Transcription
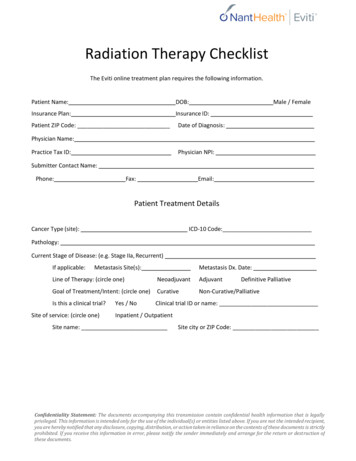
Hu et al. Journal of Hematology & 2018) 11:136REVIEWOpen AccessProton beam therapy for cancer in the eraof precision medicineMan Hu1,2,3, Liyang Jiang1,2,3, Xiangli Cui4, Jianguang Zhang5 and Jinming Yu1,2,3*AbstractPrecision radiotherapy, which accurately delivers the dose on a tumor and confers little or no irradiation to thesurrounding normal tissue and organs, results in maximum tumor control and decreases the toxicity to the utmostextent. Proton beam therapy (PBT) provides superior dose distributions and has a dosimetric advantage over photonbeam therapy. Initially, the clinical practice and study of proton beam therapy focused on ocular tumor, skullbase, paraspinal tumors (chondrosarcoma and chordoma), and unresectable sarcomas, which responded poorly whentreated with photon radiotherapy. Then, it is widely regarded as an ideal mode for reirradiation and pediatrics due toreducing unwanted side effects by lessening the dose to normal tissue. During the past decade, the application of PBThas been rapidly increasing worldwide and gradually expanding for the treatment of various malignancies. However, todate, the role of PBT in clinical settings is still controversial, and there are considerable challenges in its application. Wesystematically review the latest advances of PBT and the challenges for patient treatment in the era ofprecision medicine.BackgroundRadiotherapy (RT) is an established treatment modalityof malignant tumors. Currently, photon beam therapy isthe most widely used in clinical settings. Intensity-modulated photon radiotherapy (IMRT) was introduced inthe mid-1990s, and it took the radiotherapy with photons to a huge leap forward. As the development ofIMRT, it has been considered to be the advanced andthe standard of treatment for many malignancies [1]. Although the IMRT technique can typically provide amore conformal dose distribution than the traditionalRT mode, it is necessary to improve the tumor controland overall survival (OS), and reduce the RT toxicity. Itis well known that the advantage of a proton beam is thephysical characteristics of its depth-dose curve, with adose peak (Bragg peak) at a well-defined depth in tissue(Fig. 1). For relatively shallow tumors, unlike the photondepth-dose curve showing an exponentially decreasingenergy deposition with increasing depth in tissue, theBragg peak allows for rapid fall-off of the radiation doseat the end of the range and a sharp lateral dose fall-offwith the maximum energy deposition for each proton* Correspondence: sdyujinming@163.com1Shandong Cancer Hospital Affiliated to Shandong University, Jinan, China2Shandong Academy of Medical Sciences, Jinan, ChinaFull list of author information is available at the end of the articlebeam in the target region and almost no energy aroundit. Therefore, proton beam therapy (PBT) effectively allows the delivery of high-radiation doses to tumor cellsand very low or zero doses to the normal cells, which isrecognized as an ideal therapy modality for treatment ofmalignant diseases, especially for organs at risk (OARs)with less toxicity. As Dr. Herman Suit in the departmentof radiation oncology of Massachusetts General Hospital(MGH) said: “No advantage to any patient for any irradiation of any normal tissue exists; and radiation complication never occurs in nonirradiated tissues.”In 1946, Robert R. Wilson proposed to useaccelerator-produced beams of protons to treat patientswith deep-seated tumors [2]. In 1954, the first patientwith breast cancer was treated with proton radiation ofthe pituitary in the Berkeley Radiation Laboratory [3]. In1961, protons commenced to be used for clinical treatment at Harvard Cyclotron Laboratory [4]. Initially, theclinical practice and research of PBT only focused onthe tumors near a critical structure or those thatresponded poorly to photon radiotherapy such as oculartumors, skull base tumors, paraspinal tumors, and unresectable sarcomas. Over the next 60 years, with the vastdevelopment of technology, the application of PBT hasbeen gradually expanding to various neoplasms. Although increasingly more evidence has been indicated The Author(s). 2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, andreproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link tothe Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication o/1.0/) applies to the data made available in this article, unless otherwise stated.
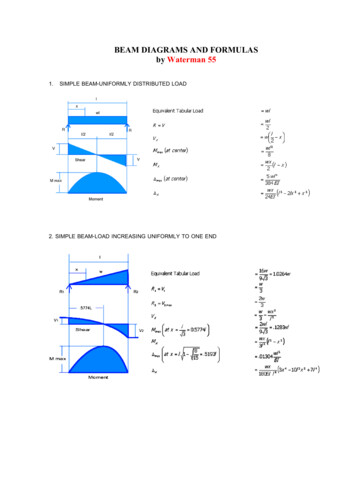
Hu et al. Journal of Hematology & Oncology(2018) 11:136Fig. 1 The diagram of dose distributions for photon (dashedyellow line), single proton beam (dashed green line) as a function ofpenetration depth in tumor (normalized to the maximum dose), andspread-out proton beam (solid blue line)for the advantages of PBT in clinical experience, PBT isnot good for all cases all of the time. It is very important to understand the benefits and limitations of protons as well as the biology and the behavior of thetumor. In this review, we summarized the latest advances and clinical applications of PBT. We also considered the challenges of treatment optimization in theera of precision medicine.Latest clinical studies of PBTThe dosimetry advantage of protons over photons hasalready been established (which is not reviewed in thearticle). However, do the potential advantages of the proton beam significantly transfer into clinical benefits forpatients? Can the advanced techniques such as 360 rotational gantries and intensity-modulated proton therapy(IMPT) further minimize toxicity and/or improve theclinical outcome? To date, there is not enough evidenceto answer these questions due to small cohorts of patients in most published studies and the limited prospective data of comparisons between proton andphoton radiotherapy. In this part, we present the clinicalexperiences and studies in the past few years, which maybe provide a valuable understanding of the true valueand advantage of PBT.ReirradiationReirradiation may provide the best chance of long-term disease control and even a potential cure for the patients whotruly undergo local and/or regional recurrence and whowould not develop distant metastasis. The physical characteristics of PBT are particularly suited for reirradiation,Page 2 of 16which has been reported in head and neck cancer (HNC),thoracic cancers and liver cancer.The largest report of recurrent HNC to date was ananalysis of 92 patients treated with a proton beam usingpassive scatter technique reirradiation by Romesser et al.[5]. The median doses were 60.6 Gy, and the 1 year cumulative incidence of locoregional failure (LRF), actuarial freedom of distant metastasis (FDM), and overallsurvival (OS) were 25.1%, 84.0%, and 65.2%, respectively.Eighty-seven (94.6%) patients completed the reirradiation course. Acute grade 3 toxicities of mucositis, dysphagia, esophagitis, and dermatitis accounted for 9.9%,9.1%, 9.1%, and 3.3%, respectively. Late grade 3 adverseevents included skin (8.7%) and dysphagia (7.1%), andonly two patients (2.2%) underwent grade 5 treatmentrelated bleeding toxicity. Phan et al. [6] evaluated 60HNC patients receiving proton beam reirradiation.Twenty-five percent patients (15/60) received passivescatter proton therapy (PSPT), and 75% (45/60) receivedIMRT. The 1 year rates of locoregional failure-free survival (LRFFS), progression-free survival (PFS), OS, anddistant metastasis-free survival (DMFS) were 68.4%,60.1%, 83.8%, and 74.9%, respectively. Acute grade 3 toxicity occurred in 30% patients (18), and 22% (13) neededa feeding tube. The 1-year rates of late grade 3 toxicityand feeding tube independence were 16.7% and 2.0%, respectively. Three patients may have died due toreirradiation-related toxicity. For patients with recurrentHNC, it is safe and effective to reirradiate disease byutilizing proton beam, which has acceptable rates ofcomplications and durable tumor control and survival.Because more patients with non-small cell lung cancer(NSCLC) have better survival, recurrence can occurmore often in the previously irradiated area or adjacentarea. Earlier published studies had explored the role ofproton beam reirradiation for recurrent NSCLC patients,and most were focused on the palliative intent withlower overall doses. Recently, with definitive intent,Chao et al. [7] have reported the safety/feasibility of PBTfor locally recurrent NSCLC (n 57) in a multi-centerprospective study. More than 90% of patients completedthe reirradiation course. With a median dose of 66.6 Gy,locoregional control (LRC) was 75%, with 1- and 2-yearOS rates of 59% and 43%, PFS of 58% and 38%, respectively. Twenty-four patients (42%) developed grade 3acute and/or late toxicities. Six patients experiencedgrade 5 toxicities. In the study, the proton plan waslargely double-scatter (n 34 [59.6%]) or uniform scanning (n 17 [29.8%]); only 10.6% were the IMPT technique, which spares the esophageal area and heart betterwith lower toxicity than PSPT. Ho et al. [8] have reported a retrospective analysis of 27 patients with reirradiation of thoracic malignancies using the IMPTtechnique delivery of a higher dose of radiation (median
Hu et al. Journal of Hematology & Oncology(2018) 11:136dose of 66 Gy). Twenty-two patients (81%) were treatedfor NSCLC. The satisfactory outcomes revealed that patients who received the dose 66 Gy had increased1-year freedom rates of local failure (LF) (100% vs 49%;P 0.013), LRF (84% vs 23%; P 0.035), and PFS (76% vs14%; P 0.050), while no grade 4 toxicities occurredand only 2 patients (7%) experienced late grade 3 pulmonary toxicity. These studies demonstrate that PBTcan provide benefits recurrent NSCLC patients, especially for metastatic lymph nodes in mediastinum, andallow more patients receiving a definitive concurrentchemoradiotherapy.The feasibility and efficacy of repeated PBT for intrahepatic recurrence or metastasis has been evaluated.Oshiro et al. [9] reported that among the 83 patientswith liver cancer who received definitive repeated PBT,the 5-year survival rate of the whole group is nearly50%, and no patient has radiation-induced liver disease.For reirradiation, it is critical to select the proper patientwith the tumor volume and location.Pediatric cancersWith more data from children treated with PBT, the proton beam model policy adopted by the American Societyof Radiation Oncology in 2017 supports PBT in childrenwith solid neoplasms, and it is now an option for manyChildren’s Oncology Group (COG) protocols [10]. Manystudies have confirmed the feasibility of PBT in pediatriccancer and achieved excellent outcomes compared tophoton therapy. The advantage of PBT is recognized forcraniospinal irradiation. A phase II clinical study reportedthe long-term results of PBT in 59 patients (aged 3–21years) with medulloblastoma [11]. Patients receivedchemotherapy and had a median craniospinal irradiationdose of 23.4 Gy (RBE) followed by a boost dose of 54 Gy(RBE). The 5-year cumulative incidence of severe hearingloss was 16%. There were no late toxicities of the heart,lungs, and digestive tract side effects, and no second primary tumor occurred, which was significantly better thanthat of photon therapy; the notable finding was that theintelligence quotient (IQ) of patients using PBT decreasedslower than that using photon therapy. The rates of PFSand OS at 5 years were 80% and 83%, respectively. Severalstudies reported that PBT has been used in the treatmentof retinoblastoma, which is a common pediatric intraocular tumor. Mouw et al. [12] reported long-term outcomesfor retinoblastoma with PBT. There were no patients diedof retinoblastoma or developed metastasis at a medianfollow-up of 8 years. Eleven of 60 irradiated tumors wereenucleated, mainly due to tumor progression. Twelve eyesdeveloped ocular complications requiring intervention,which mainly included cataract, radiation retinopathy,glaucoma, and neovascularization. Various other pediatriccancers including chordoma and chondrosarcoma [13],Page 3 of 16ependymoma [14], craniopharyngioma [15], low-grade glioma [16], atypical teratoid rhabdoid tumor [17], andEwing sarcoma [18] were treated with PBT, which is similar in adults, resulting in acceptable toxicities and showingsimilar survival outcomes to conventional radiotherapy.With the prolongation of the survival of pediatric cancers, the late response from radiotherapy has receivedincreasing attention. Growing evidence has demonstrated that PBT provide a health outcome benefit inpediatric patients, including radiation-associated lateendocrine dysfunction, cognitive ability, and quality oflife (QoL). Eaton et al. [19] compared the long-termclinical data in hormone levels after proton and photonirradiation. The results showed that PBT was associatedwith a reduced risk of hypothyroidism, sex hormone deficiency, and requirement for any endocrine replacementtherapy compared to photon therapy, but no significantdifference was found in the incidence of growth hormone deficiency, adrenal insufficiency, or precocious puberty. Pulsifer et al. [20] evaluated the cognitive functionafter PBT in 60 patients with pediatric CNS tumors including medulloblastoma, glioma, craniopharyngioma,ependymoma, and other brain tumors. During thefollow-up of 2.5 years, there was a significant decline inthe mean processing speed standard score, especially inyounger patients (age at baseline 12 years). The cognitive outcomes compare favorably to published results forpatients received photon RT. In a large prospectivestudy, Yock et al. [21] first showed the improvedlong-term health-related quality of life (HRQoL) outcomes of children with brain tumors treated with PBTcompared to photon RT. Leiser et al. [22] reported theQoL were encouraging in children with rhabdomyosarcoma who were treated with pencil-beam scattering(PBS). PBT appears to provide a low risk of second primary tumors, which is a very important problem forpediatric patients treated with RT. Children are in aperiod of growth and development, with high sensitiveness to radiation, and pediatric patients often have along-survival time. As mentioned above, in the phase IIclinical study [11], patients did not have an occurrenceof a second primary tumor during the 7-year follow-up,while a meta-analysis showed the 10-year second tumorand second malignant tumor incidence rates after photon therapy [23] were 6.1% and 3.7%, respectively. Sethiet al. [24] compared the risk of second malignancy in patients with retinoblastoma treated with photon therapyand PBT. At a median follow-up of 13.1 years in thephoton therapy group and 6.9 years in the PBT group,the cumulative incidence of second malignancies (radiation-induced or in-field) at 10 years was significantlyhigher in photon therapy group than that in PBT group(14% vs. 0%; P 0.015). An important challenge in children’s PBT is the anesthesia due to the need of precision
Hu et al. Journal of Hematology & Oncology(2018) 11:136therapy. To ensure the precision of repeatability duringtreatment, most children need anesthesia, which mayincrease the associated risks.Neurological tumorPBT offers an alternative modality of RT available forneurological tumors in adults, potentially better sparingthe surrounding normal brain tissue. Several prospectivestudies assessed the benefit of PBT in the managementof glioma or meningiomas for the patients with lowgrade disease, who are usually young with typically longsurvival with the disease. A proton treatment protocol(NCT01024907) by Maquilan et al. [25] first reportedthe acute toxicities in patients with low-grade gliomas(LGGs) or meningioma who received 54 Gy. Among the23 enrolled patients, only 1 patient suffered grade 3 fatigue during the treatment and the follow-up, and only 1patient had a grade 3 headache at on-treatment visitweek 3. There was no observed grade 3 acute toxicitiesin a multi-institution prospective study of 58 LGG patients who received PBT with 50.4 Gy to 54 Gy [26]. Astudy at MGH by Shih et al. [27] showed the findings of20 LGG patients with the delivered dose of 54 Gy usingPBT. The rates of PFS and OS at 5 years were 40% and84%, respectively. No grade 4 or 5 acute and late side effects occurred. All patients remained stable or slightlyimproved in neurocognitive status; 6 patients developedhormone deficiency, and there was no significant decrease in quality of life. The side effects of PBT are mildin clinical practice. McDonald et al. [28] reported the results of PBT in patients with World Health Organization(WHO) atypical meningiomas (grade 2). Twenty-two patients received a median dose of 63 Gy (RBE). With themedian follow-up of 39 months, the 5-year estimate of LCwas 71.1%, and it was 87.5% following a RT dose 60 Gy(RBE), compared to 50.0% for 60 Gy (RBE). The datashowed that PBT for meningiomas achieved favorabletumor control. For meningiomas that were partially adjacent to vital organs, PBT can be hypofractionated to bettercontrol the tumor, which has potential advantages.Vlachogiannis et al. [29] utilized IMPT (4 5 Gy or4 6.6 Gy) for treatment of intracranial meningioma(WHO I) in 170 patients, of which 155 were locatedin the skull base, and reported a 10-year PFS rate of 85%,with 6 patients with pituitary dysfunction, and 5 with signsof radiation necrosis (but only 1 requiring surgery, 5 withvisual impairment, and 1 with a tumor cyst). Tumors located in the anterior cranial fossa were significantly increasing the risk of complications.The preferred treatment of chordoma and chondrosarcoma is surgery. However, chordoma and chondrosarcoma, which originate in the skull base, are difficult tocompletely resect because the location is close to cranialnerves and blood vessels. To achieve a better local control,Page 4 of 16the radiation dose should be more than 74 Gy [30]. Thetreatment efficacy of photon therapy is unsatisfied due tothe dose limitation of structures surrounding the tumor,such as the brain stem, temporal lobe and optic nerve,and the radiation dose of the tumor cannot be radical byphoton therapy. However, PBT can increase the tumordose and can better protect normal tissues. PBT has beenused for the treatment of radio-resistant chordomas andchondrosarcomas for many decades. The patients withlow-grade chondrosarcoma usually have a better longterm survival than those with chordoma in PBT and caneven achieve a curable effect. Weber et al. [31] used PBSin 77 patients with skull-base chondrosarcoma. With amedian dose of 70 Gy, the actuarial LC and OS rates at 8years were 89.7% and 93.5%, respectively. Weber et al.have also reported long-term outcomes of skull-baselow-grade chondrosarcoma and chordoma patients (n 151) treated with PBS. The rates of 7-year LC were 70.9%and 93.6%, respectively, and the rates of 7-year OS were72.9% and 94.1%, respectively [32]. The toxicities of PBSfor chordoma and chondrosarcoma are mild, which include optic nerve injury, brain necrosis, spinal cord necrosis, and hearing loss. A recent meta-analysis compared theeffectiveness of PBT and photon therapy for chordoma[33]. The estimated 10-year OS rates of the PBT groupreached 60%, which was significantly higher than that ofconventional photon therapy (21%) and SRT (40%).Feuvret et al. [34] reported the results of 159 chondrosarcoma patients treated with either PBT alone orcombined with photon therapy. The median dose was70.2 Gy (RBE) and with a median follow-up of 77months, the LC and OS rates at 10 years were 93.5%and 87%, respectively. Sixteen patients died, 13 of intercurrent disease and 3 of disease progression. There wasno significant correlation between the incidence of toxicityand dose. Spinal cord necrosis is a serious side effect, anda study by Stieb et al. [35] has shown that dose constraintsof 64 Gy as a dose to relative volume of 2% (D2%) for thesurface spinal cord and 54 Gy for the center spinal cordseemed safe and appropriate for clinical use. Protons havebeen used in the treatment of functional pituitary adenomas [36], but the data are very limited to date.HNCPBT has been as an option when normal tissue constraintscannot be met by photon-based therapy for tumors of theethmoid sinus, maxillary sinus, salivary gland, periorbital,nasopharynx, and mucosal melanoma, from the updated2017 National Comprehensive Cancer Network (NCCN)guidelines. PBT is uniquely suited for HNC with the complex anatomy of tumors and important sensitive OARs,such as brain stem, optic chiasm, and optic nerve. The radiation targets of some HNC, including major salivarygland cancer, skin cancer, early-stage tonsil cancer, and
Hu et al. Journal of Hematology & Oncology(2018) 11:136select oral cavity cancer, can be confined to unilateral headand neck, and therefore, lend themselves to the treatmentof PSPT, which is better suited to superficial tumors whichinvade or abut critical structures. Romesser et al. [37]compared the treatment-related toxicities between patients receiving PSPT and IMRT in 41 patients with oneside of major salivary gland tumors or cutaneous squamous cell cancers. The results showed that the rates ofgrade 2 acute dysgeusia, mucositis, and nausea were significantly lower in PSPT group than those in IMRT group(5.6% vs. 65.2%, 16.7% vs. 52.2%,11.1% vs. 56.5%; P 0.001, 0.019, 0.003, respectively). Russo et al. [38] have reported that 54 patients with stage III and IV SCC of thenasal cavity and paranasal sinus received PBT. The median dose was 72.8 Gy (RBE). At 5 years, the PBT yieldedgood actuarial LC rate of 80%, and the OS rate of 47%.Wound adverse events constituted the most common severe toxicity. Fifteen grade 3 side effects were observed.No grade 5 toxicity occurred. A meta-analysis study fornasal cavity and paranasal sinus tumors has showed a5-year locoregional benefit and a slight OS advantage withPBT when compared to IMRT [39]. Decreased acute toxicities such as dysgeusia, mucositis, and nausea occurredin the PSPT group. However, the PSPT group had a higherincidence of grade 2 dermatitis. Excellent LRC and survival rates were acquired on patients with nasopharyngealcarcinoma (NPC) using PBT. In a phase II trial, Chan etal. [40] assessed the efficacy and side effects of 23 patientswith stage III–IVB NPC received concurrent chemo-PBT.With a median follow-up of 28 months, there were nolocal or regional recurrence occurred, and the 2-yeardisease-free survival (DFS) and OS were 90% and 100%,respectively. There was no acute or late grade 4 or 5treatment-related toxicities. A three-dimensional (3D)technique, PSPT with two posterior oblique fields, wasused in the study. For treatment of regions in the nasopharynx or oropharynx with the bilateral neck, PSPTseemed to have difficulty achieving high-dose conformality, whereas IMPT has clear dosimetric advantages, providing the ability to cover a large field and deliver theconformity dose to complex head and neck tumors withirregular shapes. Lewis et al. [41] presented the clinical results for 10 patients treated with IMPT. No patientsunderwent any acute grade 4 toxicities or any chronicgrade 3 toxicities. With the median follow-up of 24.5months, 2-year rates of LRC, DMFS, and OS were 100%,88.9%, and 88.9%, respectively. In a retrospective casecontrol study [42], IMPT-treated NPC patients (n 10) had significantly lower rates of gastrostomy tubeinsertion compared to IMRT-treated patients (n 20)(20% vs. 65%, P 0.02). There was no significant difference in chronic grade 3 toxicity, body weight lost,and swallowing dysfunction between type of radiation(P 0.542, 0.333, and 0.175, respectively). No patientPage 5 of 16developed LF in the IMPT group and 1 did in theIMRT group. One patient in each IMPT and IMRTgroup developed distant metastatic disease. Additionally, one patient in each group died. A series of studies on patients with (OPC) using IMPT were reportedat MD Anderson Cancer Center. Sio et al. [43] retrospectively collected data from a prospective study anddiscovered that IMPT led to a lower symptom burdenduring the first 3 months after treatment for OPC patients who treated with IMPT and concurrent chemotherapy. In the same prospective study, Gunn et al.reported the clinical outcome of 50 patients withOPC received IMPT. The encouraging results showedthe 2-year OS and PFS of 94.5% and 88.6%, respectively, without grade 3 acute and late toxicities found[44]. Then, the outcomes of the same cohort from2011 to 2014 and 100 IMRT OPC patients from 2010to 2012 were compared [45]. With a medianfollow-up of 32 months, the significant differenceswere not found in OS, PFS, acute grade 3 dermatitisor mucositis between the two groups. The results ofthe abovementioned comparative studies of IMRT andIMPT in NPC and OPC may be biased due to thecase-matched analysis. Additionally, the samples weresmall in the single-institution case, and the follow-upwas relatively short for NPC or OPC patient with favorable OS.Eye tumorsAlthough the incidence of eye tumors is very low, thereis a relatively longstanding experience for plenty of patients with eye tumors treated with PBT, yielding excellent survival outcomes with ocular conservation andvisual preservation. Lane et al. [46] showed the findingsof PBT in 3088 patients with uveal melanoma. With themedian follow-up of 12.3 years, the melanoma-relatedmortality rate was 24.6% in 15 years after treatment and26.4% in 25 years. The highest annual rates of deathfrom melanoma were reported 3 to 6 years after PBT,with the death rates of approximately 3–4%. A study of982 patients with uveal melanoma treated with PBTshowed that the 10-year LC and overall eye retentionrates were 96.4% and 95%, respectively, with a medianfollow-up of 60.7 months [47]. The toxicities were acceptable, where 115 (12.1%) patients developed glaucoma and 30 patients had to be enucleated. In aretrospective study that enrolled 336 patients with largechoroidal melanomas, the rates of visual acuity retentionat 10 years were 8.7% for 20/200 and 22.4% for at leastcounting fingers; neovascular glaucoma was found in25.3% patients. The rates of eye retained and tumor controlled were 70.4% and 87.5%, respectively, at 10 yearspost-PBI therapy. The 10-year rates of all-cause mortality and dying of metastatic uveal melanoma were 60.7%
Hu et al. Journal of Hematology & Oncology(2018) 11:136and 48.5%, respectively [48]. Verma et al. [49] reviewedthe results of 14 studies of PBT for uveal melanoma,which was consistent with prior studies. In a retrospective study with 492 choroidal melanomas patients receiving PBT [50], the 5-year LC was high at 94%, and thesurvival was not deteriorative. The mean baseline visualacuity, visual acuity 20/200, neovascular glaucoma, andenucleation were in 31.7% (20/63), 20%, 27%, and 19.5%,respectively. The study indicated that PBT was a safestrategy for large choroidal melanomas. Similarly, inorder to achieve good vision function and cosmesis, PBTis an attractive RT mode for patients with periorbital tumors. At MD Anderson Cancer Center, 20 patients withlacrimal gland (n 7), lacrimal sac/nasolacrimal duct (n 10), and eyelid (n 3) underwent orbit-sparing surgeryfollowed by PBT [51]. With a median follow-up of 27.1months, no patient had local recurrence, only 1 sufferedregional recurrence and another 1 distant metastasis.There were no patients who experienced acute grade 3ocular disorders, acute and chronic grade 4 toxicity.Meanwhile, the good local control has been obtained[52]. Among 11 patients who experienced orbit-sparingsurgical resection followed by PBT and/or chemotherapy, 10 patients had post-treatment visual acuities betterthan 20/40 and were also satisfied with their cosmesis after eye-sparing surgery. PBT achieved good LCand was well tolerated with a good vision functionand cosmesis.The eye toxicities were acceptable for patientstreated with PBT. Thariat et al. [53] showed the 5-yearincidence of dry-eye syndrome and severe (grade 2–3)dry-eye syndrome was 23.0% and 10.9%, respectively.Patients whose tumors located on the superotemporalor temporal lobe had a higher risk for severe dry-eyesyndrome.The lens is one of the most radiosensitive organs andcan cause cataracts when exposed. PBT can better spareall or part of the lens than other forms of RT. The5-year incidence of cataract was 18.7%, and the corresponding vision-impairing cataract rate was 12.8% of1696 ocular melanomas by PBT [54]. For tumors whichare located on the upper side of the choroid plexus, ifthe upper eyelid margin is not retracted out of the radiation field, patients abrade the cornea every time theyare blinking. This may cause keratopathy, and it can become so severe as to cause corneal enucleation. However, transpalpebral (i.e., through closed eyelids) PBT ofchoroidal melanoma can spare the eyelid and avoid ocular surface complications without increasing failure oflocal control [55].NSCLCThe toxicity of cardiopulmonary, lung, and spinal cordrestricts the ascent of dose for patients with NSCLC byPage 6 of 16RT with or without chemotherapy. PBT’s early use inNSCLC was confined to small (stage I) tumors with conventional fraction, producing a high rate of LC. For stageI NSCLC, it is interesting in stereotactic body protonradiotherapy (SBPT). Loma Linda University reportedclinical experiences in the early-stage NSCLC (n 111)with SBPT [56]. With the dose escalated from 51 Gy to70 Gy in 10 fractions, the OS was improved, with a4-year OS rate of 18% up to 51% (P 0.006). Chang etal. [57] have reported a modified less hypofractionatedregimen of PBT with a total dose of 87.5 Gy and 2.5 Gype
Proton beam therapy for cancer in the era of precision medicine Man Hu1,2,3, Liyang Jiang1,2,3, . results in maximum tumor control and decreases the toxicity to the utmost extent. Proton beam therapy (PBT) provides superior dose distributions and has a dosimetric advantage over photon beam therapy. Initially, the clinical practice and .