Transcription
Rheumatoid Arthritis:BYDr/ Elham Ahmed
Arthritis Inflammation that affecting joints Onsetcan be gradual (chronic), or sudden(acute) symptoms : joint pain and stiffness Other symptomsmay include redness, warmth, swelling,and decreased range of motion of theaffected joints.
Causes of acute arthritis 1-infection: staph. Aureus, strepthaemolyticus, brucellosis,viral, typhoidfever. Metabolic: acute gouty arthritis Collagen: acute rheumatoid arthritis,rheumatic arthritis Trauma, haemophilia
DEFINITION1 Inflammatory disease of peripheral joints,especially the small joints of the hands and feet. Chronic untreated inflammation may lead to jointerosions and joint destruction. Rheumatoid arthritis (RA) is a systemic disease{articular and extra-articular manifestations(cvs,respiratory system, blood, eye, muscle, liver,spleen)}.
Chronic arthritis InfectionMetabolic: goutCollagen diseae: Rh. ArthritisDegnerative: osteoarthritisMiscellaneous: malignancy
Clinical Presentation of RASevere RAEarly RAIntermediate RALatinis KM, et al. The Washington ManualTMRheumatology Subspecialty Consult. Philadelphia, Pa:Lippincott Williams & Wilkins; 2004.
Epidemiology Peak onset is in the fourth or fifth decadefor women and the sixth to eighth decadesfor men Female: Male ratio, 3:1
Pathophysiology3,6 The cause is unknown but risk factors arepresent:1. Hereditary (Genetic, epigenetic)2. Infection (Porphyromonas gingivalis),present in the mouths of people withperiodontal disease linked to rheumatoidarthritis, gut infection.3. Women around 40 years.4. smoking
This radiograph shows significant bone loss between the two roots of atooth (black region). The spongy bone has receded due to infectionunder tooth, reducing the bony support for the tooth.
Pathophysiology autoimmune disease characterized byinflammatory polyarthritis. infiltration of the synovial membrane with– Lymphocytes– Plasma cells– Dendritic cells– Macrophages. CD4 T lymphocytes, including Th1 cells and Th17cells play a central role by interacting with other cellsin the synovium.
Pathophysiology Lymphoid follicles form within the synovialmembrane in which T cell–B cellinteractions lead B cells to producecytokines and autoantibodies, includingRF, L.E cell and ACPA. Synovial macrophages - activated byimmune complexes - produceproinflammatory cytokines, including TNF,IL-1, IL-6 and IL-15.
Pathophysiology Proinflammatory cytokines act on synovialfibroblasts, to promote swelling of thesynovial membrane and damage to softtissues and cartilage. Activation of osteoclasts and chondrocytesdrives destruction of bone and cartilage The RA joint is hypoxic and this promotesnew blood vessel formation(neoangiogenesis).
Pathophysiology The inflammatory granulation tissue(pannus) formed by the above sequenceof events spreads over and under thearticular cartilage, which is progressivelyeroded and destroyed. Later, fibrous or bony ankylosis may occur. Muscles adjacent to inflamed jointsatrophy and may be infiltrated withlymphocytes
McInnes and Schett, NEJM 2011
McInnes and Schett, NEJM 2011
Clinical manifestations for RA Swelling in joints, with or without pain Symmetrical pattern ofaffected joints1. fingers: proximal interpharyngeal joint, metacarpopharyngeal orwrist2. Lower limb: ankle, lateral metatarsopharyngeal joint, big limb joint.3. Head: tempromandibular joint.4. Chest: stenoclavicular joint. Swelling in soft tissues around the joints Joint stiffness upon awakening Lately, hand deformities (ulnar deviation, Z shaped, boutinnare) Subcutaneous nodules in the pressure areas e.g elbow
Clinical manifestations for RA Fatigue, depression, occasional low gradefevers, anemia, general sense of malaise
Diagnostsisof Rheumatoid Arthritis Rheumatoid factor in 85%L.E cells in15%Anti-CCP antibodiesPlain X-ray: obliteration of the space, bonerarefaction and deformities MRI Ultrasound
Rheumatoid Factor Antibody directed against the Fc portion ofIgG Present in approximately 85% of RA patients Found in other conditions, especiallyHepatitis C
Anti-Cyclic Citrullinated Peptide(CCP) Antibodies in RA Anti-citrulline Abs produced in RA synovium Early RA Diagnosis– sensitivity 48%; specificity 96%– seen in 2% of pts with other autoimmunediseases and infections (vs. 14% for RF)– less than 1% of healthy controls Predicts erosive disease Present years before the onset of symptoms.34% of blood samples obtained 2.5 yr beforeonset of symptoms
Plain X-ray
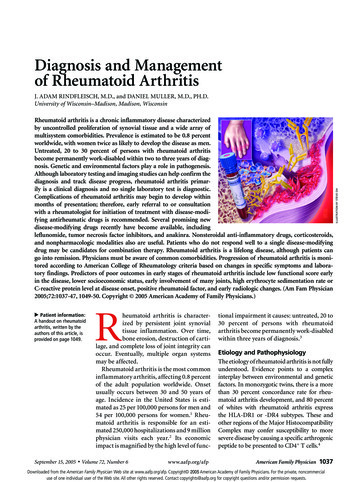
Magnetic Resonance Imaging asa Diagnostic ToolErosions Detected:X-rays vs MRI (%)504540302014100McQueen FM et al. Ann Rheum Dis. 1999;58:156-163.McQueen FM et al. Ann Rheum Dis. 1998;57:350-356.X-rayMRI
Rheumatoid arthritis: episcleritisCopyright 1972-2004 American College ofRheumatology Slide Collection. All rightsreserved.
Rheumatoid arthritis: scleromalacia perforansCopyright 1972-2004 American College ofRheumatology Slide Collection. All rightsreserved.
Treatment NSAIDs Glucocorticoids DMADs :1. D- penicillamine and choloquine methotrexate2. Biologics– TNF alpha inhibition– T-cell inhibition– B cell inhibition– IL-6 inhibition Small molecules
Traditional DMARD SelectionAgentTime toBenefitPotentialToxicityMethotrexate1–2 moModerateHydroxychloroquine2–6 moLowMacular damageSulfasalazine1–3 moLowMyelosuppressionLeflunomide4–12 wkLowDiarrhea, alopecia, rash, headache,risk of immunosuppression infectionMinocycline1–3 moLowHyperpigmentation, dizziness, vaginalyeast infectionsToxicities to MonitorMyelosuppression, hepatic fibrosisand cirrhosis, pulmonary infiltrates
Dr/ Elham Ahmed . Arthritis Inflammation that affecting joints Onset can be gradual (chronic), or sudden . Latinis KM, et al. The Washington ManualTM Rheumatology Subspecialty Consult. Philadelphia, Pa: Lippincott Williams & Wilkins; 2004.