Transcription
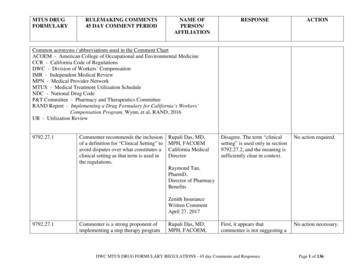
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODNAME OFPERSON/AFFILIATIONRESPONSEACTIONCommon acronyms / abbreviations used in the Comment ChartACOEM - American College of Occupational and Environmental MedicineCCR - California Code of RegulationsDWC - Division of Workers’ CompensationIMR - Independent Medical ReviewMPN - Medical Provider NetworkMTUS - Medical Treatment Utilization ScheduleNDC - National Drug CodeP&T Committee - Pharmacy and Therapeutics CommitteeRAND Report - Implementing a Drug Formulary for California’s Workers’Compensation Program, Wynn, et al, RAND, 2016UR - Utilization Review9792.27.1Commenter recommends the inclusionof a definition for “Clinical Setting” toavoid disputes over what constitutes aclinical setting as that term is used inthe regulations.Rupali Das, MD,MPH, FACOEMCalifornia MedicalDirectorDisagree. The term “clinicalsetting” is used only in section9792.27.2, and the meaning issufficiently clear in context.No action required.First, it appears thatcommenter is not suggesting aNo action necessary.Raymond Tan,PharmD,Director of PharmacyBenefitsZenith InsuranceWritten CommentApril 27, 20179792.27.1Commenter is a strong proponent ofimplementing a step therapy programRupali Das, MD,MPH, FACOEM,DWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesPage 1 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODto work with the proposed drugformulary. This should be a priority ofthe P&T Committee. Any step therapyprogram should be designed to workin conjunction with the definitions andusage of Preferred, Non-Preferred, andUnlisted Drugs as defined underSection 9792.27.1. Any step-therapyprogram must also work seamlesslywith the MTUS guidelines.NAME OFPERSON/AFFILIATIONCalifornia MedicalDirectorRaymond Tan,PharmD,Director of PharmacyBenefitsZenith InsuranceWritten CommentApril 27, 2017When a step therapy hierarchy isestablished, it would be beneficial iffirst line therapies aligned with thePreferred Drug category so thatPreferred Drugs must be tried first, aNon-Preferred Drug second and anunlisted drug only if neither aPreferred Drug nor a Non-PreferredDrug is available or has beenineffective.9792.27.1Because Section 9792.27.21(b)(4)references a therapeutic interchangeprogram and that term maybe new to many people in the industry,commenter recommends adding adefinition for TherapeuticInterchange to 9792.27.1.Rupali Das, MD,MPH, FACOEM,California MedicalDirectorRaymond Tan,PharmDRESPONSEACTIONstep therapy program beadopted in the initial formularyregulations, but is suggesting itbe instituted after the P&TCommittee is formed and canparticipate in consulting on theissue.Second, disagree withcommenter’s suggestion that astep therapy align: Step 1 Preferred, Step 2 - NonPreferred, Step 3 - Unlisteddrugs. The proposed structurewould not align with theMTUS ACOEM guidelinesusage recommendations, whichare not structured in this way.There is far more nuance to theevidence-based treatmentrecommendations based on thepatient’s condition, phase ofcare, and patient comorbidities.Disagree. There are a varietyNo action necessary.of ways to structure atherapeutic interchangeprogram and a step therapyprogram. The definitionsshould not be added until thescope of such programs isDWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesPage 2 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIOD“Therapeutic Interchange meansthe substitution of a drug by apharmacist or payor with a drugthat is a therapeutic alternative orequivalent, with the prescribingprovider’s permission.”NAME OFPERSON/AFFILIATIONRESPONSEDirector of PharmacyBenefitsfurther developed, includingconsulting with the P&TCommittee. Moreover, inrelation to the suggesteddefinition of “TherapeuticInterchange” it would not beappropriate to include“therapeutic equivalent” asthose are drugs identified inthe Orange Book as “A” ratedequivalents, and which alreadymay be substituted by apharmacist, for examplesubstituting a generictherapeutic equivalent for abrand name drug.Zenith InsuranceWritten CommentApril 27, 2017Commenter also recommends addinga definition for step-therapy.Commenter recommends thefollowing new language:Step-therapy means the practice ofbeginning drug therapy for amedical condition with the safestand most cost effective drug andprogressing to other higher risk ormore costly drug therapy, only ifmedically necessary.9792.27.1Commenter notes the definitions forCommenter requests that the DWCconsider identifying how pain pumprefill drugs should be classified andinclude that in the definitions underboth the Formulary regulations andeventually the Physician's FeeSchedule regulations as well.Suzanne HonorVangerov, Esq.May 1, 2017Written CommentDisagree. MTUS Low BackDisorders Guideline does notrecommend the use ofintrathecal pain pumps.However, for existing patientsthe guideline states that itshould not be interpreted asrequiring device removal.Commenter states that thisissue is a “fee scheduleDWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesACTIONNo action necessaryin this regulatoryaction. DWC willconsider these forinclusion in thePhysician FeeSchedule and/or thePharmaceutical FeeSchedule.Page 3 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODNAME OFPERSON/AFFILIATIONRESPONSEACTIONproblem”. It is moreappropriate to address the issuein a future fee schedulerulemaking action.9792.27.1Commenter recommends thefollowing revised language:(f) “Dispense” means: 1) thefurnishing of a drug for outpatient useupon a prescription from a physicianor other health care provider actingwithin the scope of his or her practice,or 2) the furnishing of a drugs foroutpatient use directly to a patient by aphysician acting within the scope ofhis or her practice.(s) “Perioperative Fill” means thepolicy set forth in section 9792.27.12allowing dispensing of identified NonPreferred drugs without prospectivereview where the drug is prescribedfor outpatient use within during theperioperative period and meetsspecified criteria.Commenter states that the changesrecommended in (f) are necessary toclarify that the definition of dispenserelates to outpatient drugs for theCWCIBrenda RamirezDenise NiberClaims and MedicalDirectorEllen Sims LangilleGeneral CounselMay 1, 2017Written CommentDisagree. The definitionproposed in the regulationsmirrors the definition of“dispense” set forth in theBusiness and Professions Code§4024. It is beneficial to alignthe workers’ compensationdefinition with the definitiongenerally applicable topharmaceuticals statewide.Moreover, in relation to boththe definition of “dispense”and “perioperative fill,” otherprovisions of the proposedregulations make it clear thatthe MTUS Drug List and theformulary are applicable todrugs dispensed for “outpatientuse”; duplication of thisconcept in the definition of“dispense” or “perioperativefill” would not improve theclarity of the regulation.DWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesNo action necessaryregarding (f).No action necessaryregarding (s).Page 4 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODpurpose of these sections.As currently proposed in (s), the drugmust be prescribed during theperioperative period. If the intent isfor the drug to be prescribed for useduring the perioperative period, therecommended modification isnecessary for clarification, otherwise aprescribing physician could, on the 4thday after surgery, prescribe a 90-daysupply of a drug.(z) “Surgery” means a surgicalprocedure that has “010”, or 10 GlobalDays, listed for the reimbursable CPTcode as found in the MedicareNational Physician Fee ScheduleRelative Value File incorporated intothe Official Medical Fee Schedule.Commenter states that adding adefinition for “surgery” is necessary toclarify under what specific conditionsthe “Perioperative Fill” policy isapplicable. Spinal injections such astrigger points injections and epiduralsteroid injections, as well asNAME OFPERSON/AFFILIATIONRESPONSEACTIONRegarding the possibility thatthe perioperative fill could beused to prescribe a 90-daysupply on the 4th day aftersurgery, that would not bepossible under the regulationsas drafted. The perioperativefill is specified as not toexceed a supply specified inthe MTUS Drug List.Currently anticoagulants areset at a maximum 14-daysupply, and all other drugs areset at a 4-day supply.Disagree. The perioperativeNo action necessaryregarding (z).fill must be prescribed inaccordance with the MTUSGuidelines. The medicalnecessity for a perioperativefill drug may not align with theglobal days designation in thephysician fee schedule.Additionally, although theZero day procedures areunlikely to warrant opioids,they may be requireddepending for individualpatient circumstances, whichthe doctor will address usingDWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesPage 5 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODNAME OFPERSON/AFFILIATIONdiagnostic procedures such asendoscopy, are all procedures thatwould not normally necessitate theprescribing of drugs for outpatient useof during the perioperative period butcould be considered surgery. Add thedefinition in order to avoidunnecessary frictional costs.9792.27.1(a)RESPONSEACTIONprofessional judgment, and inaccordance with the MTUS.A pattern of inappropriateprescribing by a physician forthe perioperative fill is likelyto be identified onretrospective review and willbe addressed through theremedies set forth in LaborCode section 4610.Commenter recommends addingclarification to the word “device” tospecify that it means “devices” thatare used to deliver a drug to the body.Rupali Das, MD,MPH, FACOEMCalifornia MedicalDirector“(a) “Administer” means the directapplication of a drug or drug deliverydevice to the body of the patient byinjection, inhalation, ingestion, orother means.”Raymond Tan,PharmDDirector of PharmacyBenefitsDisagree. The definition in the No action necessary.regulation conforms to thedefinition of “administer” inthe Business and ProfessionsCode section 4616, which is inDivision 2 - Healing Arts, inChapter 9 – Pharmacy.Zenith InsuranceWritten CommentApril 27, 20179792.27.1(e)The current proposed definition forcompounded medications could leaveopen a loophole for compounds thatinvolve only active ingredients or foronly altered ingredients.Brian Allen, VicePresident,Governmental AffairsOptum Workers’Comp and Auto No--Agree in part. The proposeddefinition should be modifiedto be more comprehensive so aloophole in the definition of“compounded drug” is notDWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesModify proposedlanguage to referencethe governingregulationspromulgated by thePage 6 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODRecommend defining “compoundedmedication” as follows:A pharmaceutical product thatresults from the combining,mixing, or altering of one or moreactive or inactive ingredients,excluding flavorings, tocreate a customized drug (nottypically produced by amanufacturer) for an individualpatient in response to a licensedpractitioner’s prescription.9792.27.1(e)The current definition is overlyspecific may create unintendedloopholes. This dangerous level ofspecificity is unnecessary since theproposed rules already recognize aprotected class of FDA-approved“combination drugs” as a separatedefined, category.NAME OFPERSON/AFFILIATIONRESPONSEACTION- FaultApril 28, 2017Written CommentMay 1, 2017Oral Commentcreated. The regulation will bemodified to tie thecompounded drug definition toregulations of the CaliforniaPharmacy Board and federallaw governing compounding.It would be preferable to tiethe definition of “compoundeddrug” to the governingstatutes; the suggesteddefinition may still be subjectto creating loopholes and canbe out of sync with therelevant legal authority.California Board ofPharmacy, and thegoverning federalstatute.Ben RobertsExecutive VicePresident and GeneralCounselPRIUMApril 29, 2017Written CommentAgree in part. See responseabove to comment of BrianAllen, Optum, dated April 28,2017.See action describedabove in relation tothe response to BrianAllen, Optum.Suggested revision:“Compounded drug” means a drugthat is created by combining one ormore active pharmaceuticalingredients, and one or more inactiveingredients, to meet specific patientDWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesPage 7 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODNAME OFPERSON/AFFILIATIONRESPONSEACTIONmedical needs that cannot be met withFDA-approved prescription drugs,FDA-approved non-prescriptiondrugs, or other drugs commerciallyavailable in the marketplace;however, this definition shall notinclude “Combination drugs” asdefined in 9792.27.1(d).9792.27.1(h)Section 9792.27.1(h) includes adefinition of Expedited Review;however, this term is also defined inSection 9792.6.1(j) [utilization reviewregulations]. Commenterrecommends only referencing theprior definition and not including anyadditional language.Rupali Das, MD,MPH, FACOEMCalifornia MedicalDirectorAgree.Raymond Tan,PharmDDirector of PharmacyBenefitsCommenter recommends revision:“(h) “Expedited review” means theutilization review conducted prior tothe delivery of the requested medicalservices, in accordance with LaborCode section 4610 and title 8,California Code of Regulationssection 9792.6.1 et seq., where theinjured worker’s condition is suchthat the injured worker faces animminent and serious threat to hisZenith InsuranceWritten CommentApril 27, 2017DWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesRevise section9792.27.1(h) todelete the repetitionof the definitionlanguage included insection 9792.6.1(j).For clarity, add theword “expedited”:“(h) “Expeditedreview” means theexpedited utilizationreview conductedprior to the deliveryof the requestedmedical services ”Page 8 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODNAME OFPERSON/AFFILIATIONRESPONSEACTIONRobert Blink, MDPresidentWesternOccupational &EnvironmentalMedical Association(WOEMA)Written CommentDated April 24, 2017Received April 27,2017Agree that some payers maymisinterpret the meaning of“Non-Preferred,” although theregulations are structured tomake it clear the drugs sodesignated are available totreat the injured worker whenauthorized through prospectivereview. The terminology willbe modified from“Preferred/Non-Preferred” to“Exempt/Non-Exempt.” Thisterminology will align moreclosely with the effect of thedesignation. Exempt meansexempt from prospectivereview, and “Non-Exempt”means the drug is not exemptfrom authorization throughprospective review.The terminology willbe modified from“Preferred/NonPreferred” to“Exempt/NonExempt.”or her health, including, but notlimited to, the potential loss of life,limb, or other major bodily functionor the normal prospective reviewtimeframe would be detrimental tothe injured worker’s life or healthor could jeopardize the injuredworker’s permanent ability toregain maximum enter is concerned that thedesignation of many medications as“Non-Preferred,” the meaning ofwhich could be misinterpreted bysome payers as “should be denied.”Many such “non-preferred” drugs areuseful and potentially critical in somesituations. The Division should makeit clear in these regulations that nonpreferred drugs are appropriate incertain instances and not automaticallydenied for use based upon thisdesignation.DWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesPage 9 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODNAME enter states that the proposeddefinition of Perioperative Fill fails todefine or identify the location of thedefinition for the specified criteria inthe rules. Commenter recommendsthat a clarifying citation to be added tomake the definition more clear.“ ‘Perioperative Fill’ means the policyset forth in section 9792.27.12allowing dispensing of identified NonPreferred drugs without prospectivereview where the drug is prescribedwithin the perioperative period andmeets specified criteria. , as defined insection 9792.27.12(b).”Ben RobertsDisagree. Not necessary andExecutive Viceappears duplicative.President and GeneralCounselPRIUMApril 29, 2017Written CommentNo action necessary.9792.27.1(s)Commenter recommends thefollowing revised language:Jeremy MerzAmerican InsuranceAssociationNo action necessary.“ ‘Perioperative Fill’ means the policyset forth in section 9792.27.12allowing dispensing of identified NonPreferred drugs without prospectivereview where the drug is prescribedwithin the perioperative period for asurgical procedure that has “010” or10 Day Post-operative Period or has“090”, or 90 Day Post-operativePeriod, listed for the reimbursableJason SchmelzerCalifornia Coalitionon Workers’CompensationDisagree. See response aboveto comment of CWCI datedMay 1, 2017, suggestingadding a definition of“surgery.”.May 1, 2017Written CommentDWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesPage 10 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIODNAME OFPERSON/AFFILIATIONRESPONSEACTIONRobert Blink, MDPresidentWesternOccupational &EnvironmentalMedical Association(WOEMA)Written CommentDated April 24, 2017Received April 27,2017Rupali Das, MD,MPH, FACOEMCalifornia MedicalDirectorRaymond Tan,PharmDDirector of PharmacyBenefitsZenith InsuranceWritten CommentApril 27, 2017Mitch SeamanLegislative AdvocateComment is not directed at theregulatory text.Nevertheless, DWC iscognizant of the need toexpeditiously recruit, select,and convene the P&TCommittee after adoption ofthe regulations.No action necessary.Comment is not directed at theregulatory text.Nevertheless, DWC iscognizant of the need toexpeditiously recruit, select,and convene the P&TCommittee after adoption ofthe regulations.No action necessary.Disagree with the suggestedmodification. SubstitutingNo action necessary.CPT code as found in the MedicareNational Physician Fee ScheduleRelative Value File incorporated intothe Official Medical Fee Scheduleand meets specified criteria.”9792.27.1(t)9792.27.16Commenter states that there will be aneed for further assessment andongoing updating of the drugformulary as time goes on. TheDivision should act swiftly to selectand appoint members of thiscommittee so that they are prepared tomeet ASAP after the implementationdate.9792.27.1(t)9792.27.16Commenter recommends acceleratedconstitution of the P&T Committee.9792.27.1(v)Commenter recommends the revisedlanguage that replaces the wordDWC MTUS DRUG FORMULARY REGULATIONS - 45 day Comments and ResponsesPage 11 of 136
MTUS DRUGFORMULARYRULEMAKING COMMENTS45 DAY COMMENT PERIOD“does” with “shall.”“Preferred drug” means a drug on theMTUS Drug List which is designatedas being a drug that does shall notrequire authorization thoughprospective review prior to dispensingthe drug .9792.27.1(y)Commenter recommends:“Special Fill” means the policy setforth in section 9792.27.11 allowingdispensing of identified Non-Preferreddrugs without prospective reviewwhere the drug is prescribed ordispensed at the single initialtreatment visit following a workplaceinjury, where the visit occurs within 7days of the date of injury. inaccordance with the criteria set forthin section 9792.27.11(b).9792.27.2Commenter recommends revisions:“(b) Except for continuing medicaltreatment subject to section 9792.27.3,subdivision (b), a drug dispensed on orafter January 1, 2018 July 1, 2017 foroutpatient use shall be subject to theMTUS Drug Formulary, regardless ofNAME OFPERSON/AFFILIATIONCalifornia LaborFederationWritten CommentMay 1, 2017Oral CommentRESPONSEACTION“shall not”, for “does not”,require authorization throughprospective review, would notmake a substantive differencein the meaning of the sentence.Ben RobertsAg
Zenith Insurance . Written Comment . April 27, 2017 . step therapy program be adopted in the initial formulary regulations, but is suggesting it be instituted after the P&T Committee is formed and can participate in consulting on the issue. Second, disagree with commenter’s suggestion that a step therapy align: Step 1 - Preferred, Step 2 - Non-