Transcription
Perspectives onManaging PatientResponsibilitySurvey of Independent Medical Practicesand Billing Companiesinboxhealth.com
Table of Contents3Introduction Patient Responsibility Rises Rising Patient Consumerism andIncreased Adoption of Digital Technology What Does This Mean for Medical Practicesand Billing Companies?5 Surveyof Medical Practicesand Billing Companies Survey Goals Respondent Demographics Survey Results10Conclusionsinboxhealth.com // Perspectives on Patient Responsibility2
IntroductionToday’s era of healthcareis defined by rising patientresponsibility. This trend is acatalyst for increased patientconsumerism and medicaldebt. Several important factorsare propelling patients to takeon an increased burden ofmedical costs.This report explores the underlying factors fueling this trendand the associated need for more advanced and efficient billingprocesses to optimally manage patient responsibility.This report also presents results from an online survey1conducted with independent medical practices and medicalbilling companies to gain deeper insight into these topics.Key Highlights from Survey:Over 50% of medical practices have had apatient leave their practice because of aperceived billing issue. fter collecting patient balances, bothApractices and billing companies saidmanaging phone calls is their primarypatient responsibility challenge.Both practices and billing companies saidbetter patient communication channels isthe #1 factor that would help improve patientcollections. In the next 12 months, 48% ofpractices would like to offer text support.Over two-thirds of billing companies wouldlike to offer mobile payments within thenext 12 months.Executive SummaryThis survey was conducted to better understand the uniquechallenges practices and billing companies face aspatient responsibility rises in healthcare.The goals were to compare how practices and billingcompanies currently approach patient accounts receivableand how they see their methods changing in the future.The data consists of 140 respondents who participatedvia an online survey. Most notably, over half of practices saidrising patient payments/responsibility is their primary businesschallenge, and less than half are satisfied with the way patientresponsibility is currently managed. Billing companies andpractices agree that managing patient phone calls is one of thetop operational challenges, and better communication channelsare imperative to improve administration of collections.Billing companies, in particular, view mobile payments asa key solution streamlined operations.inboxhealth.com // Perspectives on Patient Responsibility ess than half of practices are satisfiedLwith the way patient responsibility iscurrently managed.Patient Responsibility RisesA large driver of the growth in patient responsibility is therise in enrollment in high-deductible health plans (HDHPs).HDHPs, created to provide an option for consumers to obtainhealth insurance at a lower premium, are defined by the IRS asany plan with a deductible of at least 1,400 for an individualor 2,800 for a family.2 Fifty-one percent of the workforcenationwide was enrolled in a HDHP in 2019.33
Regardless of whether a deductible applies, a large share ofcovered workers also pay a portion of the cost when theyvisit an in-network physician. Most covered workers havea copayment when they visit a doctor, and some also havecoinsurance requirements. The average copayments in 2020were 26 for primary care and 42 for specialty care.The average coinsurance rates were 18% for primary careand 19% for specialty care.4Moreover, individuals without insurance bear the full bruntof their medical expenses. In the first half of 2020, 12.5%of U.S. adults ages 19-64 were uninsured and 43.4% wereinadequately insured.5The rise of patient responsibility corresponds with the rise ofmedical debt. In June 2020, an estimated 17.8% of individualshad medical debt,6 and just over one-third of consumers saidthey have had an unpaid medical bill go to collections.7Unexpected medical bills are similarly ubiquitous. More thanhalf of respondents to a 2020 survey said they have receivedan unexpected medical bill, meaning that they assumed aservice was covered by insurance and it ultimately was not, orthe amount they expected to pay out of pocket was differentfrom the bill they received.8 Furthermore, 48% have been lateon a medical bill payment, owing in large part to confusion overthe bill and who owes what,9 highlighting the need for bettercommunication about patient responsibility.Rising Patient Consumerism andIncreased Adoption of DigitalTechnologyWith rising patient consumerism – patients acting asconsumers with a choice in their healthcare options and strivingto make the best decisions for quality and cost – comes ashift in patient experience expectations. Paralleling this risingconsumerism of healthcare is a rapidly increasing adoption ofdigital technology. According to a 2019 survey:10 4 9% of healthcare consumers said they are frustratedabout their provider’s lack of adoption of digitaladministrative processes, such as online bill pay, accessto insurance information, digital pre-appointment forms,or mobile and email bill delivery. 4 1% of patients said they would stop going to theirhealthcare provider over a poor digital experience.One in five patients already stopped or switched providersover a poor digital experience.Furthermore, the COVID-19 pandemic has acceleratedadoption and expectations for digital offerings. During theinboxhealth.com // Perspectives on Patient Responsibilitypandemic, consumers shifted rapidly and dramatically to onlinechannels,11 with technology and digital capabilities standing outas key factors of business success during the crisis.12 Notably,44% of older adults (50 ) have a more positive attitude towardtechnology now than they did prior to the pandemic.13What Does This Mean for MedicalPractices and Billing Companies?With these aforementioned factors as the backdrop, medicalpractices and billing companies must effectively and efficientlymanage their patient accounts receivable to sustain thebusiness. Furthermore, for practices, a poor patient experiencecan result in negative reviews and subsequent loss of businessand associated revenue. For billing companies, a negativepatient experience can result in loss of clients andstunted growth.Over half of the medical practicesparticipating in the survey had a patientleave their practice because of aperceived billing issue.Patient billing is a vital task, but it places an enormousadministrative burden on practices and billing companies.A study of 27 health system administrators and 34 physiciansin 2016 and 2017 showed the estimated costs of billing andinsurance-related activities ranged from 20 for a primary carevisit to 215 for an inpatient surgical procedure, representing3% to 25% of professional revenue.14Survey respondents spend an average of15 minutes on each patient statement.“ Phone calls with billing questions take upa significant amount of time, regardless[of how] carefully we review patientstatements prior to sending for clarityand accuracy.”- Billing Company Operations Leader4
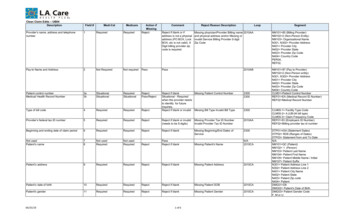
Survey of Medical Practicesand Billing CompaniesSurvey GoalsThe goals of the online survey conducted with independentmedical practices and medical billing companies were to: I dentify trends, challenges, and key factors important toeach constituent regarding collecting patient responsibility B etter understand how patient collections arecurrently managedSurvey ResultsThis section provides an in-depth look at key findings fromthe survey.Rising patient responsibility is in the topthree business challenges for practices.Primary Business Challengesof Medical PracticesResponses P rovide insight into preferences for payment andbill delivery methods69%Insurance reimbursement challenges70 C ompare responses from medical practices with billingcompanies to identify potential opportunities65%Paperwork/administrative tasks6657%Rising patient payments/responsibility5825%Improving patient experience2517%Shift toward value-based care1717%Other17Respondent roles were as follows:12%Reputation management/competition12 Physician: 48%10%Price transparency10Respondent DemographicsMedical PracticesA total of approximately 90 independent medical practicesthroughout the country are represented in the survey results. Practice Manager/Administrator/Front Office: 25% Medical Biller/Billing Manager: 11%Total Respondents:101 Other roles: 16%Practices ranged in size from 1 to 100 or more providers,with an average of 16 providers across a variety ofclinical specialties.Billing CompaniesA total of approximately 50 billing companies throughout thecountry are represented in the survey results.Respondent roles were as follows:Collecting patient balances is atop challenge of managing patientresponsibility for both practicesand billing companies.The survey showed the top three patient responsibilitychallenges for practices to be: Owner/CEO/President: 56%1Collecting patient balances Operations Leader: 21%2Managing patient phone calls (tie) Billing Manager: 11%3Collecting copayments at the time of service (tie) Other roles: 12%Billing companies served anywhere from 1 to over 100practices, with an average of 37 practices across a varietyof clinical specialties.inboxhealth.com // Perspectives on Patient ResponsibilityThe top three patient responsibility challengesfor billing companies were cited as:1Collecting patient balances2Managing patient phone calls3Cost of collecting from patients5
Primary Patient Responsibility Challenges for Practices and Billing CompaniesResponsesPracticesResponsesBilling Companies57%Collecting patient balances5877%Collecting patient balances4439%Collecting copayments at the time of service3958%Managing patient phone calls3339%Managing patient phone calls3951%Cost of collecting from patients2931%Cost of collecting from patients3144%Reviewing statements for accuracy2530%Front desk/billing team communication3040%Front desk/billing team communication2328%Reviewing statements for accuracy2833%Posting/processing patient payments1920%Patient payment experience2030%Patient payment experience1719%Posting/processing patient payments1928%Collecting copayments at the time of service1618%Reporting on patient collections performance1825%Reporting on patient collections performance1412%Other125%Other3Total Respondents:101Total Respondents:57Overall satisfaction with the way patient reponsibility ismanaged is relatively low: 56% of practices and 49% ofbilling companies are less than satisfied.Satisfaction with Managing Patient ling Companies2%11%Extremely Satisfied (10)33%15%Extremely Satisfied (8)18%33%Satisfied (29)9%Neutral (33)Neutral (17)Dissatisfied (13)37%Total Respondents:inboxhealth.com // Perspectives on Patient ResponsibilitySatisfied (15)Dissatisfied (4)Extremely Dissatisfied (4)(89)38%Total Respondents:Extremely Dissatisfied (1)(45)6
Both practices and billing companies would like to see anincrease in all digital payment methods, including credit card,ACH, mobile payment, and portal and a decrease in paymentsvia cash and check.Notably, while only 33% of billing companies currently offermobile payments, 69% would like to offer mobile paymentsin the next 12 months.Preferences for billing methodstrending toward digital.Payment Method Preferences: What Practices and Billing Companies Currently OfferPractices(80)(43)90% 96%CheckBilling Companies(75)(33)(56)(32)(50)84%73%63%71%56% 58%38% 47%20% 33%Point ofServiceTerminalPortalMobilePaymentsCashCredit Cardon 1)(1)18%33%4%11%1%2%ACHOtherBitcoinPayment Method Preferences: What Practices and Billing Companies Would Like to Offer in the Next 12 MonthsPractices(59)(55)(23)(59)66% 64%62%51%66% 69%54% 47%43% 49%43% 69%Credit Cardon FilePoint th.com // Perspectives on Patient (31)Billing %ACHOtherBitcoin7
Practices would like to see an increase in digital support optionsand a reduction in phone calls.The survey showed that only 36% of billing companiesresponding to the survey currently offer text/SMS patientbilling support.Practices want fewer phone calls andmore text-based billing support.Practice Preferences for Billing Support OptionsCurrently offeredResponsesWould like to offer within 12 ther64%Other41%IVR13%IVR3Total Respondents:89Total Respondents:89Support Options Currently Offered by Billing CompaniesCurrently 11%Chat57%IVR37%Other3Total Respondents:inboxhealth.com // Perspectives on Patient Responsibility458
Better communication cited as topmeans to improve collecting patientresponsibility.Respondents from medical practices and billing companies alikecited better patient communication channels as one of thebest ways to improve collecting patient responsibility.Features to Improve Collecting Patient ResponsibilityResponsesPracticesBilling CompaniesResponses43%A better patient portal3849%Better patient comm. channels (email, text, IVR)2243%Better patient comm. channels (email, text, IVR)3847%Automated patient billing2139%Improved analytics and reporting3547%Automated patient payment posting2136%Personalized patient statements3242%A better patient portal1935%Automated patient billing3136%More patient payment options1634%Automated patient payment posting3031%Improved analytics and reporting1429%More patient payment options2624%Personalized patient statements1113%Other124%OtherTotal Respondents:89Total Respondents:Billing companies share their thoughtson the benefits achieved from using aspecialized billing software solution:“ Major increase of patient payments. Patientsdid not have a way to pay online previouslyand now they just click and pay. Also, they canask a quick question via text or email and get aresponse from Inbox Health team. Saves me lotsof questions and time. Love the convenience ofclicking a button to send out a paper statement.”245“Automation, online payments, [fewer] phone calls.”“Saving time by not printing, folding,stuffing envelopes, [and adding] postage.”“ Reducing the inbound phone calls hasallowed my team to focus on their dailyduties without constant interruption.”“ Velocity of capital, less human error, fewer touch points in the process.”inboxhealth.com // Perspectives on Patient Responsibility9
Inbox Health Users StandOut in the Survey“ Inbox Health has truly been agame-changer.”Although representing a small portion of the overallsurvey respondents, responses from billing companiesthat use Inbox Health’s specialized billing softwareconsistently had a more positive perspective on manyof the topics covered in the survey.- Medical Billing Company Owner A n overwhelming majority of respondents usingInbox Health say they are satisfied with the waypatient responsibility is managed.“ Love using Inbox Health forpatient payments.” I nbox Health users also indicated that usingthe platform has:- Medical Biller/Account Manager educed the level of effort required toRmanage patient collections treamlined sending of patient statementsS(greater utilization of text) Improved patient collectionsSources1Online survey conducted September – October 2021 via Survey Monkey .Improved performance reporting2 Reduced inbound patient calls3 Improved overall patient experienceU.S. Centers for Medicare & Medicaid Services (CMS), Healthcare.gov, High Deductible HealthPlan (HDHP), retrieved from e-health-plan/.51% of U.S. Workforce Enrolled in High-Deductible Health Plans, Which May Leave SomeUnderinsured, Value Penguin, Jul 27, 2021, retrieved from -high-definition-health-insurance-plans.2020 Employer Health Benefits Survey, 2020 Annual Survey, Kaiser Family Foundation, Oct08, 2020, retrieved from ry-of-findings/.4 The Commonwealth Fund, U.S. Health Insurance Coverage in 2020: A Looming Crisis inAffordability, Survey Brief August 2020, retrieved from es/2020-08/Collins looming crisis affordability biennial 2020 sb.pdf.5 Kluender R, Mahoney N, Wong F, Yin W. Medical Debt in the US, 2009-2020. JAMA.2021;326(3):250–256. doi:10.1001/jama.2021.8694, retrieved from ract/2782187.6 ConclusionsThe survey results reveal a resounding need for more efficientand technically advanced methods of managing patientresponsibility, undoubtedly spurred by the recent pandemic thatacted as a catalyst for broader technology adoption. Further,there is a growing emphasis on the patient financial journey,as patients are demanding new ways to communicate, engage,and interact with their doctors and their medical bills at thesame time as copayments, coinsurance, and rising deductiblesdrive patient responsibility increasingly higher.For billing companies, more efficient and effective billing andpayment options can improve overall productivity and drivepatient satisfaction for their client organizations while removingbarriers to communication regarding payment, which can inturn result in less time spent on the phone and greater paymentrates. It is inevitable that the medical billers who thrive will bethose who implement patient-focused strategies that maximizecollections through patient-friendly payment mechanisms.inboxhealth.com // Perspectives on Patient ResponsibilityKey trends among healthcare consumers in 2019, October 10, 2019, Health Exec,retrieved from ends-among-healthcareconsumers-2019.7 Consumer Attitudes Toward Medical Bills The Price Transparency Rule, Waystar, 2020,retrieved from cy-Survey.html?utmsource linkedin&utm campaign 20210202 consumer price transparency survey&utmmedium social&utm content ad01.8 9Ibid.60% of younger patients will switch healthcare providers over a poor digital experience:survey, Fierce Healthcare, Oct 10, 2019, retrieved from or-digital-experiencesurvey.10 How COVID-19 has pushed companies over the technology tipping point—and transformedbusiness forever, McKinsey & Company, Oct 5, 2020, retrieved from oint-and-transformed-business-forever.11 12Ibid.Personal Tech and the Pandemic: Older Adults Are Upgrading for a Better OnlineExperience, 2021 Tech Trends and the 50 : Top 10 Biggest Trends, AARP Research, April2021, retrieved from -CMP RDRCT-PRI-TECH-040721/?cmp RDRCT907b618d-20210416.13 Tseng P, Kaplan RS, Richman BD, Shah MA, Schulman KA. Administrative Costs AssociatedWith Physician Billing and Insurance-Related Activities at an Academic Health Care System.JAMA. 2018;319(7):691-697. doi:10.1001/jama.2017.19148, retrieved from 85/.14 10
About Inbox HealthInbox Health is changing the way people think about patientbilling. The company’s patient billing communication platformhelps medical billing teams streamline patient engagement andsupport while creating exceptional consumer experiences.Using Inbox Health’s data-driven platform, billers easilyautomate and personalize patient communication, providingconsumers increased clarity and confidence around chargesand more convenient payment options which dramaticallyimproves profitability, collection rates and speed to payment.This survey was conducted by Inbox Health.Data was collected from September to October 2021.Learn more at inboxhealth.comInbox Health is a registered trademark of Inbox Health, Inc.
inbohealthco Perspecties on Patient esponsiility 6 19% Posting/processing patient payments 19 18% Reporting on patient collections performance 18 Practices Responses Total Respondents: 101 20% Patient payment experience 20 12% Other 12 28% Reviewing statements for accuracy 28 31% Cost of collecting from patients 31 30% Front desk/billing team communication30 .