Transcription
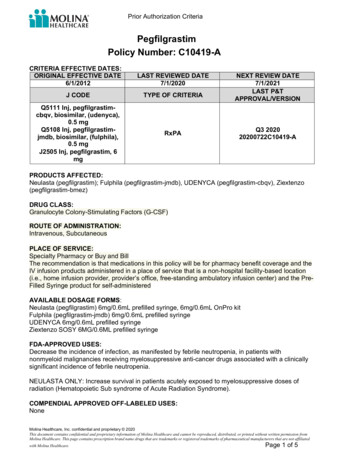
Prior Authorization CriteriaPegfilgrastimPolicy Number: C10419-ACRITERIA EFFECTIVE DATES:ORIGINAL EFFECTIVE DATE6/1/2012LAST REVIEWED DATE7/1/2020J CODETYPE OF CRITERIAQ5111 Inj, pegfilgrastimcbqv, biosimilar, (udenyca),0.5 mgQ5108 Inj, pegfilgrastimjmdb, biosimilar, (fulphila),0.5 mgJ2505 Inj, pegfilgrastim, 6mgRxPANEXT REVIEW DATE7/1/2021LAST P&TAPPROVAL/VERSIONQ3 202020200722C10419-APRODUCTS AFFECTED:Neulasta (pegfilgrastim); Fulphila (pegfilgrastim-jmdb), UDENYCA (pegfilgrastim-cbqv), Ziextenzo(pegfilgrastim-bmez)DRUG CLASS:Granulocyte Colony-Stimulating Factors (G-CSF)ROUTE OF ADMINISTRATION:Intravenous, SubcutaneousPLACE OF SERVICE:Specialty Pharmacy or Buy and BillThe recommendation is that medications in this policy will be for pharmacy benefit coverage and theIV infusion products administered in a place of service that is a non-hospital facility-based location(i.e., home infusion provider, provider’s office, free-standing ambulatory infusion center) and the PreFilled Syringe product for self-administeredAVAILABLE DOSAGE FORMS:Neulasta (pegfilgrastim) 6mg/0.6mL prefilled syringe, 6mg/0.6mL OnPro kitFulphila (pegfilgrastim-jmdb) 6mg/0.6mL prefilled syringeUDENYCA 6mg/0.6mL prefilled syringeZiextenzo SOSY 6MG/0.6ML prefilled syringeFDA-APPROVED USES:Decrease the incidence of infection, as manifested by febrile neutropenia, in patients withnonmyeloid malignancies receiving myelosuppressive anti-cancer drugs associated with a clinicallysignificant incidence of febrile neutropenia.NEULASTA ONLY: Increase survival in patients acutely exposed to myelosuppressive doses ofradiation (Hematopoietic Sub syndrome of Acute Radiation Syndrome).COMPENDIAL APPROVED OFF-LABELED USES:NoneMolina Healthcare, Inc. confidential and proprietary 2020This document contains confidential and proprietary information of Molina Healthcare and cannot be reproduced, distributed, or printed without written permission fromMolina Healthcare. This page contains prescription brand name drugs that are trademarks or registered trademarks of pharmaceutical manufacturers that are not affiliatedwith Molina Healthcare.Page 1 of 5
Prior Authorization CriteriaCOVERAGE CRITERIA: INITIAL AUTHORIZATIONDIAGNOSIS:see FDA-approved uses aboveREQUIRED MEDICAL INFORMATION:IF THIS IS A NON-FORMULARY/NON-PREFERRED PRODUCT FOR INITIAL OR CONTINUATIONOF THERAPY REQUEST: Documentation of trial/failure of or intolerance to a majority (not more than3) of the preferred formulary BIOLOGIC/PDL alternatives for the given diagnosis. If yes, please submitdocumentation including medication(s) tried, dates of trial(s) and reason for treatment failure(s)BIOSIMILAR DRUGS are preferred when requested as a physician administered drug and/orpharmacy formulary product per applicable state regulations and there is a lack of data demonstratingclinical superiority of reference drugs over the FDA approved biosimilar drugs. A referencemedication is approved under the following conditions:1. Treatment with at least two (2) associated biosimilar drug(s) has been ineffective, not tolerated, oris contraindicated (i.e. an allergic reaction to a specific inactive ingredient in the preferred biologicproduct or biosimilar OR an adverse reaction to a specific inactive ingredient in the preferredbiologic product or biosimilar OR therapeutic success while taking a non-preferred biologic productor biosimilar and therapeutic failure while taking the preferred biologic product or biosimilardocumented by patient diary or medical charted notes)[DOCUMENTATION REQUIRED-Document when the preferred biologic product or biosimilar was triedand the length of the trial period, Provide specific clinical documentation of therapeutic failure on thepreferred biologic product or biosimilar whenever possible. Describe the medical problem caused by thepreferred referenced biologic. Vague and non-descriptive symptoms are not adequate rationale (e.g.,stomachache)]A. FEBRILE NEUTROPENIA PROPHYLAXIS IN NON-MYELOID MALIGNANCIES:1. Documented diagnosis of non-myeloid malignancyAND2. Documentation that pegfilgrastim is being used following myelosuppressive chemotherapy[Documentation of current chemotherapy regimen, any previous chemotherapyregimens, and anticipated treatment plan]AND3. (a) Member has a risk of febrile neutropenia (FN) of greater than 20% based on currentchemotherapy regimen (as listed in current ASCO and NCCN guidelines for myeloid growthfactors [See Appendix]OR(b) Member has a risk of febrile neutropenia of 10‑20% based on chemotherapy regimen,and atleast ONE of the following risk factors apply:(i) Prior chemotherapy or radiation therapy(ii)Persistent neutropenia (defined as neutrophil count less than 500 neutrophils/mcLor less than 1,000 neutrophils/mcL and a predicted decline to less than or equal to500neutrophils/mcL over next 48 hours)(iii) Bone marrow involvement by tumor(iv) Recent surgery and/or open wounds(v) Liver dysfunction (bilirubin greater than 2.0 mg/dL)(vi) Renal dysfunction (creatinine clearance less than 50 mL/min)(vii) Age greater than 65 receiving full chemotherapy doseintensityOR(c) Previous neutropenic fever complication from a prior cycle of similarMolina Healthcare, Inc. confidential and proprietary 2020This document contains confidential and proprietary information of Molina Healthcare and cannot be reproduced, distributed, or printed without written permission fromMolina Healthcare. This page contains prescription brand name drugs that are trademarks or registered trademarks of pharmaceutical manufacturers that are not affiliatedwith Molina Healthcare.Page 2 of 5
Prior Authorization CriteriachemotherapyOR4.(d) The member is receiving a dose‑dense chemotherapy regimenANDFOR A NON-FORMULARY REQUESTED DRUG: Documentation or prescriber attestation thatthe alternative formulary agents have been ineffective in the treatment of the patient's disease ormedical condition OR based on both sound clinical evidence and medical and scientificevidence, the known relevant physical or mental characteristics of the enrollee, and knowncharacteristics of the drug regimen, is likely to be ineffective or adversely affect the drug'seffectiveness or member compliance.B. HEMATOPOEITIC SUB SYNDROME OR ACUTE RADIATION SYNDROME:1. Documented diagnosis of member who have radiation injury due to accidental orintentional total body radiation of greater than 2 Grays (Gy)AND2. FOR A NON-FORMULARY REQUESTED DRUG: Documentation or prescriber attestationthat the alternative formulary agents have been ineffective in the treatment of the patient'sdisease or medical condition OR based on both sound clinical evidence and medical andscientific evidence, the known relevant physical or mental characteristics of the enrollee,and known characteristics of the drug regimen, is likely to be ineffective or adversely affectthe drug's effectiveness or member compliance.DURATION OF APPROVAL:Initial authorization: One chemotherapy cycle or 12 weeks, Continuation of Therapy: for up to 6monthsQUANTITY:Requested drug, dose, and frequency is defined Current weight in kilograms (actual body weight)Dose is adjusted if weight is 45kgPatients 10kg: 0.1mg/kgPatients 10-20kg: 1.5mgPatients 21-30kg: 2.5mgPatients 31-44kg: 4mgUp to 2 prefilled syringes (1.2mL) per 28 days (1 prefilled syringe per chemotherapy cycle) Up to 2OnPro kits per 28 days (1 OnPro kit per chemotherapy cycle)PRESCRIBER REQUIREMENTS:Prescribed by or in consultation with a board-certified hematologist, oncologist, or transplantspecialistAGE RESTRICTIONS:One month of age and olderCONTINUATION OF THERAPY:FOR ALL INDICATIONS:1. Member is compliant with pegfilgrastim therapy as verified by prescriber andfill historyAND2. Documentation of clinical benefits to support continuation of treatment including positiveresponse to therapy (i.e. member did not become neutropenic mid-cycle requiring G-CFS)AND3. Documentation of regular lab monitoring (i.e. CBC and platelet count4. ANDMolina Healthcare, Inc. confidential and proprietary 2020This document contains confidential and proprietary information of Molina Healthcare and cannot be reproduced, distributed, or printed without written permission fromMolina Healthcare. This page contains prescription brand name drugs that are trademarks or registered trademarks of pharmaceutical manufacturers that are not affiliatedwith Molina Healthcare.Page 3 of 5
Prior Authorization Criteria5.Documentation of disease CONTINUATION:All other uses of pegfilgrastim and its biosimilars are considered experimental/investigational andtherefore, will follow Molina’s Off-Label policy. Use in routine infection prophylaxis (e.g. adjunctivetherapy to antibiotics in a member with uncomplicated febrile neutropenia, afebrile neutropenia).Continued use beyond 42 days with no response. Concurrent use with other CSF agents(Neupogen, Leukine). Known hypersensitivity to pegfilgrastim or any ingredient in the requestedformulation. E. coli protein hypersensitivity. Receiving chemotherapy with a risk of febrileneutropenia 20% and no significant high risk for complications. Pegfilgrastim will be administered inthe period between 14 days before and 24 hours after administration of cytotoxic chemotherapyOTHER SPECIAL CONSIDERATIONS:NoneBACKGROUND:NoneAPPENDIX:A biosimilar is highly similar version of a brand name biological drug that meets strict controls forstructural, pharmaceutical, and clinical consistency. A biosimilar manufacturer must demonstratethat there are no meaningful clinical differences (i.e., safety and efficacy) between the biosimilar andthe reference product. Clinical performance is demonstrated through human pharmacokinetic(exposure) and pharmacodynamic (response) studies, an assessment of clinical immunogenicity,and, if needed, additional clinical studies.1As costs for biological specialty drugs continue to rise, the growing biosimilar market will benefitproviders and patients by broadening biological treatment options and expanding access to thesemedications at lower costs.Molina Healthcare, Inc. continues to be committed to continually reevaluating Preferred strategiesand applying innovative cost-controls to ensure patients receive safe, effective, and qualityhealthcare. This commitment includes potentially creating a preference for biosimilars when valuecan be added without compromising patient satisfaction and safety.1. Food and Drug Administration. Biosimilar and Interchangeable Products. Retrieved ar-and-interchangeable-products. Accessed October 8, 2019.High risk for chemotherapy induced FN infectious complications because of bone marrowcompromise OR co-morbidity with any of the following risk factors (not an all-inclusive list):Age 65 yearsPoor performance statusPrevious episodes of FNHistory of previous chemotherapy or radiation therapyCompletion of combined chemoradiotherapyBone marrow involvement by tumor producing cytopeniasPre-existing neutropeniaPoor nutritional statusPoor renal functionLiver dysfunction (i.e. elevated bilirubin)Presence of open wound(s) or active infectionMolina Healthcare, Inc. confidential and proprietary 2020This document contains confidential and proprietary information of Molina Healthcare and cannot be reproduced, distributed, or printed without written permission fromMolina Healthcare. This page contains prescription brand name drugs that are trademarks or registered trademarks of pharmaceutical manufacturers that are not affiliatedwith Molina Healthcare.Page 4 of 5
Prior Authorization CriteriaRecent surgery (within the past 12 weeks)More advanced cancerOther serious co-morbiditiesDocumentation Requirements:Molina Healthcare reserves the right to require that additional documentation be made available aspart of its coverage determination; quality improvement; and fraud; waste and abuse preventionprocesses. Documentation required may include, but is not limited to, member records, test resultsand credentials of the provider ordering or performing a drug or service. Molina Healthcare maydeny reimbursement or take additional appropriate action if the documentation provided does notsupport the initial determination that the drugs or services were medically necessary, notinvestigational or experimental, and otherwise within the scope of benefits afforded to the member,and/or the documentation demonstrates a pattern of billing or other practice that is inappropriate orexcessive.REFERENCES:1. Molina Clinical Policy for Granulocyte Colony Stimulating Factors (MCP-108); June 29,20122. Neulasta [package insert]. Thousand Oaks, CA; Amgen Inc; June2018.3. Fulphila [package insert]. Zurich, Switzerland; Mylan GmbH; June 2018.4. Udenyca [package insert]. Coherus Biosciences. Redwood City, CA November 2018.5. Referenced with permission from the NCCN Drugs & BiologicsCompendium(NCCNCompendiumR) pegfilgrastim. National Comprehensive Cancer Network, 2018.6. Chemoradiotherapy with or without granulocyte-macrophage colony-stimulating factor in thetreatment of limited-stage small-cell lung cancer: a prospective phase III randomized study ofthe Southwest Oncology Group Bunn PA Jr, Crowley J, Kelly K, Hazuka MB, Beasley K,Upchurch C, Livingston R, Weiss GR, Hicks WJ, Gandara DR. J Clin Oncol. 1995;13(7):16327. Intensified hyperfractionated accelerated radiotherapy limits the additional benefit ofsimultaneous chemotherapy--results of a multicentric randomized German trial in advancedhead-and-neck cancer.Staar S, Rudat V, Stuetzer H, Dietz A, Volling P, Schroeder M, FlentjeM, Eckel HE, Mueller RP. Int J Radiat Oncol Biol Phys. 2001;50(5):1161Molina Healthcare, Inc. confidential and proprietary 2020This document contains confidential and proprietary information of Molina Healthcare and cannot be reproduced, distributed, or printed without written permission fromMolina Healthcare. This page contains prescription brand name drugs that are trademarks or registered trademarks of pharmaceutical manufacturers that are not affiliatedwith Molina Healthcare.Page 5 of 5
Pegfilgrastim Policy Number: C10419-A . CRITERIA EFFECTIVE DATES: ORIGINAL EFFECTIVE DATE LAST REVIEWED DATE NEXT REVIEW DATE 6/1/2012 . 7/1/2020 . 7/1/2021 : J CODE TYPE OF CRITERIA LAST P&T APPROVAL/VERSION Q5111 Inj, p