Transcription
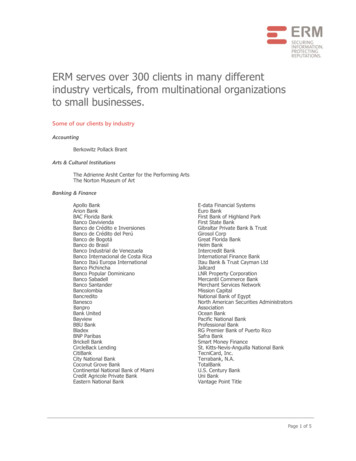
THIS PATHWAYSERVES AS A GUIDEAND DOES NOTREPLACE CLINICALJUDGMENT.CLINICAL PATHWAY:Emergency Department AsthmaInclusion Criteria: 1 yrs old, previous diagnosis of asthma or 2 previous episodes of wheezing, MPIS 5Exclusion Criteria: 1 yrs old, bronchiolitis or pneumonia as primary diagnosis, chronic cardiac or lung disease other than asthmaInitial Assessment (MPIS 5):Dexamethasone 0.6 mg/kg (max 16 mg) PO/IM(Can substitute with prednisolone/prednisone/methylprednisolone 2 mg/kg at initialprovider s discretion. Can omit if already on oral steroids.)MPIS 5-6 MPIS 6 MPIS 7Albuterol 4 puffs MDI/spacer(with teach) ORAlbuterol 2.5 mg nebCalculate MPISAlbuterol 5 mg/Ipratropium 500 mcgvia nebulizerMPIS 7 Discharge Criteria/Instructions: MDI/spacer teach F/u with PCP in 2-3 days Medications: Albuterol PRN*Consider Prednisolone/Prednisone for patients thatmight benefit from longer steroids. Start 24 hoursafter Dexamethasone dose.MPIS 6MPIS 7-8Observe for 1 hour ReassessCalculate MPIS MPIS 6Albuterol 4 puffsMDI/spacer(with teach)if not already doneMPIS 7 Discharge Criteria andInstructions: MDI/spacer teach F/u with PCP in 2-3 days Medications: Albuterol q4hr*Consider Prednisolone/Prednisone for patients that mightbenefit from longer steroids. Start24 hours after Dexamethasonedose.LAST UPDATED: 10.21.19MPIS 6MPIS 7 Long Albuterol treatment: 20 kg: 10 mg over 1 hour 20 kg: 20 mg over 1 hour Reassess in 15-30 minutesCalculate MPISMPIS 9-10Medications:Albuterol 5 mg nebq2hrED provider to placeorder InitiateAlbuterol weanRT will rescore MPISand speak withprovider to placeappropriateAlbuterol orderNursing:Place PIV ifinadequate oralintake, or unable totake oral steroids Medications:Resume continuousAlbuterol atprevious doseED provider to placeorder InitiateAlbuterol weanRT will rescore MPISand speak withprovider to placeappropriateAlbuterol orderNursing:Place PIV ifinadequate oralintake, or unable totake oral steroidsMPIS 11-12 Medications:Resume continuousAlbuterol atprevious doseED provider to placeorder InitiateAlbuterol weanRT will rescore MPISand speak withprovider to placeappropriateAlbuterol orderNursing:Place PIV Admission:Admit to MS (PHM or Pulmonary if patient is known to them)See Inpatient Asthma Pathway At time of transfer:Re-assess patient and calculate MPISInform attending and admitting team if MPIS is increasingHold transfer if MPIS 13 and consider PICU consultCONTACTS: ERIC HOPPA, MD KRISTIN WELCH, MD 2019 Connecticut Children’s Medical Center. All rights reserved. 19-004Reassess in 15-30 minutesCalculate MPISMPIS 13 Medications:Resume continuousAlbuterol at 20 mg/hrConsider additionaltherapies per PICUconsultation (e.g,methylprednisolone ifnot done, MgSO4,terbutaline)Nursing:Place PIV (if not done)Consults:Consult PICU attendingin ED: observe in ED forfurther improvementvs admission to PICUAdmission:- Admit to MS floor or PICUin discussion with IMT andPICU attending- If to be admitted to MS floor,ED provider to place orderInitiate Albuterol wean . RTwill rescore MPIS and speakwith provider to placeappropriateAlbuterol order.
THIS PATHWAYSERVES AS A GUIDEAND DOES NOTREPLACE CLINICALJUDGMENT.CLINICAL PATHWAY:Inpatient AsthmaInclusion Criteria: 1 yrs old, inadequate response to ED asthma treatment (see ED Asthma Pathway)Exclude Criteria: 1yr old, primary diagnosis of bronchiolitis or pneumonia, active cardiac disease MPIS 11 Admit to Medical/ Surgical UnitOxygen: Titrate per orderOral Steroid:oPrednisone or Prednisolone 1mg/kg/dose q12hr; 12 yr old:max 60 mg/day, 12 y/o: max 80 mg/day (Start 24 hr afterdexamethasone. Total steroid course: 5 days)oOR give additional dose of Dexamethasone 0.6 mg/kg (max16mg) PO/IM prior to dischargeDetermine initial MPISIf poor PO, place PIV and administer IVF with potassiumUse asthma-specific H&P to document asthma severity and control(Appendix A, Appendix B, Appendix C)Consider ordering medications for bedside delivery on admissionInitiate Phase 1:Albuterol via continuous neb:o 20kg: 10 mg/hro20kg: 20 mg/hrInitiate Albuterol Wean Protocol*oOption: If improving on 20 mg/hr, wean to10 mg/hr prior to going to q2hrIf not tolerating oral steroid:oMethylprednisolone 1 mg/kg/dose IV q6hr( 12 yr old: max 60 mg/day; 12 max 80 mg/day) Improvement?(MPIS 6 x2) NoInitiate Phase 3Albuterol MDI w/ spacer 8 puffs q4hr(nebulizer can be used if pt sleeping orunable to perform proper MDI technique)Continue Inhaled Corticosteroids (AppendixA, Appendix B, Appendix C, Appendix D),and consider ordering medications forbedside delivery if not doneDiscontinue O2 when RA sat 92%Intermittent pulse ox once off O2Vital signs q4hr, MPIS q4hrComplete Asthma EducationSupply nebulizer or spacer, if needed Initiate Phase 2 and followpathway Increase Albuterol to20 mg/hr if on 10 mg/hrNotify attendingObtain PICU consultConsider Mg sulfateImprovement?YesContinue on pathwayas MPIS dictatesYesMPIS 13 x 1 Discontinue CR monitorVital signs q4hr, MPIS q2hrDiscontinue O2 when RA sat 92%Intermittent pulse ox once off O2 Improvement?(Two consecutive scores inappropriate range)NoInitiate Phase 2:Albuterol MDI w/ spacer 8 puffs q2hr(nebulizer can be used if patient sleeping or unable toperform proper MDI technique)Initiate Albuterol Wean Protocol*Assess severity and treatment recommendations, startInhaled Corticosteroids (Appendix A, Appendix B,Appendix C, Appendix D)Initiate Asthma Education and home treatment plan Place PIV, if not already doneCR monitor w/continuous pulse oximetryVital signs q4hr, MPIS q2hrInitiate Asthma EducationMPIS 7-10YesDischarge Criteria:Off supplemental oxygen, MPIS 5 on q4hr albuterol, hydrated without need for IVFs,asthma home management plan of care complete, asthma education complete and familygiven copy, appropriate follow up in placeDischarge Medications (to be outlined in Asthma Action Plan) Albuterol MDI with spacer: 4 puffs (or 2.5mg via neb) q4hr while awake Total oral steroid x3-5 days (prednisone/prednisolone vs 2nd dose of dexamethasone) Controller therapy (Appendix C, Appendix D), based on chronic severity (Appendix A,Appendix B) Screen for Flu vaccine (Oct-March); administer if indicatedContinue on pathwayas MPIS dictatesNoConsider transferto PICU* ALBUTEROL WEAN PROTOCOL: RT s wean Albuterolaccording to this MPIS-drivenprotocol Wean when two consecutivescores are in appropriaterange RT s inform MD/APRN/PA ofALL changes in Albuteroldosing Any escalation in carerequires an exam by MD/APRN/PA at bedside MD/APRN/PA can authorizevariance from protocolMPIS SCORING TOOLO2 Saturation(RA)AccessoryMuscle UseScoreI:E RatioScoreScore 1000 30 20011121-140101-120131-4521-3512Insp/Exp:Good asedaeration3 160 1403 60 e 3 yr old 3 yr old Score 6 yr old 6 yr old Score 120NoneSevereCONTACTS: CHRISTINA GIUDICE, APRN ALEX HOGAN, MD ANAND SEKARAN, MDLAST UPDATED: 11.11.19Respiratory Rate003Heart RateNone: GoodaerationEndexpiratory 95% 90%WheezingNEXT PAGE 2019 Connecticut Children’s Medical Center. All rights reserved. 19-004The following tests and treatmentsare NOT routinely indicated for thetreatment of asthma: Ipratropium bromide shouldnot be administered after 24hours of hospitalization Chest x-rays (features typicallyassociated with positive chestx-ray findings include fever,no family history of asthma,and localized lung examfindings) Antibiotics (unless diagnosedwith a bacterial infection)
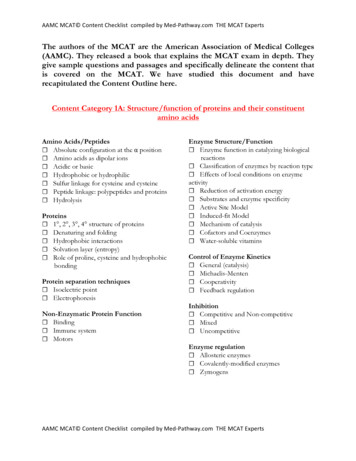
CLINICAL PATHWAY:Inpatient AsthmaAppendix A: Simplified Controller FlowchartTHIS PATHWAYSERVES AS A GUIDEAND DOES NOTREPLACE CLINICALJUDGMENT.Assessing Asthma Severity and Treatment Recommendations: Ages 5 and UpSymptom Frequency12Assess andDOCUMENTAsthma Controlfor 2 Weeks Priorto ExacerbationNight timeawakeningsAlbuterol forsymptom control312 Years Old4None0-1/yearConsult (PRN)Throughout the day 1x/weekEvery Night 2 days/weekDailySeveral times perdayMinor LimitationSome LimitationExtremely Limited2/year with more frequent or intense events greater severityIf on meds, takingappropriately*?NOWorst symptomdocumented abovedetermines severityTreatmentRecommendation(NHLBI STEPCORRELARY)Daily3-4x/month2 days/weekIf currently onmedication & wellcontrolled, continuecurrent treatment5-11 Years Old 2 days/week butNOT daily2x/monthInterfere withnormal activityExacerbationsrequiring systemicsteroidsDetermineseverity if newdiagnosis ofasthmaClassify AsthmaSeverity2 days/weekIntermittentMild PersistentYESIncrease Step by 1UNLESS well controlled(all green answers above)Moderate Persistent(STEP 3)If starting tx: 1 PuffFluti casone 110 BIDIf stepping up tx: 1 PuffFluti casone 110 BID MontelukastOR 2 Puffs Fl uticasone/Salmeterol 45/21 BID /MontelukastSevere Persistent(STEP 3 or 4)(STEP 1)Albuterol PRN(STEP 2)2 Puffs Fluticasone44 BID(STEP 1)Albuterol PRN(STEP 3 or 4)(STEP 3)Fluticasone/2 Puffs Fluticasone(STEP 2)Salmeterol 11544 BID 2 Puffs Fluticasonemcg/21 mcg 2 PuffMontelukast OR 244 BIDBID vs FluticasonePuff Fluticasone 110110mcg 2 Puffs BIDBID Montelukast2 Puff Fluticasone/Salmeterol 115/21 BIDORConsult PulmonaryConsult Pulmonology If: Patient Requires Step 5 Treatment, Or High Dose Inhaled Steroids(2 Puffs 110 for 5-11yo, 2 puffs 220 for 12 year old)*Taking Controller Medications Appropriately: Taking medications as prescribed 80% of the time (self report, pharmacy refills) Using correct technique (using a spacer correctly)If insurance does not cover the recommended medication, see below for equivalent doses of inhaled steroidsDosingConversionChartFluticasone/ Budesonide/ Mometasone/Salmeterol ticasone(Flovent)Beclomethasone(Qvar)44 mcg40 mcg45/21 mcg80/4.5 mcg100/5 mcg110 mcg80 mcg115/21 mcg 160/4.5 mcg200/5 mcgRETURN TOTHE BEGINNINGCONTACTS: CHRISTINA GIUDICE, APRN ALEX HOGAN, MD ANAND SEKARAN, MDLAST UPDATED: 11.11.19 2019 Connecticut Children’s Medical Center. All rights reserved. 19-004Montelukast 6 years old 4mg daily;6-14 years old: 5mg daily; 14 years old: 10mg daily
LAST UPDATED: 11.11.19RETURN TOTHE BEGINNINGCONTACTS: CHRISTINA GIUDICE, APRN ALEX HOGAN, MD ANAND SEKARAN, MDAsthma exacerbationsrequiring oral systemiccorticosteroids‡FEV1 /FVCFEV1 (% predicted)Lung functionInterference withnormal activitySABA use forsymptom control(not to prevent EIB )Nighttime awakeningsSymptomsComponents ofSeverityNotapplicable0Ages0–4 yearsAges 12 yearsNormal† 85%Ages5–11 yearsAges 12 years 2 exacerb.in 6 months,or wheezing 4x peryear lasting 1 dayAND riskfactors forpersistentasthmaNotapplicable 2 days/weekbut not daily1–2x/monthNormal† 80%Notapplicable3–4x/monthAges0–4 yearsAges 12 years75–80%60–80%Some limitationDailyReduced 5%†60–80% 1x/week but not nightlyDailyAges5–11 yearsModeratePersistent 2/yearStep 1Step 3 75% 60%Extremely limitedStep 3Step 3Step 3medium-doseICS optionor Step 4Consider short course of oral systemic corticosteroids.Step 3medium-doseICS optionFor children 0–4 years old, if no clear benefit is observed in 4–6 weeks, consider adjusting therapy or alternate diagnoses.In 2–6 weeks, depending on severity, assess level of asthma control achieved and adjust therapy as needed.Step 2Relative annual risk of exacerbations may be related to FEV1 .Ages 12 yearsindicate greater underlying disease severity. For treatment purposes, patients with 2 exacerbations may be considered to have persistent asthma, even in the absence of impairment levels consistent with persistent asthma.† Normal FEV1 /FVC by age: 8–19 years, 85%; 20–39 years, 80%; 40–59 years, 75%; 60–80 years, 70%.‡ Data are insufficient to link frequencies of exacerbations with different levels of asthma severity. Generally, more frequent and intense exacerbations (e.g., requiring urgent care, hospital or intensive care admission, and/or oral corticosteroids)Step 4or 5Reduced 5%† 60%Often 7x/weekThroughout the dayAges5–11 yearsSevereSeveral times per dayNotapplicable 1x/weekAges0–4 yearsGenerally, more frequent and intense events indicate greater severity.Generally, more frequent and intense events indicate greater severity. 80% 80%Minor limitation 2 days/week butnot daily and not morethan once on any day3–4x/month 2 days/week but not dailyAges0–4 yearsMildConsider severity and interval since last asthma exacerbation. Frequency and severity may fluctuate over time for patients in any severity category.0–1/year 80%Normal FEV1betweenexacerbations 80%Normal FEV1betweenexacerbationsNone 2 days/week 2x/month 2 days/weekAges5–11 yearsIntermittentAbbreviations: EIB, exercise-induced bronchospam; FEV1 , forced expiratory volume in 1 second; FVC, forced vital capacity; ICS, inhaled corticosteroid; SABA, short-acting beta2-agonist.The stepwise approach is meantto help, not replace, the clinicaldecisionmaking needed to meetindividual patient needs.(See “Stepwise Approach forManaging Asthma Long Term,”page 7)Recommended Step forInitiating TherapyRisk 2019 Connecticut Children’s Medical Center. All rights reserved. 19-004ImpairmentLevel of severity (Columns 2–5) is determined by events listed in Column 1 for both impairment (frequency and intensity of symptoms and functional limitations) and risk (ofexacerbations). Assess impairment by patient’s or caregiver’s recall of events during the previous 2–4 weeks; assess risk over the last year. Recommendations for initiating therapybased on level of severity are presented in the last row.(in patients who are not currently taking long-term control medications)INITIAL VISIT: CLASSIFYING ASTHMA SEVERITY AND INITIATING THERAPYCLINICAL PATHWAY:Inpatient AsthmaAppendix B: NHLBI Asthma ClassificationTHIS PATHWAYSERVES AS A GUIDEAND DOES NOTREPLACE CLINICALJUDGMENT.Asthma Care Quick Reference5
RETURN TOTHE BEGINNINGCONTACTS: CHRISTINA GIUDICE, APRN ALEX HOGAN, MD ANAND SEKARAN, MDLAST UPDATED: 11.11.19 2/year16–19 1.51–2Not applicable60–80%1–3x/week 2 days/weekAges 12 yearsNot applicableEvaluation requires long-termfollow-up care.Consider severity and interval since last asthma exacerbation.2–3/yearNot applicable75–80%60–80% 2 days/weekSome limitation 2x/month 2 days/week ormultiple times on 2 days/weekAges5–11 yearsNot Well ControlledNot applicable 3/yearNot applicableMaintain current step.Consider step down if well controlled for at least3 months.Step up at least1 stepStep up 1 step3–4Evaluation requires long-termfollow-up care. 15Not applicableReevaluate in 2 weeks to achieve control.Step up 1–2 steps.Consider short course of oral systemic corticosteroids.Before step up in treatment:Review adherence to medication, inhaler technique, and environmental control. If alternative treatment was used,discontinue and use preferred treatment for that step. For side effects, consider alternative treatment options.For children 0–4 years, if no clear benefit observed in 4–6weeks, consider adjusting therapy or alternative diagnoses.Reevaluate in 2–6 weeks to achieve control.Step up 1 step 60% 4x/weekAges 12 yearsNot applicable 2/yearNot applicable 75% 60%Several times per dayExtremely limited 2x/weekThroughout the dayAges5–11 yearsVery Poorly ControlledNot applicable 1x/weekAges0–4 yearsMedication side effects can vary in intensity from none to very troublesome and worrisome.The level of intensity does not correlate to specific levels of control but should be considered in the overall assessment of risk.Evaluation requires long-termfollow-up care.Regular follow-up every 1–6 months.Not applicable0–1/yearNot applicableNot applicable 1x/month 2 days/weekAges0–4 yearsindicate poorer asthma control.† Minimal important difference: 1.0 for the ATAQ; 0.5 for the ACQ; not determined for the ACT.‡ ACQ values of 0.76–1.4 are indeterminate regarding well-controlled asthma.§ Data are insufficient to link frequencies of exacerbations with different levels of asthma control.Generally, more frequent and intense exacerbations (e.g., requiring urgent care, hospital or intensive care admission, and/or oral corticosteroids)Abbreviations: ACQ, Asthma Control Questionnaire ; ACT, Asthma Control TestTM; ATAQ, Asthma Therapy Assessment Questionnaire ; EIB, exercise-induced bronchospasm; FVC, forced vital capacity; FEV1, forced expiratory volume in 1 second;SABA, short-acting beta2-agonist.The stepwise approach is meantto help, not replace, the clinicaldecisionmaking needed to meetindividual patient needs.(See “Stepwise Approach forManaging Asthma Long Term,”page 7)Recommended Actionfor TreatmentTreatment-relatedadverse effectsReduction in lunggrowth/Progressive lossof lung functionAsthma exacerbationsrequiring oral systemiccorticosteroids§ 20ACT0Not applicable 80%Not applicable 80% 80% 0.75‡Not applicableNot applicable 2 days/weekNone 2 days/week 2 days/week butnot more thanonce on each day 2x/monthAges 12 yearsAges5–11 yearsWell Controlled 1x/month 2 days/weekAges0–4 yearsACQATAQValidated questionnaires†FEV1 /FVCFEV1 (% predicted)or peak flow(% personal best)Lung functionSABA use forsymptom control(not to prevent EIB )Interference withnormal activityNighttime awakeningsSymptomsComponents of ControlImpairment 2019 Connecticut Children’s Medical Center. All rights reserved. 19-004Risk6Level of control (Columns 2–4) is based on the most severe component of impairment (symptoms and functional limitations) or risk (exacerbations). Assess impairment by patient’s or caregiver’srecall of events listed in Column 1 during the previous 2–4 weeks and by spirometry and/or peak flow measures. Symptom assessment for longer periods should reflect a global assessment,such as inquiring whether the patient’s asthma is better or worse since the last visit. Assess risk by recall of exacerbations during the previous year and since the last visit. Recommendations foradjusting therapy based on level of control are presented in the last row.FOLLOW-UP VISITS: ASSESSING ASTHMA CONTROL AND ADJUSTING THERAPYCLINICAL PATHWAY:Inpatient AsthmaAppendix B: NHLBI Asthma ClassificationTHIS PATHWAYSERVES AS A GUIDEAND DOES NOTREPLACE CLINICALJUDGMENT.Asthma Care Quick Reference
STEPWISE APPROACH FOR MANAGING ASTHMA LONG TERMGenerally, more frequent and intense exacerbations (e.g., requiring urgent care, hospital or intensive care admission, and/or oral corticosteroids)The stepwise approach tailors the selection of medication to the level of asthma severity (see page 5) or asthma control (see page 6).The stepwise approach is meant to help, not replace, the clinical decisionmaking needed to meet individual patient needs.ASSESSCONTROL:STEP UP IF NEEDED (first, check medication adherence, inhaler technique, environmental control, and comorbidities)STEP DOWN IF POSSIBLE (and asthma is well controlled for at least 3 months)STEP 6STEP 5STEP 4STEP 3STEP 2STEP 1At each step: Patient education, environmental control, and management of comorbiditiesIntermittentAsthma0–4 years of agePreferredTreatment†SABA asneededPersistent Asthma: Daily MedicationConsult with asthma specialist if step 3 care or higher is required. Consider consultation at step 2.low-dose ICSmedium-doseICSmedium-doseICS either LABA ormontelukasthigh-dose ICS either LABA ormontelukasthigh-dose ICS either LABA ormontelukast oral corticosteroidsAlternativeTreatment†,‡cromolyn ormontelukastIf clear benefit is not observed in 4–6 weeks, and medication technique and adherence are satisfactory,consider adjusting therapy or alternate diagnoses.Quick-ReliefMedication SABA as needed for symptoms; intensity of treatment depends on severity of symptoms. With viral respiratory symptoms: SABA every 4–6 hours up to 24 hours (longer with physician consult). Consider shortcourse of oral systemic corticosteroids if asthma exacerbation is severe or patient has history of severe exacerbations. Caution: Frequent use of SABA may indicate the need to step up treatment.IntermittentAsthma5–11 years of agePreferredTreatment†indicate poorer asthma control.SABA as neededPersistent Asthma: Daily MedicationConsult with asthm
Instructions: MDI/spacer teach F/u with PCP in 2-3 days Medications: Albuterol q4hr *Consider Prednisolone/ Prednisone for patients that might benefit from longer steroids. Start 24 hours after Dexamethasone dose. MPIS 11-12 Medications: Resume continuous Albuterol at 20 mg/hr