Transcription
Embedded Inferior Vena Cava Filter Removal:Use of Endobronchial ForcepsS. William Stavropoulos, MD, Robert G. Dixon, MD, Charles T. Burke, MD, Joseph M. Stavas, MD,Anand Shah, MD, Richard D. Shlansky-Goldberg, MD, and Scott O. Trerotola, MDPURPOSE: Removing a retrievable inferior vena cava (IVC) filter can be extremely difficult with the use of standardtechniques if the filter is tilted and embedded in the wall of the IVC. The use of rigid endobronchial forceps has beendescribed in case reports to remove embedded IVC filters, and the present report describes the use of this techniqueto remove a series of tip-embedded IVC filters in two separate institutions.MATERIALS AND METHODS: The medical records were reviewed of 21 consecutive patients at two institutions whounderwent attempted IVC filter removal with rigid endobronchial forceps over a 34-month period. The mean age ofpatients was 32.4 years (range, 14.1–54.1 y). The patients had the following filters: Recovery (n ⴝ 6), G2 (n ⴝ 10),Günther Tulip (n ⴝ 4), and OptEase (n ⴝ 1).RESULTS: Rotational or biplane venography was used to confirm that the filters were tilted and embedded in the wallof the IVC in all 21 patients. Rigid endobronchial forceps were used successfully to remove 20 embedded IVC filtersin 21 patients. There was one case of failure to remove an embedded suprarenal G2 filter. There were no majorcomplications.CONCLUSIONS: Rigid endobronchial forceps may be used as a reliable option for removal of embedded IVC filters.J Vasc Interv Radiol 2008; 19:1297–1301Abbreviations:DVT deep vein thrombosis, IVC inferior vena cavaRETRIEVABLE inferior vena cava(IVC) filters are designed to be removed if the filter is no longer neededor may be left in place as a permanentdevice (1,2). Multiple studies havedemonstrated that retrievable filtersare safe to deploy and can be removedwith a high rate of success if cavalfiltration is no longer deemed neces-From the Department of Radiology (S.W.S., A.S.,R.D.S.G., S.O.T.), Division of Interventional Radiology, Hospital of the University of Pennsylvania, 1Silverstein, 3400 Spruce Street, Philadelphia, PA19104; and Department of Radiology (R.G.D., C.T.B.,J.M.S.), Division of Interventional Radiology, University of North Carolina, Chapel Hill, NorthCarolina. Received December 7, 2007; final revisionreceived April 8, 2008; accepted April 15, 2008. Address correspondence to S.W.S.; E-mail: stav@uphs.upenn.eduNone of the authors have identified a conflict ofinterest. SIR, 2008DOI: 10.1016/j.jvir.2008.04.012sary (3–5). However, many retrievablefilters are not retrieved (6). Reasons fornot retrieving an IVC filter include theneed for permanent IVC filtration, theduration of required IVC filtration being longer than the filter’s window ofretrievability, the patient being lost tofollow-up, a large amount of clottrapped in the filter, and technicallyunsuccessful filter removal attempts(2,7).Currently, there are two retrievableIVC filters approved by the UnitedStates Food and Drug Administration:the OptEase filter (Cordis, MiamiLakes, Florida) and the Günther Tulipfilter (Cook, Bloomington, Indiana).Both these filters can be retrieved withthe use of a snare device. The G2 filter(Bard Peripheral Vascular, Tempe, Arizona) is currently approved by theFood and Drug Administration as apermanent device, but it may be removed on an off-label basis with theuse of a 10-F proprietary retrieval de-vice (Recovery Cone; Bard). Similarly,the predecessor to the G2 filter, theRecovery filter (Bard), was approvedas a retrievable filter that could be removed with the Recovery Cone. TheCelect filter (Cook) is another approved permanent filter that can beretrieved on an off-label basis with theuse of a snare. Although the standardtechniques for IVC filter removal aresuccessful in the vast majority of cases,there are instances when filters cannotbe removed with standard techniques(4,8). This is an increasing problemand usually occurs as a result of filtertilt, which then causes the tip of thefilter to be embedded in the wall of theIVC. Alternative techniques for IVCfilter removal have been described, including the use of rigid bronchoscopyforceps (9,10). This article reports theuse of the forceps technique to retrievea variety of tip-embedded filters (Recovery, G2, Günther Tulip filter, andOptEase) at two institutions.1297
1298 Removal of Embedded IVC Filters with Endobronchial ForcepsMATERIALS AND METHODSInstitutional review board approvalwas granted for this retrospectivestudy. Imaging studies and medicalrecords of patients who underwentIVC filter removal with rigid endobronchial forceps (model 4162; Bryan,Woburn, Massachusetts) at two institutions were reviewed and included inthis study. All patients underwent anextensive informed consent processbefore this procedure, and it was explicitly discussed with the patientsthat this represented off-label use ofthe products involved.Over a 34-month period, 21 patientspresented to the interventional radiology divisions of two institutions withIVC filters that could not be removedwith standard techniques because thetip of the filter was embedded in thewall of the IVC. This group included15 female patients and six male patients with a mean age of 32.4 years(range, 14.1–54.1 y). Four of the patients were included in the initial description of this technique (9), andBurke et al (10) subsequently described one of the patients in a casereport.Five of the filters had been initiallyplaced for prophylaxis before bariatricsurgery. Filters had been placed in 10patients who had a history of pulmonary embolism and/or deep veinthrombosis (DVT) with a contraindication to anticoagulation. Five filters hadbeen placed in patients who had a history of trauma with lower-extremitylong bone fractures. One patient washomozygous for factor V Leiden anddeveloped recurrent pulmonary emboli despite anticoagulation 1 week after a miscarriage and dilation and curettage.The filters were removed in 12 patients (57%) because protection fromvenous thromboembolic disease andpulmonary embolism was no longerneeded. In eight of the patients (38%),the filters were referred for removalbecause the patients were able to tolerate anticoagulation. The one patientwith factor V Leiden developed upperabdominal and chest pain more than 3years after insertion and was found tohave a tilted, embedded filter withthree legs that had embolized to herheart and lungs before any attempt atfilter removal was performed. Nine ofthe filters had been placed at outsideinstitutions and were referred to oneof the two medical centers after unsuccessful attempts at filter removal withuse of standard techniques with theRecovery Cone or a snare. In thesepatients referred from outside hospitals, initial venography revealed thatthe tip of the filter was embedded inthe IVC, and therefore the initial removal attempt at our institutions wasmade with the endobronchial forceps.In seven of the patients who were notreferred from outside hospitals, initialcavography demonstrated the tip ofthe filter to be embedded, and the forceps were therefore used as the initial(and only) device to remove the IVCfilters. In five of the patients, the endobronchial forceps were used afteran initial attempt at removal withstandard techniques by the authorsfailed.Before attempted IVC filter removal, all patients underwent imaging with lower-extremity Doppler ultrasound (US) of the deep veins orcomputed tomographic (CT) venography of the IVC with extension to thelower extremities. The US images (n 9) were obtained to evaluate for lowerextremity DVT. The CT venograms (n 12) were obtained to evaluate forDVT and also allowed for evaluationof the IVC and filter before attemptedIVC filter removal to look for filter tiltand clot trapped in the filter.RESULTSNo patient was refused a filter retrieval attempt. The forceps were usedto remove 20 IVC filters in 21 patientsat two institutions (13 at one institution and eight at the other) that couldnot be removed with standard techniques. Therefore, on an intent-to-treatbasis, the success rate of removal withforceps was 95%. No major complications occurred during the retrievals.Retrieval attempts of Recovery IVCfilters (n 6), G2 filters (n 10), andGünther Tulip filters (n 4) were performed via right internal jugular veinaccess. Venography of the IVC and filter was performed in all patients. Rotational venography was performed in12 patients with an injection of 7 mL/sec of nonionic contrast medium (Visipaque; GE Healthcare, London, England) for 12 seconds while the C-armgantry rotated 120 (Multistar TOP orArtis Axiom d-TA; Siemens, Erlangen,September 2008JVIRGermany). In eight patients, the filterswere removed with biplane fluoroscopy guidance (Neurostar; Siemens).When an embedded filter is diagnosed on venography, the key imaging features include an unopacifiedtissue cap around the tip of the filter orprojection of the tip of the filter outside the opacified lumen of the IVC.After detailed venography, a 12- or14-F, 40 cm sheath (Cook) with anaerostatic valve was placed into theIVC from the right internal jugularvein just superior to the filter. Rigidbronchoscopy forceps were placedthrough the sheath just superior to thetip of the filter. The forceps can begently bent to direct the forceps to thetip of the filter. This must be donecarefully, as one set of forceps wasbroken when the tip was bent too aggressively. The forceps were then usedto attempt to grasp the tip of the Recovery, G2, or Günther Tulip filter. Because the tip was embedded, the forceps were used to dissect the tip freefrom tissue around it in six patients.This tissue around tip of the filter wasremoved by pulling the tissue awayfrom the tip with the teeth of the forceps. After the tissue was dissectedfree, the filter was moved into a lesstilted position, more centered into theIVC. This usually happened spontaneously as soon as the tip was dissectedfree with the forceps. The centered filter was then removed with bronchialforceps or the Bard Recovery Cone. In13 patients, after the tissue—which encapsulated the tip of the filter—wasdissected away from the filter, the forceps were used to grab the tip of thefilter and the filter was pulled directlyinto the sheath and removed.In the one case in which the endobronchial forceps were used to removethe OptEase filter, a right femoral approach was used. Rotational venography was performed. A 12-F, 40-cmsheath was then placed from the rightcommon femoral vein into the IVC justinferior to the hook on the OptEasefilter. The tissue encapsulating thehook of the OptEase filter was dissected away using the teeth of forcepsand the filter was then pulled into thesheath and removed.Following IVC filter removal avenogram of the IVC was performedin all patients to evaluate for damageto the IVC or residual thrombus. All
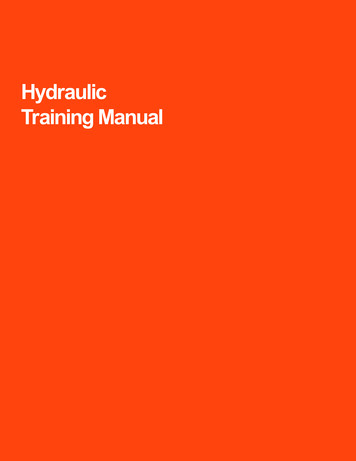
Volume 19Number 9Stavropoulos et al 1299Figure. Subtracted (a) and unsubtracted (b) IVC images demonstrate the tip of a Recovery filter embedded in the wall of the IVC (whitearrows). (c) The endobronchial forceps have been used to grasp the tip of the filter (white arrow). (d) IVC image after removal revealsmild narrowing of the IVC as a result of spasm and a small defect in the IVC that corresponds to the location of the embedded filter(white arrow).filters were inspected to ensure thatthe entire filter was removed.The average filter dwell time was296 days (range, 26 –1,251 d). Preremoval imaging with US and CTvenography revealed that no patientshad lower-extremity DVT. Review ofthe cavograms before filter removal(Figure, parts a,b) revealed that, in100% of cases, the IVC filters weretilted and the tips of the filters wereembedded into the IVC wall. This resulted in a hood of tissue around thetip of the filter. Postremoval venograms (Figure, part d) revealed noevidence of contrast agent extravasation in any of the patients. In sixpatients, a small defect was seen inthe wall of the IVC, which corresponded to the previous location ofthe filter. One of these patients wasfollowed with CT, and at 9 monthsafter filter removal, no caval injurywas evident. In this same patient,two of the secondary struts of theGünther Tulip filter were inadvertently partially disrupted; however,the filter was ultimately removed intact. One subsequent patient alsohad partial disruption of one of thesecondary struts of the Günther Tulip filter. Again, this filter was removed intact. None of these patientsdeveloped symptoms or had anysigns of retroperitoneal hemorrhage.Clinical follow-up in all 20 patientsrevealed no evidence of symptomaticrecurrent PE or symptomatic cavalstenosis or thrombosis after filter removal. Interestingly, the patient withFactor V Leiden was pain-free afterthe removal of her Recovery filter.The endobronchial forceps technique failed in one patient (4.8%). AG2 filter had been placed at an outsidehospital in the suprarenal IVC in apregnant woman who developed DVTduring her first trimester of pregnancy. After the birth of a healthybaby, the patient presented at the outside hospital for possible filter removal. A plain radiograph of the abdomen revealed that the filter wastilted nearly sideways. The patientwas then referred to our center forfilter removal. CT venography and rotational venography revealed a severely tilted filter that had its tip embedded in the wall of the IVC. Theinitial attempt at filter removal wasmade with the endobronchial forceps.After attempting to remove the filterfor 45 minutes, the procedure wasstopped. The tip of the filter could notbe accessed. In addition, multiple attempts to remove the tissue aroundthe embedded cap of the filter werenot successful. The filter was left inplace as a permanent device. No complications occurred during the failedattempt at removal.DISCUSSIONAlthough permanent IVC filtershave an excellent safety profile, latecomplications from these devices dooccur, including an increased risk ofDVT, late device fracture, and migration (1,11–13). The recent introductionand subsequent widespread use of retrievable IVC filters offer the hope ofproviding protection from pulmonaryembolism while decreasing the risks oflong-term filter complications. Thispromise of decreased complicationswill be realized only if the retrievableIVC filters are removed. All currentlyavailable retrievable IVC filters caneasily be removed in the majority ofcases with use of standard techniques(5,14 –16). The difficulty of removingan IVC filter can be increased bylengthened dwell time, thrombus inthe filter, and tilting of the filter (17,18)The issue of filter tilt as the cause ofretrieval failure as a result of the tip ofthe filter being embedded in the IVCwall is not uncommon, occurring in asmany as 11.7% of attempted filter retrievals (7,19 –22). When a filter is unable to be removed with use of standard techniques, it is often left in placeas a permanent device. This is not anoptimal outcome for many patients,as retrievable filters are placed in ayounger group of patients comparedwith the traditional recipients of IVC
1300 Removal of Embedded IVC Filters with Endobronchial Forcepsfilters. In addition, there are no longterm data available showing a decadelong safety record of the currentlyavailable retrievable filters. Many patients do not feel comfortable havingan IVC filter in place if it is no longerneeded. This is especially true whenthey were told this was a retrievabledevice. For these reasons, patients often see removing these filters as a veryhigh priority. However, the risks ofany filter removal procedure must beweighed against the risks of leavingthe filter in place as a permanent device. There are no data to suggest thatretrievable filters are less or more safethan permanent filters when left inplace for many years. Some patientsdo choose to allow the filter to be leftin place rather than undergo attempted removal with the forceps.Alternative techniques to remove afilter that is tilted have been described.Asch (4) described the use of an angled catheter to manipulate a wire toward the side of the filter tilt, whichfacilitates placement of a RecoveryCone over the filter. However, whenthe tip of the filter is embedded in thewall of the IVC, this technique will notwork. Hagspiel et al (8) described atechnique to straighten a tilted filterthat involves placing a tip-deflectingwire through the center lumen of theRecovery Cone. The tip-deflectingwire is then placed through the filterstruts and traction is applied to thewire to straighten the tilted filter. Kuoet al (23) described a technique forremoving a Günther Tulip filter thathad become tilted and embedded inthe wall of the IVC. This techniqueinvolves the establishment of throughand-through guide wire access throughfilter struts and placement of a snareover the two wire ends. After engaging the filter hook and neck, the snareand sheath can be advanced over thefilter and the filter can be removed.This technique was successful in fourpatients, with no treatment failures.Rubenstein et al (7) described a technique of removing embedded IVCfilters by creating a wire loop between the filter legs and pulling thefilter into a sheath. This techniquewas successfully used to remove fourGünther Tulip filters and four Recovery filters.Rigid bronchoscopy forceps wereused in the present study to remove 20IVC filters at two institutions. The pro-cedures were performed by Certificateof Added Qualifications board– certified interventional radiologists. All filters in the present series were not onlytilted, but venograms also showed thetip of each filter to be embedded in thewall of the IVC. Although this technique was successful in all but onepatient in whom it was tried and hasresulted in no permanent sequelae, itis recognized that this is a fairly aggressive technique. Mention of potential life-threatening complications (eg,filter fracture, filter migration, venousperforation) should be included during the consent process. Minor complications have occurred, including minor defects in the wall of the IVC andpartial disruption of the secondarystruts of Günther Tulip filters. The finesecondary struts of the Günther Tulipfilter can be damaged by the teeth ofthe bronchoscopic forceps. Therefore,care must be taken to grasp only thehook of the Günther Tulip filter withthe bronchoscopic forceps, not themore caudal portion of the filter wherethe primary and secondary struts coalesce. Endobronchial forceps shouldbe used in the venous system only if itis demonstrated that the filter tip isembedded and cannot be removedwith the use of standard techniques.At our institutions, the use of bronchial forceps has become the primarymethod for filter removal if preprocedural venography reveals that the tipof the filter is embedded in the wall ofthe IVC. Extended fluoroscopic timesand potential complications such asfilter fracture and dislodgment can beavoided if futile attempts at filter removal are not performed with a snareor Recovery Cone after an embeddedfilter is recognized. In addition, because the forceps enable the operatorto dissect free the tissue covering theembedded filter, this technique mayoffer advantages versus other techniques, which may not successfullydisrupt the fibrous tissue cap.As the use of retrievable filters increases, the need for widely adaptabletechniques to remove embedded IVCfilters will increase. The use of therigid bronchoscopy forceps allows embedded filters to be removed safely inpatients who would otherwise have atilted filter left in place permanentlywhen it is no longer needed.September 2008JVIRReferences1. Kinney TB. Update on inferior venacava filters. J Vasc Interv Radiol 2003;14:425– 440.2. Kaufman JA. Optional vena cava filters: what, why, and when. Vascular2007; 15:304 –313.3. Van Ha TG, Chien AS, Funaki BS, et al.Use of retrievable compared to permanent inferior vena cava filters: a singleinstitution experience. Cardiovasc Intervent Radiol 200
unsuccessful filter removal attempts (2,7). Currently, there are two retrievable IVC filters approved by the United States Food and Drug Administration: the OptEase filter (Cordis, Miami Lakes, Florida) and the Gu nther Tulip filter (Cook, Bloomington, Indiana). Both these filters can be retrieved with