Transcription
CLINICAL BRIEFSPhase 3 Clinical Trials SupportSTELARA (ustekinumab)for the Treatment of Moderateto Severe Plaque PsoriasisBy Jack Alan McCain Jr.A review of recently published datawith a commentary for managed care decision makersBy Jeffrey M. Sobell, MDSupplement toCentocor Ortho Biotech Inc. provided funding for thispublication and had editorial control.Volume 19, No. 10Supplement 3October 2010Please see Important Safety Information on pages 8-9 and accompanyingFull Prescribing Information and Medication Guide for STELARA on pages 10-15.
Phase 3 Clinical Trials Support STELARA (ustekinumab) for theTreatment of Moderate to Severe Plaque PsoriasisSTELARA is a subcutaneously administered biologic approved by the US Food and Drug Administration in September 2009 for thetreatment of adult patients (18 years or older) with moderate to severe plaque psoriasis who are candidates for phototherapy orsystemic therapy.1,2 This Clinical Brief summarizes the 2 phase 3 multicenter, randomized, double-blind, placebo-controlled trialsthat demonstrated the efficacy and safety of STELARA .1,3,4PHOENIX 1PHOENIX 1 examined the efficacy and safety ofSTELARA vs placebo over 12 weeks in patients withmoderate to severe plaque psoriasis. To assess the efficacyand safety of long-term usage for up to 76 weeks, arandomized-withdrawal design was used. The primaryendpoint was the proportion of patients who achieved aPsoriasis Area and Severity Index* score (PASI 75) atWeek 12. PASI 75 represents a 75% improvement frombaseline PASI score. Major secondary endpoints includedthe proportion of patients with a Physician’s GlobalAssessment (PGA) score of Cleared or Minimal at Week12, and in the randomized withdrawal phase, time to lossof PASI 75 response in the group receiving maintenancetherapy with STELARA compared with the groupwithdrawn from treatment at Week 40. The eligibilitycriteria for PHOENIX 1 are presented in Table 1.3Study designPHOENIX 1 was divided into 3 phases: (1) a placebocontrolled phase from Weeks 0 to 12, (2) a placebocrossover and active-treatment phase during Weeks 12 to40, and (3) a randomized-withdrawal phase during Weeks40 to 76 (Figure 1). Patients were randomly assigned inequal proportions at baseline to STELARA 45 mg orSTELARA 90 mg at Weeks 0 and 4, and then every 12weeks, or placebo. Patients randomized to receive placeboat Weeks 0 and 4 crossed over to receive STELARA 45 mg or STELARA 90 mg at Weeks 12 and 16.1,3At Week 40, patients initially randomized to receiveSTELARA who achieved long-term response (PASI 75,defined as a 75% improvement from baseline PASI scoreat Weeks 28 and 40) were rerandomized to continuemaintenance treatment with STELARA or placebo. Whenpatients who were withdrawn from treatment at Week 40lost at least 50% of PASI improvement, they wereretreated. Patients not achieving PASI 75 at Week 28 or 40were not rerandomized, and their dosing was discontinuedor modified.3TABLE 1. Eligibility criteria for PHOENIX 1 and PHOENIX 23,4Key inclusion criteriaKey exclusion criteriaMen and women 18 years of ageNonplaque psoriasisDiagnosis of plaque psoriasis for 6 monthsRecent serious systemic or local infectionEligible for phototherapy or systemic therapyMalignancy (excluding treated basal or squamous cell skin cancer 5 years)Plaques covering 10% body surface area (BSA)Previous treatment with agents targeting IL-12 or IL-23PASI score 12Biological or investigational agents within the previous 3 monthsConventional systemic psoriasis therapy or phototherapy within the previous 4 weeksNo history or symptoms of active tuberculosis (TB)†Topical psoriasis treatment within the previous 2 weeks*The PASI divides the body into 4 regions and assesses each separately for redness, thickness, and scaliness on a scale of 0 to 4. Scores range from 0 to 72.Higher scores indicate greater severity of disease. PASI 50 and PASI 75 represent 50% and 75% improvement overall, respectively, in PASI score.5,6†Patients with latent TB (a positive Mantoux tuberculin skin test without radiologic evidence of TB at screening) were allowed to enroll if they beganappropriate therapy for TB according to local country guidelines for immunocompromised patients prior to, or concurrently with, the firstadministration of study agent.3,42Please see Important Safety Information on pages 8-9 and accompanying Full Prescribing Information andMedication Guide for STELARA on pages 10-15.
FIGURE 1. Week 0 through Week 76 study design for PHOENIX 13RANDOMIZATIONRANDOMIZATIONGROUP 1STELARA 45 mg at Weeks 0, 4, then every 12 weeksGROUP 2STELARA 90 mg at Weeks 0, 4, then every 12 weeksSTELARA 45 mg at Weeks 12, 16, then every 12 weeksGROUP 3Placebo-controlled phase045 mg every 12 weeksPlaceboRetreatment90 mg every 12 weeksPlaceboRetreatmentPlaceboRetreatmentGROUP 3bSTELARA 90 mg at Weeks 12, 16, then every 12 weeksWeek -4RetreatmentGROUP 3aPlacebo at Weeks 0GROUPand 4 1ScreenPlaceboRandomizedwithdrawal phasePlacebo-crossover and active-treatment phase1228‡40§76Reprinted from The Lancet, Vol. 371, Leonardi CL, et al; for the PHOENIX 1 study investigators. Efficacy and safety of ustekinumab, a humaninterleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial(PHOENIX 1), pages 1665-1674, 2008, with permission from Elsevier.‡At Week 28, non-responders (PASI 50) in all groups discontinued STELARA , partial responders (PASI 50 to 75) initiated dosing every 8 weeks,and PASI responders (PASI 75) were treated every 12 weeks.3§At Week 40, patients in Group 1 and Group 2 who responded to dosing every 12 weeks were randomized to receive either placebo or continuedtreatment with STELARA every 12 weeks at their original dose. Individuals in Group 3 were treated with placebo. Upon loss of therapeutic effect,patients receiving placebo were retreated at their dosing regimen before withdrawal. Across all groups, non-responders or partial responders wereadjusted to dosing every 8 weeks. Patients already receiving dosing every 8 weeks continued this dosing schedule.3ResultsSignificantly more patients in both the STELARA 45 mgand 90 mg groups achieved the primary endpoint—PASI 75 atWeek 12—than the patients in the placebo group (P 0.0001;Figure 2). Efficacy was achieved rapidly, with significantly higherproportions of patients treated with STELARA achievingPASI 50, or a 50% improvement from baseline PASI score, byWeek 2 and PASI 75 by Week 4. Cleared or Minimal disease asmeasured by the PGA was achieved by significantly morepatients receiving STELARA than by those receiving placeboat Week 12 (P 0.0001; Figure 2). Patients taking STELARA consistently showed greater improvement in their psoriasiscompared with patients taking placebo, as measured byPASI or PGA scores through Week 12. Efficacy continued wellafter the placebo-controlled portion of the study. Patientsrandomized to receive placebo at baseline achieved similarresponse rates after crossover at Week 12.3Maximum efficacy was observed in both STELARA 45 mg and 90 mg groups at Week 24. At Week 28, 90% ofpatients in both groups treated with STELARA achievedPASI 50, 70% achieved PASI 75, and approximately 50%achieved PASI 90 (Figure 2). These response rates weregenerally maintained through Week 40, at which pointlong-term responders underwent randomized withdrawal.3Among patients rerandomized at Week 40, maintenanceof PASI 75 (defined as the time to loss of PASI 75 response)was better in patients receiving maintenance therapy thanin patients withdrawn from therapy through 1 year(P 0.0001). Patients on maintenance therapy maintainedPASI 50, PASI 75, PASI 90, and PGA responses up to at leastWeek 76. In contrast, the withdrawal groups showed a declinein PASI improvement, which began gradually by Week 44.The rate of decline in PASI score accelerated after Week 52,finally decreasing from over 96% in both withdrawal groupsat Week 40 to about 40% at Week 64. In the patientswithdrawn from treatment, the median time to loss ofPASI 75 response was about 15 weeks. Rebound psoriasis wasnot reported in patients who were withdrawn fromtreatment. Eighty-six percent of patients who reinitiatedSTELARA achieved PASI 75 within 12 weeks of reinitiation,with similar response rates observed in all treatment groups.33
FIGURE 2. Percentage of patients who responded at Weeks 12 and 28 in PHOENIX 13100100STELARA (ustekinumab) 45 mg (n 255)STELARA 90 mg (n 256)Placebo (n 403020203%02%PASI 75PASI 9059%49%45%40301062%73%66%61%56%5042%*37%*STELARA 45 mg (n 250)STELARA 90 mg (n 243)Placebo to STELARA 45 mg (n 123)Placebo to STELARA 90 mg (n 119)104%0PGA Clearedor MinimalPASI 75Week 12PASI 90PGA Clearedor MinimalWeek 28*P 0.0001 vs placebo.phase. Patterns of common adverse events were similar duringthe placebo-crossover and randomized-withdrawal phases.The most common serious adverse events observed duringthese phases included infections (3 patients), malignancies(2 patients), cardiovascular events (2 patients), and a stroke(1 patient). No dose response was seen in the rates of adverseevents, serious adverse events, or adverse events leading tostudy agent discontinuation. The percentage of patients withabnormal hematologic and chemistry laboratory measures,including liver and renal function tests, were low and generallycomparable between the groups treated with STELARA andplacebo.3Adverse eventsIn PHOENIX 1, adverse events were generally mild, notserious, and did not require treatment adjustments (Table 2).The most commonly reported adverse events were upperrespiratory tract infections, nasopharyngitis, headache, andarthralgia. Serious adverse events occurred in 2 patientsreceiving placebo (1 patient with pneumonia and 1 patientwith a psychotic disorder); 2 patients receiving STELARA 45 mg (1 patient with a stroke and 1 patient withhypertension); and 4 patients receiving STELARA 90 mg(2 patients with serious infections, 1 patient with coronaryartery disease, and 1 patient with worsening psoriasis). Nomalignancies were reported during the placebo-controlledTABLE 2. Adverse events reported through Week 12 in PHOENIX 13STELARA 45 mg (n 255)STELARA 90 mg (n 255)Placebo (n 27%Nasopharyngitis10%8%9%Upper respiratory tract infection7%6%6%0 1% 1% 1%2% 1% 1%2%2%Serious infectionsSerious adverse events†Adverse events leading to withdrawal of STELARA Reprinted from The Lancet, Vol. 371, Leonardi CL, et al; for the PHOENIX 1 study investigators. Efficacy and safety of ustekinumab, a humaninterleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial(PHOENIX 1), pages 1665-1674, 2008, with permission from Elsevier.†An adverse event that resulted in any of the following outcomes: death, a life-threatening condition, inpatient hospitalization or prolongation ofexisting hospitalization, persistent or significant disability or incapacity, or a congenital anomaly or birth defect, irrespective of its relationship tostudy agent.4Please see Important Safety Information on pages 8-9 and accompanying Full Prescribing Information andMedication Guide for STELARA on pages 10-15.
STELARA FOR MODERATE TO SEVERE PLAQUE PSORIASISBy Jeffrey M. Sobell, MD, Assistant Professor of Dermatology, Tufts University School of Medicine; Director,Psoriasis Treatment Center, SkinCare Physicians; and Chief Dermatologist, Ora Clinical Research“STELARA is the first FDA-approved IL-12/IL-23inhibitor to treat moderate to severe plaquepsoriasis. The arrival of this drug was highlyanticipated. Basic science has demonstrated thatboth IL-12 and IL-23 are proinflammatory cytokineswhich are important in the pathogenesis of psoriasis.Additionally, polymorphisms for the IL-23 receptorand for p40, a subunit common to both IL-12 andIL-23, may promote susceptibility to developingpsoriasis. Thus, IL-12 and IL-23 are highly attractivetherapeutic targets for this disease.PHOENIX 1 and PHOENIX 2 are two large phase 3trials that examined the safety and efficacy ofSTELARA in subjects with moderate to severeplaque psoriasis. The results of both studies areconsistent. The improvements seen in psoriasis withtwo starter doses at Weeks 0 and 4 are rapid. Patientsbegan to see benefits within 2 to 3 weeks of the initialdose. At Week 12, two-thirds of patients haveachieved PASI 75 and are almost clear of psoriasis.After the third dose at Week 16, PASI 75 responsewas observed in more than 75% of patients. AtWeek 28, both 45 mg and 90 mg doses were studied.In patients weighing 100 kg, 45 mg was alsoshown to be efficacious. However, 90 mg resulted ingreater efficacy in these patients.During the randomized withdrawal period inPHOENIX 1, those subjects that received placebo hada slow and controlled return of their psoriasis withoutany cases of rebound. A high majority of subjectsthat remained on therapy with maintenance dosesevery 12 weeks maintained PASI 75 throughout76 months of the trial (80-90%). This durabilityis notable and a strength of the drug.Thus far, the safety profile of STELARA has beenfavorable and generally well tolerated. Commonside effects include mild headache, pharyngitis,fatigue, and uncomplicated upper respiratory tractinfections. As with other immunosuppressiveagents, serious adverse reactions observed in thesePHOENIX 2PHOENIX 2 was the second, major clinical trial that soughtto assess the efficacy and safety of STELARA in patients withmoderate to severe psoriasis for up to 52 weeks. In addition,PHOENIX 2 looked to determine if dosing intensificationwould improve response in patients who had a partialresponse to initial treatment. The primary endpoint was theproportion of PASI 75 responders at Week 12. Majorsecondary endpoints included the proportion of patients witha PGA score of Cleared or Minimal at Week 12, and theproportion of partial responders rerandomized betweenWeeks 40 and 52 who demonstrated PASI 75 response every8 weeks vs every 12 weeks. The eligibility criteria forPHOENIX 2 are presented in Table 1.4Study designPHOENIX 2 was divided into 3 phases: (1) a placebocontrolled phase from Weeks 0 to 12, (2) a placebo-crossoverand active-treatment phase during Weeks 12 to 28, and (3) arandomized-dose-intensification phase during Weeks 28 to52 (Figure 3). At baseline, patients were randomly assignedto receive STELARA 45 mg or STELARA 90 mg atWeeks 0 and 4, and then every 12 weeks, or placebo. Of thepatients receiving placebo, half were randomized to crossover to STELARA 45 mg at Weeks 12, 16, and every12 weeks thereafter; the other half received STELARA 90 mg according to the same schedule.4trials includedserious infections,malignancies, andone case ofreversible posteriorleukoencephalopathy Jeffrey M. Sobell, MDsyndrome (RPLS). Priorto initiating treatment, patients should be evaluatedfor tuberculosis. Patients with any clinically importantactive infection should not receive STELARA , norshould live vaccines be given to patients receivingSTELARA . STELARA should be discontinued if RPLSis suspected.STELARA is a noteworthy addition to ourarmamentarium in treating moderate to severeplaque psoriasis. The unique mechanism of action,convenient dosing options, and favorable benefit/risk profile are highly attractive attributes todermatologists and to patients.”At Week 28, those responders who had initially beenrandomized to receive STELARA and achieved PASI 50,but PASI 75, were rerandomized to continue to eitherreceive the drug every 12 weeks or intensified dosing every8 weeks. Patients not achieving PASI 50 at Week 28discontinued treatment, and patients achieving PASI 75at Week 28 continued to receive STELARA every 12weeks. Efficacy and safety parameters were assessedthrough Week 52.4ResultsSignificantly more patients treated with STELARA achieved PASI 75 in both groups (67% and 76%,respectively) compared with 4% in the placebo group(P 0.0001; Figure 4). At Week 12, a PGA assessment scoreof Cleared or Minimal was achieved by 68% and 74% ofpatients who received STELARA 45 mg or STELARA 90 mg, respectively, vs 5% of patients in the placebogroup (P 0.0001; Figure 4). PASI 50, PASI 75, PASI 90,and PASI 100 were achieved by a significantly greaterproportion of patients treated with STELARA at Week 12than those patients who had been given placebo. AfterWeek 12, response rates in the patients who crossed overfrom placebo to active treatment with STELARA weresimilar to those seen in the patients initially randomizedto the respective STELARA dose at baseline.45
ScreenWeek -4RANDOMIZATIONRANDOMIZATIONFIGURE 3. Week 0 through Week 52 study design for PHOENIX 24GROUP 1STELARA (ustekinumab) 45 mg at Weeks 0, 4, then every 12 weeksGROUP 2STELARA 90 mg at Weeks 0, 4, then every 12 weeksSTELARA 45 mg every 8 weeksSTELARA 45 mg every 12 weeksSTELARA 90 mg every 8 weeksSTELARA 90 mg every 12 weeksGROUP 3aSTELARA 45 mg at Weeks 12, 16, then every 12 weeksGROUP 3Placebo at Weeks 0 and 4GROUP 3bSTELARA 90 mg at Weeks 12, 16, then every 12 weeksPlacebo-crossover andactive-treatment phasePlacebo-controlled phase012Randomized dose-intensification phase5228*Reprinted from The Lancet, Vol. 371, Papp KA, et al; for the PHOENIX 2 study investigators. Efficacy and safety of ustekinumab, a humaninterleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial(PHOENIX 2), pages 1675-1684, 2008, with permission from Elsevier.*At Week 28, non-responders (PASI 50) discontinued treatment with STELARA . Partial responders (PASI 50 to 75) treated with STELARA were randomly assigned to receive treatment either every 8 or 12 weeks. Responders (PASI 75) continued treatment every 12 weeks. All partialresponders who were initially assigned to receive placebo received doses every 8 weeks at Week 28.4tended to have a higher body weight and more marked orsevere disease as measured by the PGA. For patients weighing 100 kg (220 lbs), the recommended dose is 45 mg initiallyand 4 weeks later, followed by 45 mg every 12 weeks. Forpatients weighing 100 kg (220 lbs), the recommended dose is90 mg initially and 4 weeks later, followed by 90 mg every 12weeks. In patients weighing 100 kg, 45 mg was also shown tobe efficacious. However, 90 mg resulted in greater efficacy inthese patients.1,4At Week 28, more than 90% of all patients treated withSTELARA achieved PASI 50 response. Patients who werePASI 75 responders at Week 28 and continued to receiveSTELARA every 12 weeks typically sustained responseuntil Week 52.4Twenty-three percent (93 patients) in the STELARA 45 mggroup and 16% (65 patients) in the 90 mg group were partialresponders at Week 28.4 When compared with those patientswho responded to dosing every 12 weeks, partial respondersFIGURE 4. Percentage of patients who responded at Weeks 12 and 28 in PHOENIX 24100100STELARA 45 mg (n 409)STELARA 90 mg (n 411)Placebo (n 410)908076%†7067%79%8074%††STELARA 45 mg (n 397)STELARA 90 mg (n 400)Placebo to STELARA 45 mg (n 193)Placebo to STELARA 90 mg (n 04030302020104%1%5%070%70%61%65%52%43%100PASI 75PASI 90Week 12PGA Clearedor MinimalPASI 75PASI 90PGA Clearedor MinimalWeek 28†P 0.0001 vs placebo.6Please see Important Safety Information on pages 8-9 and accompanying Full Prescribing Information andMedication Guide for STELARA on pages 10-15.
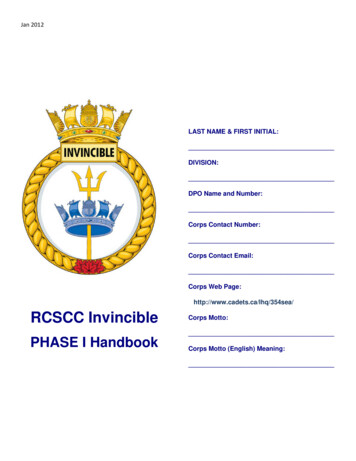
FIGURE 5. Patient treated with STELARA 45 mg every 12 weeksWeek 0—PASI score 16.1Week 12—Achieved PASI 75Week 52—Achieved PASI 75Images are used with permission by Centocor Ortho Biotech Inc.Adverse eventsIn PHOENIX 2, adverse events were generally mild and didnot require modification of treatment. During the placebocontrolled phase, rates of infections were the same across all 3groups (Table 3). Serio
Full Prescribing Information and Medication Guide for STELARA on pages 10-15. Phase 3 Clinical Trials Support STELARA (ustekinumab) for the Treatment of Moderate to Severe Plaque Psoriasis 2 STELARA is a subcutaneously administered biologic approved by the