Transcription
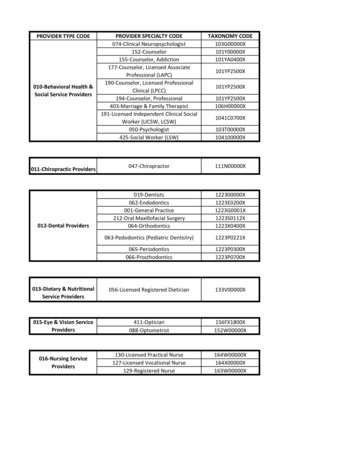
www.indianamedicaid.comIndiana Health Coverage ProgramsMonthly NewsEDSP.O. Box 7263Indianapolis, IN 46207-7263Provider Monthly NewsletterNL200505May 2005Table of ContentsAcronyms Used in this Newsletter. 1Provider News. 2Provider Eligibility Maintenance and Disenrollments. 2Revisions to Radioimmunotherapy Services. 2Billing Changes for BOTOX and Myobloc Injections . 3File Exchange Updates . 4Provider Profile Now Available in Web InterChange . 5Corrections to the 2005 Annual HCPCS Update. 5New Provider Manual Available. 7State-Wide Hoosier Healthwise Mandatory MCO Transition . 8Dental Services . 12RBMC Carve Out Dental Guidelines . 12Vision Services . 13Ophthalmologists, Optometrists, and Opticians . 13Provider Workshops . 152005 Second Quarter Workshops for Medicaid Providers . 15Contact Information . 17IHCP Provider Field Consultants, Effective April 1, 2005 . 17Field Consultants for Bordering States. 17Member and Provider Relations Leaders. 17Indiana Health Coverage Programs Quick Reference, Effective April 1, 2005 . 18Provider Workshop Registration . 19Acronyms Used in this Newsletter1915(b)ADAASCAVRCCFCD-ROMCHIPSocial Security Act section referenceAmerican Dental AssociationAmbulatory Surgical CenterAutomated Voice ResponseClaim Correction FormCompact disk, read-only memoryChildren’s Health InsuranceProgramCMSCenters for Medicare & MedicaidServicesCPTCurrent Procedural TerminologyDMEdurable medical equipmentDURDrug Utilization ReviewEDIElectronic Data InterchangeFQHCFederally Qualified Health CenterHCEHealth Care ExcelHCPCS Healthcare Common ProcedureCoding SystemHIPAAHealth Insurance Portability andAccountability ActHPBHealth Professions BureauIACIndiana Administrative CodeICIndiana CodeICD-9-CM International Classification ofDiseases, 9th Revision, ClinicalModificationICF/MRIntermediate Care Facility for theMentally RetardedIEPIndividual Education PlanIFSSAIndiana Family and Social ServicesAdministrationIHCPIndiana Health Coverage ProgramsISPInternet Service ProviderMCOManaged Care OrganizationMHSManaged Health ServiceOIGOffice of the Inspector GeneralOMPPOffice of Medicaid Policy and PlanningOPPSOutpatient Prospective PaymentSystemPAprior authorizationPCCMPrimary Care Case ManagementPHIProtected Health InformationPMPprimary medical providerPro-DUR Prospective Drug Utilization ReviewRAremittance adviceRBMCRisk-Based Managed CareRHCrural health clinicSURSurveillance and Utilization ReviewTPLThird Party LiabilityCurrent Dental Terminology (CDT) (including procedures codes, nomenclature, descriptors, and otherdata contained therein) is copyrighted by the American Dental Association. 2002, 2004 AmericanDental Association. All rights reserved. Applicable Federal Acquisition Regulation System/Departmentof Defense Acquisition Regulation System (FARS/DFARS) Apply.Current Procedural Terminology (CPT) is copyright 2004 American Medical Association. All RightsReserved. No fee schedules, basic units, relative values, or related listings are included in CPT. TheAMA assumes no liability for the data contained herein. Applicable FARS/DFARS restrictions apply forgovernment use.Page 1 of 19For more information visit www.indianamedicaid.com
Indiana Health Coverage ProgramsNL200505Provider Monthly NewsletterMay 2005Provider NewsProvider Eligibility Maintenance andDisenrollmentsProvider Enrollment has implemented averification process that uses HPB data toenhance provider file maintenance. The HPBnow submits monthly electronic provider licensestatus reports to EDS. The statuses permit theProvider Enrollment Unit to disenroll providerswho no longer have active or probationarylicensure.Additionally, information received from theOIG, OMPP, and IFSSA is used to terminateproviders who are not eligible to participate inthe IHCP.The information available to EDS is used togenerate termination letters to providers who nolonger qualify for enrollment in the IHCP.Licensure Renewal and IHCP EligibilityTo participate in the IHCP, all providers arerequired to be duly licensed, registered, orcertified (405 IAC 5-4-1). Licensure renewal isimportant to extend providers’ IHCP eligibility.Non-renewed licenses are reported as expired orinactive on the HPB reports. Providers listed onthe reports are subject to termination. If you donot intend to renew your license, it is importantto report the non-renewal to the EDS ProviderEnrollment Unit. The information should bereported to EDS on a Provider EnrollmentUpdate Form. The form is available on theIHCP Web site at www.indianamedicaid.com.If a provider obtains a new license at a later dateand wishes to participate in the IHCP, theprovider can submit an Provider EnrollmentApplication with their new license number. Theapplication is available on the IHCP Web site atwww.indianamedicaid.com.The following licensure statuses are subject totermination for participation in the IHCP.HPB Statuses for Termination Closed facility Current prerequisites not met Deceased Emergency suspension Expired Expired over three years Inactive Null and void/error RetiredEDSP.O. Box 7263Indianapolis, IN 46207-7263 Revoked Suspended Voluntary SurrenderNon-HPB Termination Reasons Excluded by the OIG and CMS FSSA determination of non-eligible providersPayment for ServicesUnder IC 12-15-22-4, following theirtermination of participation in the IHCP,providers are no longer eligible for payment.Appeal ProcessUnder IC 4-21.5-3-7 and 405 IAC 1-1.5-2,providers have the right to appeal terminationaction. To preserve an appeal, providers mustspecify the reason for the appeal in writing andfile the appeal with the ultimate authority for theagency within 15 calendar days of receipt of atermination letter.Such appeal must be sent to:E. Mitchell Roob Jr., SecretaryIndiana Family and Social ServicesAdministrationc/o Pat Nolting, Director-ProgramOperations, Acute Care402 West Washington Street, Room W382Indianapolis, IN 46204If providers elect to appeal a determination, theymust also file a statement of issues within 60days after receipt of notice of the determination.The statement of issues should conform to 405IAC 1-1.5-2(d) and be sent to the same addressas the appeal request.Revisions to RadioimmunotherapyServicesThis article is to specify revisions to the billinginstructions for radioimmunotherapy servicesusing Zevalin or Bexxar. This articlesupplements the article published in theNovember 2004 provider newsletter, NL200411.Effective October 1, 2004, revenue code 343,Diagnostic radiopharmaceuticals, and revenuecode 344, Therapeutic radiopharmaceuticals,became valid revenue codes. Providers may usethese revenue codes for dates of service on orafter October 1, 2004, to reportradiopharmaceuticals used for the Zevalin orBexxar regimen as listed in Table 5.1.Page 2 of 19For more information visit www.indianamedicaid.com
Indiana Health Coverage ProgramsNL200505Provider Monthly NewsletterMay 2005Table 5.1 – HCPCS Codes for Diagnostic and Therapeutic RadiopharmaceuticalsCodeC1080Code DescriptionSupply of radiopharmaceutical diagnostic imaging agent, I-131tositumomab, per doseRevenue Code(s)343, 636C1081Supply of radiopharmaceutical therapeutic imaging agent, I-131tositumomab, per dose343, 344, 636C1082Supply of radiopharmaceutical diagnostic imaging agent, indium-111ibritumomab tiuxetan, per dose343, 636C1083Supply of radiopharmaceutical therapeutic imaging agent, yttrium 90ibritumomab tiuxetan, per dose344, 636The article in IHCP provider newsletterNL200411 listed HCPCS code Q0084,Chemotherapy administration by infusiontechnique only, per visit, to be reported for theadministration of rituximab in the Zevalinregimen for the treatment of non-Hodgkin’slymphoma. Effective for dates of serviceJanuary 1, 2005, Medicare requires OPPShospital facilities to bill the appropriate CPT code for chemotherapy administration instead ofHCPCS code Q0084. In order to accommodatecross-over claims, providers are required toutilize the appropriate codes listed in Table 5.2for the administration of rituximab in the Zevalinregimen for dates of service on or afterJanuary 1, 2005.Table 5.2 – HCPCS Codes for Chemotherapy AdministrationCodeQ0084Code DescriptionChemotherapy administration by infusion technique only, per visitRevenue Code33596410Chemotherapy administration, intravenous; infusion technique, up to one hour33596414Chemotherapy administration, intravenous; infusion technique, initiation ofprolonged infusion (more than 8 hours), requiring the use of a portable orimplantable pump33596422Chemotherapy administration, intra-arterial; infusion technique, up to one hour33596425Chemotherapy administration, intra-arterial; infusion technique, initiation ofprolonged infusion (more than 8 hours), requiring the use of a portable orimplantable pump335Providers may direct questions about this article to customer assistance at (317) 655-3240 in theIndianapolis local area or 1-800 577-1278.Billing Changes for BOTOX andMyobloc InjectionsThe purpose of this article is to advise providersof changes in billing for BOTOX and Myoblocinjections and provide instructions for billingunused units of Myobloc. Providers maycontinue to bill these injections using HCPCScodes J0585, Botulinum toxin type A, per unit(BOTOX) and J0587, Botulinum toxin type B,per 100 units (Myobloc). Previous instructions inthe IHCP Provider Manual regarding BOTOXinjections are still in effect. Providers shoulddirect additional questions to customer assistanceat (317) 655-3240 in the Indianapolis local areaor 1-800-577-1278.EDSP.O. Box 7263Indianapolis, IN 46207-7263As of July 1, 2005, the IHCP will limitreimbursement for BOTOX and Myoblocinjections to the ICD-9-CM diagnosis codeslisted in Table 5.3. These diagnosis codes reflectmedically necessary diagnoses for theseinjections. Reimbursement of these injectionswill also be limited to one treatment sessionevery three months, per member unless anadditional injection is medical necessary. Themedical record must contain documentation ofthe medical necessity for additional treatmentsessions provided within a three-month period.Page 3 of 19For more information visit www.indianamedicaid.com
Indiana Health Coverage ProgramsNL200505Provider Monthly NewsletterMay 2005Table 5.3 – ICD-9-CM Diagnosis Codes for BOTOX and Myobloc 9.1754.1Due to the short shelf life of Myobloc, wastageof the product may be unavoidable. The IHCPhas adopted the following policy for billingunused units of Myobloc.Myobloc is supplied in 2,500, 5,000, and 10,000units. When billing for Myobloc, the providermust show the number of units given on theclaim form. If a vial is split between two ormore members, the provider must bill theamount of the Myobloc used for each memberand bill the unused amount as wastage on theclaim for the last member injected. If the vial isnot split between two or more members, theprovider may bill the discarded portion to theIHCP. Whenever a provider bills for unusedMyobloc, both the amount of agent actuallyadministered and the amount discarded must bedocumented in the member’s medical record.Providers should follow the instructions alreadyprovided in the IHCP Provider Manualregarding billing unused units of BOTOX.File Exchange UpdatesTo ensure the security of PHI and enhance dataexchange performance, the current EDS directconnection dial-up method of data exchange isbeing eliminated and replaced with a solutionthat requires access to the Internet through alocal ISP. This solution is called File Exchange.File Exchange is provided by the IHCP forsecure file processing, storage, and transfer. It isdesigned to safely and securely collect, store,manage, and distribute sensitive informationbetween the IHCP and provider organizations.EDSP.O. Box 7263Indianapolis, IN 46207-7263333.83333.84333.89All trading partners connecting directly with theIHCP to exchange data are required to transitionto using File Exchange during the next fewmonths.Advantages of File Exchange Ensures secure data transfer between tradingpartners. Faster uploads and downloads – Dependentupon the chosen method of connection. Possible cost savings – Eliminates longdistance telephone charges for directconnection dial-up and the need for adedicated line. Provides capability to send files 24 hours aday, seven days a week. Maintains outgoing files in the tradingpartner’s home directory for 30 days.Note: Providers who send transactionsthrough a clearinghouse are not requiredto make any changes to the way theysubmit to the clearinghouse. Providersare encouraged to contact theirclearinghouse to ensure they are aware ofthe conversion to File Exchange.Additionally, this change does not applyto providers who send interactivetransactions, use Web interChange tosubmit claims, or use the OMNI eligibilitysystem.The IHCP is dedicated to making this anefficient transition for all trading partners. Tohelp simplify the trading partner’s search for anISP, EDS and the IHCP are working with aPage 4 of 19For more information visit www.indianamedicaid.com
Indiana Health Coverage ProgramsNL200505Provider Monthly NewsletterMay 2005service called AllInternetNow to identify Internetaccess options for each trading partner.AllInternetNow is a free service that works withmost ISPs, such as SBC, Verizon, EarthLink andothers. An AllInternetNow search showsavailable ISP options, such as dial-up and DSL,for each trading partner location. Additionally,information packets that contain ISP optioninformation are being sent to each trading partnerlocation over the next few weeks.The File Exchange How To Guide is available toprovide step-by-step assistance to tradingpartners switching from the current method todata exchange to using File Exchange. Anupdated communications guide and updates tothe IHCP Web site, provider newsletters, andbanner page articles are available athttp://www.indianamedicaid.com.Direct questions about File Exchange to the EDSEDI Electronic Solutions Help Desk at(317) 488-5160 in the Indianapolis local area or1-877-877-5182. Questions can also be sent bye-mail to inxixTradingPartner@eds.comProvider Profile Now Available inWeb InterChangeProviders can now view their profiles throughWeb interChange. Accessing Provider Profileallows providers to view information on file withthe IHCP, including name, current addresses andphone numbers, and type and specialties.Groups are also able to view all of the renderingproviders associated with their practice. Inaddition, copies of the Provider Profile can beprinted directly from Web interChange.Check with the Web interChange administratorto obtain the capability to view a ProviderProfile. Additional information about becomingan administrator can be found atWeb Membership FAQs.Corrections to the 2005 AnnualHCPCS UpdateThe CMS released corrections to the 2005 AnnualHCPCS Update. Table 5.4 lists the new codecorrections with coverage determinations, andTable 5.5 lists the deleted code corrections withreplacement codes. Description changes will beautomatically updated in the system. These updateswill be effective retroactively to January 1, 2005.Table 5.4 – Corrections to the New 2005 HCPCS Codes, Effective January 1, 2005Procedure CodeDescriptionPharmacy supply fee for initialG0369immunosuppressive drug(s) firstmonth following transplantPA RequirementsNot applicable for all programs,Not applicable for Package CModifiersProgram CoverageNon-reimbursable for allprograms, Non-reimbursablefor Package CService is billable on thepharmacy claim formG0370Pharmacy supply fee for oral anti- Not applicable for all programs,Not applicable for Package Ccancer, oral anti-emetic orimmunosuppressive drug(s)Non-reimbursable for allprograms, Non-reimbursablefor Package CService is billable on thepharmacy claim formG0371Pharmacy dispensing fee forinhalation drug(s); per 30 daysNot applicable for all programs,Not applicable for Package CNon-reimbursable for allprograms, Non-reimbursablefor Package CService is billable on thepharmacy claim formG0374Pharmacy dispensing fee forinhalation drug(s), per 90 daysNot applicable for all programs,Not applicable for Package CNon-reimbursable for allprograms, Non-reimbursablefor Package CService is billable on thepharmacy claim form(Continued)EDSP.O. Box 7263Indianapolis, IN 46207-7263Page 5 of 19For more information visit www.indianamedicaid.com
Indiana Health Coverage ProgramsNL200505Provider Monthly NewsletterMay 2005Table 5.4 – Corrections to the New 2005 HCPCS Codes, Effective January 1, 2005Procedure CodeDescriptionPA RequirementsNot applicable for all programs,Chemotherapy assessment forG9021Not applicable for Package Cnausea and/or vomiting, patientreported, performed at the time ofchemotherapy administration;assessment Level 1: not at all (foruse in a Medicare-approveddemonstration project)ModifiersProgram CoverageNon-covered for all programs,Non-covered for Package CG9022Chemotherapy assessment forNot applicable for all programs,nausea and/or vomiting, patientNot applicable for Package Creported, performed at the time ofchemotherapy administration;assessment Level 2: a little (for usein a Medicare-approveddemonstration project)Non-covered for all programs,Non-covered for Package CG9023Chemotherapy assessment forNot applicable for all programs,nausea and/or vomiting, patientNot applicable for Package Creported, performed at the time ofchemotherapy administration;assessment Level 3: quite a bit (foruse in a Medicare-approveddemonstration project)Non-covered for all programs,Non-covered for Package CG9024Chemotherapy assessment forNot applicable for all programs,nausea and/or vomiting, patientNot applicable for Package Creported, performed at the time ofchemotherapy administration;assessment Level 4: very much(for use in a Medicare-approveddemonstration project)Non-covered for all programs,Non-covered for Package CG9025Chemotherapy assessment forNot applicable for all programs,pain, patient reported, performed at Not applicable for Package Cthe time of chemotherapyadministration, assessment Level1: not at all (for use in a Medicareapproved demonstration project)Non-covered for all programs,Non-covered for Package CG9026Chemotherapy assessment forNot applicable for all programs,pain, patient reported, performed at Not applicable for Packag
to report the non-renewal to the EDS Provider Enrollment Unit. The information should be reported to EDS on a Provider Enrollment Update Form. The form is available on the IHCP Web site at www.indianamedicaid.com. If a provider obtains a new license at a later date and wishes to participate in the IHCP, the prov