Transcription
Treatment andRecovery In PsycHosisPsychosis Care Pathwayand Narrative
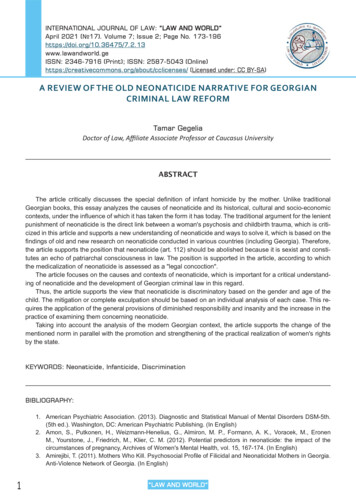
Psychosis Care Pathway and NarrativePsychosis Care Pathway and NarrativeRoutine ReferralTreatment andRecovery In PsycHosisPreventionand EarlyDetectionScreenReferralreceivedTel. triageusing screeningchecklist to: determineurgency considermedication,social,psychologicaland physicalhealth needsHolisticAssessmentMDTDiscussion‘At risk ofpsychosis’assessment:Involvingmedical, nursingand socialcare staff asminimum toagree: engagement medication,social,psychologicaland physicalhealth needs patient andcarer views outcomemeasures incl.PROM provisionalformulation/diagnosis prioritiesfor careplanningCare Plan/CPADelivery of CareReview of Care PlanDischargeCollaborative planningfrom first contact:Engagement from firstcontact (incl. assertive):If deterioration in mental health/crisis/relapse: Safety and crisis planAs indicated:Plan with patient/serviceuser, carers and GP ifover 6-12 months: Safeguarding (adult/child) S ocial care Social care (incl.education, vocation/IPS,accommodation) M edication Medicationmanagement(incl. Clozapine) Psychologicalinterventions (seestepped pathway) i dentify any deterioration early and fast track c onsider acute care pathway P sychologicalinterventions M DT discussion (CPA if criteria met) to reviewmedication, social, psychological and physicalhealth needs; update care plan P hysical health c onsider advance statements S ubstance misuse p atient and carer views C arers support c ommunication with GP W RAP/Recovery College r eview outcome measures incl. PROM Physical health (Lestertool and NICE); perinatal Substance misuseneeds s table and functioningwell n o medication or stablemedication n ot detained a cute care pathway notneededComplete crisis andcontingency plansComprehensivecommunication withprimary care, patientand carer Carers supportScreenAssessmentWithin24 hoursFirst face to facecontact within7 daysMedicationscreen within3 days ofreferral if onprescribedmedicationMDTDiscussionCare Plan/CPADelivery of CareReview as Required by Personal PlanCommence within14 days of referralWeekly face to face: if first episodeWithin 7 daysof assessmentAllocation of a carecoordinator and care planwithin 14 days of referralEarlier medicalreview ifconcernsFormulation by medicwithin 21 days ofassessmentDischarge/signpost ifpsychosispathway notappropriateWeekly: if medication changes, changing mental state, current risks, carerconcerns, specific interventionsWeekly/biweekly: if difficulties engaging in servicesEvery 4 weeks: consider Clozapine if no response to antipsychoticmedication. If mental state is settled, consider increasing review to 3 monthlythen 6 monthlyAnnual review: (if not indicated sooner) of Care Plan/CPA (incl. items listed inCare Plan / CPA box above). Completion of outcome measures
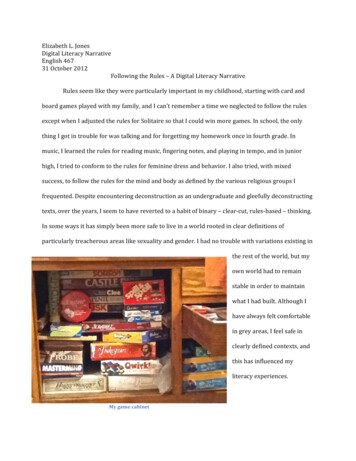
Psychosis Care Pathway and NarrativePsychosis Care Pathway and NarrativeCrisis and Acute CareTreatment andRecovery In PsycHosisScreenHolistic AssessmentMDT DiscussionCare Plan/CPADelivery of CareReviewReferralreceivedCentred around views ofpatient and carer (reviewassessment if one alreadypresent)Involving medical,nursing and social carestaff as minimum toagree: Update care plan A ssertively engage ifneeded M DT discussion (CPA if criteria met) toreview mental state, medication, social,psychological & physical health needs;update care plan engagement provisional formulation/diagnosis determineurgency considermedication,social,psychologicaland physicalhealth needs medication, social,psychological andphysical health needs priorities forcare planning Risk managementplan Physical health Safeguarding(adult/ child) Social issues patient and carer views Family issues outcome measures incl.PROM MedicationManagement plan Begin/adjustmedication,(crisis management),social care unlesscontra-indicated Initiate psychologicalinterventions (seestepped pathway) A dvanced statement W RAP, vocational needs R eview outcome measures incl. PROMWorsening mental state:Transfer toCommunity Team M DT discussion R eview needs andplan care includingcrisis plan Comprehensivecommunication withcommunity team,primary care, patientand carer m onitor risk Carers support m onitor changes Consider psychologicalinterventions m onitor compliance Commence dischargeplanningReview care plan m onitor self careReview psychological interventions(see stepped pathway)ScreenAssessmentMDT DiscussionCare Plan/CPADelivery of CareReview as per Personal Crisis PlanWithin4 hoursUrgent – Face to facewithin 24 hoursWithin 24 hours ofassessmentWithin 24 hours ofassessment, considermedicationCommence within 24-48hours of assessmentIn crisis: daily or twice daily if needed for medication compliance,interventions, review of risk and mental state and need for inpatient care, etc.Medication review withinthis time frameReview of frequency via MDT. Discuss response to treatmentAllocation of a carecoordinator within14 days7 day follow up after discharge from acute pathwayMHA assessment ifneededMedication review within48 hours of referralFormulation with medicwithin 72 hours ofassessmentDischarge CPA (if inpatient) within 7 days of assessment
Psychosis Care Pathway and NarrativeContributions and AcknowledgementsClinical Lead and Chair: Shanaya RathodSteering Group: Alison Griffiths, Carolyn Asher, Chris Woodfine, Christie Garner,Claire Morrish, David Butler, David Kingdon, Dawn Pease, Deborah Tee, Jason Hope,Jeremy Rowland, Katherine Newman-Taylor, Lars Hansen, Michael James, Nicola Abba,Paul Tabraham, Pippa North, Rob Kurn.AcknowledgementsWe would like to acknowledge the support of all patients, carers, clinicians, commissioners,Healthwatch and partners from other agencies who have supported and contributed to this workthrough the co-production workshops and engagement events.We are grateful to the Wessex Academic Health Science Network for leading on this work in theWessex region.We would also like to thank Dr Geraldine Strathdee (National Clinical Director, Mental Health) forsupporting this work.This project has received funding from NHS England (Regional Innovation Fund) and a small grantfrom the Royal College of Psychiatrists.6
Psychosis Care Pathway and NarrativeIntroductionTRIumPH (Treatment and Recovery In PsycHosis) is a care pathway for people withpsychosis that aims to promote good clinical practice. The pathway details the servicesthat people experiencing psychosis can expect during different phases of their care.The pathway is informed by the success of other pathways (eg. stroke and cardiovascular),current evidence base and by best practice guidelines. It aligns itself to the NICE Guidelinefor Schizophrenia (2014), the National Audit of Schizophrenia (NAS)1, NICE QualityStandards (2015)2 and to the Access and Waiting Time Standards for Mental HealthServices (2015/16)3.The NICE Quality Standards (2015) and Mental Health Access and Waiting TimesStandards (2015/16) state that:l Adults with first episode psychosis will be treated with a NICE approved care packagewithin 2 weeks of referral. This is measured by allocation of a care coordinator in aservice which provides the range of NICE approved treatments.l Adults with psychosis or schizophrenia are offered cognitive behavioural therapy forpsychosis.l Family members of adults with psychosis or schizophrenia are offered familyintervention.l Adults with psychosis or schizophrenia that have not responded adequately totreatment with at least 2 antipsychotic drugs are offered Clozapine.l Adults with psychosis or schizophrenia who wish to find or return to work are offeredsupported employment programmes.l Adults with psychosis or schizophrenia have specific comprehensive physical healthassessments.l Adults with psychosis or schizophrenia are offered combined healthy eating andphysical activity programmes, and help to stop smoking.l Carers of adults with psychosis or schizophrenia are offered carer-focused educationand support programmes.The pathway is underpinned by ten Principles of Care which define the overall approach,treatments, and standards. A key expectation of this pathway is that it supports timelydelivery of evidence-based interventions by appropriately trained and supervised staff.Care is shaped by the monitoring of treatment outcomes using clinician and patient/service user completed outcome measures.This pathway document covers aspects of care from assessment, through to treatmentdelivery, training and provision of clinical supervision, to discharge from secondary careservices. The pathway operates for all people experiencing psychosis who are involvedwith Southern Health NHS Foundation Trust (SHFT), regardless of the care team providingthe service; see diagram below.Psychosis in the elderly is complex. There are multiple co-morbidities and thepsychopathology is not necessarily the same as in adults. The general principles of thispathway will apply to functional psychosis although necessary adaptations will berequired to ensure that person centred care can be provided to this group.7
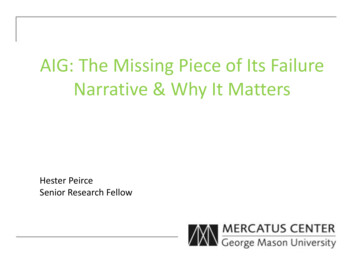
Psychosis Care Pathway and NarrativePerson with possible psychosisYoung personEIP ortransitionfromCAMHSto adultservicesAdultsOlder personPrinciples of CareCare for individualswith psychosisReferences1 The National Audit of Schizophrenia (NAS) (2014) has been consulted in creating this pathway. The NASfocuses, in the main, on the prescribing of medication. Psychological Therapy is noted as an interventionto be offered where the ‘‘illness’ is treatment resistant’; this does not align to the NICE Guideline Update(2014). Currently the NAS shows that the majority of patient/service users were offered no psychologicaltherapy even in the case of standard treatment ‘resistance’. Given this, and the need to ensure thepathway draws on all possible evidence base or recommended treatment options for psychosis, thepathway aligns itself to the NICE Guideline (2014) rather than the NAS.2 National Institute for Health and Care Excellence (NICE). NICE Quality Standards: Psychosis andSchizophrenia in Adults (2015).3 NHS England. Guidance to support the introduction of access and waiting time standards for mentalhealth services (2015/16).8
Psychosis Care Pathway and NarrativePrinciples of CareThis psychosis pathway is supported by the ten principles of care. These principlesunderpin the approach that all people experiencing psychosis can expect from the careprovided by SHFT.Principle 1: People who experience psychosis can expect care which is underpinned by up-to-datebio-psycho-social understandings of the development and maintenance of psychosisand recovery. Respect will be given to people who wish to explore alternativeframeworks for understanding their experiences (alternative to illness model).Principle 2: People who experience psychosis can expect care to be directed towards recoveryand delivered in an atmosphere of optimism and hope.Principle 3: People who experience psychosis will be supported to maximise the amount ofcontrol they have in their lives at every point in the pathway.Principle 4: Treatments offered for the experience of psychosis will be evidence-based and alignto best practice guidelines such as the NICE Guideline for Schizophrenia (2014).People experiencing psychosis can expect such interventions to be delivered byappropriately trained and clinically supervised staff, and that psychosocial outcomesfrom any treatment will be appropriately measured to ensure recovery and progressis transparent to both the patient/service user and staff.Principle 5: People on the psychosis pathway will have the same right to be consulted andinformed about any issue in the same way as patient/service users on any otherpathway. This includes being consulted about service developments, being given thechance to express opinions about services and having access to information.Principle 6: Across all phases of the episode of psychosis and across all care teams, carepackages will include a combination of psychopharmacological, psychological,and psychosocial interventions to create an optimal treatment environment.Psychological strategies will be supported by care staff with equal weighting withpsychopharmacology so as to support recovery and not undermine it by creating aunilateral dependency on medication as a means of alleviating distress.Principle 7: Care packages offered will be ‘holistic’; taking into account all domains of theperson’s life which are impacted on by the experience of psychosis and provideadvice about appropriate support.Principle 8: People experiencing psychosis will be treated with respect at all times, and theirdignity and safety will be protected by care staff during the times when they maybecome overwhelmed by their experience.Principle 9: Psychosis is personally meaningful to each person who experiences it, althoughthis is not always obvious to others. As such the content and origin of thoughts,worries and fears, and the behaviours they drive will be given due regard and notdismissed as meaningless.Principle 10: Stigma has a significant impact on recovery from psychosis. People experiencingpsychosis can expect to be treated in a de-stigmatising environment which willbe driven by the behaviours of staff, expressions of understandings by staff, andadherence to these Principles of Care. Early detection can reduce the duration ofuntreated psychosis so people should receive treatments and support as soon asthey need them.9
Psychosis Care Pathway and NarrativeCare of the IndividualPerson with possible psychosisEngagementAsk questions to identify if theperson may have psychosis. Seekinformation from primary andsecondary sourcesCluster 10if first episodeof ce misuse,anxiety, depression,trauma, learningdifficulties ordisability)Cluster 16-Dualdiagnosis withsubst
contingency plans Comprehensive communication with primary care, patient and carer Routine Referral Treatment and Recovery In PsycHosis. Psychosis Care Pathway and Narrative Psychosis Care Pathway and Narrative Screen Referral received determine urgency consider medication, social, psychological and physical health needs Holistic Assessment Centred around views of patient and