a cover letterTand claims submission to each pharmaceuticalcompany for which the ADAP is seeking arebate. Amount paid out in claims e cover letter should be sent on ADAP/healthThdepartment letterhead and include the followinginformation:RESOURCES- ate the claims submission is beingDsubmitted- statement that the ADAP participates inAthe 340B drug discount program.- otation about which quarter rebates areNbeing submitted for (i.e, Calendar Year 2013Quarter 1) - Payment remittance information To whom the check should be payable(i.e., Department of Health, ADAP) Federal identification number Contact name Mailing address Table for the claims submission, noting: Phone number in the event of questions The claims submission should include:-Company specific listing- otation about which quarter rebates areNbeing submitted for (i.e, Calendar Year 2013Quarter 1)9 ebates should be submitted within 90 days ofRthe close of a given quarter. ational Alliance of State and Territorial AIDSNDirectors (NASTAD) – www.NASTAD.org HRSA HIV/AIDS Bureau – www.hab.hrsa.gov RSA Target Center – Technical AssistanceHfor the Ryan White Community - http://careacttarget.org/ aiser Family Foundation – http://kff.org/Khivaids/ ublic Law No. 104-191, Health InsurancePPortability and Accountability Act of 1996 ( 2003). Health Insurance Continuity. In RyanWhite Ryan White Program Part B Manual(Chapter 5). Retrieved December 7, 2006 tm#SecVChap5c
OVERVIEWADAPs Contracts WithPharmacy Benefit Managers (PBM),Insurance Benefit Managers (IBM)/Third Party Administrators (TPA), andMedical Benefits Managers (MBM)10
OVERVIEW: ADAPs Contracts With PharmacyBenefit Managers (PBM), Insurance BenefitManagers (IBM)/Third Party Administrators(TPA), and Medical Benefits Managers (MBM)NASTAD recently surveyed ADAPs about their us
Jun 20, 2012 · PBM/IBM/TPA to assist in the claims adjudication process for the insurance component of their program, including eligibility screening, enrollment, and payments. ADAPs cite many reasons why they have contracted with a PBM and/or IBM/TPA, including: Reduction in adminis