Transcription
MINI SUMMIT II:EPISODE-BASED COSTMEASURE DEVELOPMENTFOR THE QUALITYPAYMENT PROGRAMOctober 12, 2017Theodore Long, MD, MHSSenior Medical OfficerQuality Measurement and ValueBased IncentivesGroup (QMVIG)Center for Clinical Standards andQuality (CCSQ)
DisclaimersThis presentation was prepared as a tool to assist providers and is not intendedto grant rights or impose obligations. Although every reasonable effort has beenmade to assure the accuracy of the information within these pages, the ultimateresponsibility for the correct submission of claims and response to anyremittance advice lies with the provider of services.This publication is a general summary that explains certain aspects of theMedicare Program, but is not a legal document. The official Medicare Programprovisions are contained in the relevant laws, regulations, and rulings.Medicare policy changes frequently, and links to the source documents havebeen provided within the document for your referenceThe Centers for Medicare & Medicaid Services (CMS) employees, agents, andstaff make no representation, warranty, or guarantee that this compilation ofMedicare information is error-free and will bear no responsibility or liability forthe results or consequences of the use of this guide.2
INTRODUCTION TOTHE MERIT-BASEDINCENTIVE PAYMENTSYSTEM (MIPS)MIPS3
How MIPS Relates to Legacy ProgramsA visualization of how the legacy programs streamline into the MIPSperformance categories:Participating in Is similar to PQRSQualityVM*CostEHRAdvancing Care Information*Also includes elements of the PQRS quality data4
MIPS Performance CategoryCost No reporting requirement; 0% of Final Score in 2017 Clinicians assessed on Medicare claims data CMS will still provide feedback on how you performed in this category in2017, but it will not affect your 2019 payments. Keep in mind:Uses measures previously used in thePhysician Value-Based Modifier programor reported in the Quality and ResourceUse Report (QRUR)Only the scoring is different5
WHAT IS A COSTMEASURE?Five Essential Componentsof Cost Measures6
What is a Cost Measure?Represents the Medicare payments for the medical care furnished to a patientduring an episode of care. There are 5 components:12345Defining anepisode groupAssigningcosts to theepisode groupAttributingepisodegroups tocliniciansRisk adjustingepisodegroupsAligning costwith quality7
1Component 1:Defining an Episode Group An episode group focuses on clinical conditions requiring treatment (the condition itselfor procedures to treat the condition)-Example: a procedural episode group that is surgical in nature could include: pre-operative services, surgicalprocedure, anesthesia, follow-up care, services related to complications, readmissions An episode is a specific instance of an episode group for a given patient and clinician-Example: A clinician might be attributed 20 episodes (instances of the episode group) from the episode groupfor heart failure in a year Can vary in scope (e.g., narrow and precise or broad and general)-Example: An episode group for cataract removal with insertion of intraocular lens prosthesis has a narrowscope. In comparison, an episode group for gastrointestinal hemorrhage has a broad scope. Can be divided into sub-groups to define more homogeneous patient cohorts-Example: Gastrointestinal hemorrhage may be divided into sub-groups for upper and lower gastrointestinalhemorrhage Three types of episode groups in December posting:1Acute InpatientMedical Condition2ChronicCondition3Procedural8
2Component 2:Assigning Costs to the Episode Group Assignment of items and services determines what is included in episodecosts and depends on role of attributed clinician Episode window determines the period of time during which claims areeligible to be assigned to the episodeItems and Services that Are Assignedto the Episode GroupDirect ServicesProvided by the attributedclinicianItems and Services thatAre Not Assigned to theEpisode GroupIndirect ServicesUnrelated ServicesProvided or ordered byother clinicians in the sameclinical context Post-acute care Ancillary care Consequencesof care (e.g.,complications)Unrelated to the clinicalmanagement of the patient’scondition or procedure that isthe focus of the episodegroup9
2Elements of an Episode of Carefor a Given Patient and ClinicianTrigger ServiceService Assigned to EpisodeService Not Assigned to sEpisode Window10
3Component 3:Attributing Episode Groups to Clinicians Attribution is the assignment of responsibility for an episode of care to aprincipal (or managing) clinician Attribution should be transparent to clinicians and only hold them responsiblefor outcomes they can reasonably be expected to influence Patient relationship categories and codes being developed under MACRAcan be used in conjunction with claims-based rules for attributionDevelopment Timeline for Patient Relationship Categories and Codes2016AprilPostedfor publiccomment2016DecemberRevisedPostingfor publiccomment2017OperationalListApril11
4Component 4:Risk Adjusting Episode Groups Adjusts for factors outside the clinician’s control that can influence cost- Age, comorbidities, illness stage/severity, other aspects of patient’s clinical history Aims to avoid penalizing clinicians who treat unhealthy or complex patients Selection of risk adjustment method informed by analyses, technical expertpanels, clinical committees, and public comment12
5Component 5:Aligning Cost with Quality Alignment with indicators of quality is necessary to compensate forinformation not adequately captured by episode costs Quality assessments might include:- Complications, rehospitalizations, unplanned care and other consequences- Outcomes of care- Overuse, underuse, misuse- Processes of care- Functional status of patient- Patient experience13
BACKGROUNDON EXISTINGEPISODE-BASEDCOST MEASURES14
CMS Has Previously Developed Two Setsof Episode-Based Cost Measures Method A measures created using Brandeis’ Episode Grouper for Medicare(EGM) Method B measures created to complement the Method A measures by usingnew approach and analyzing distinct episode groups Reporting of Method A & B episode-based cost measures in theSupplemental Quality and Resource Use Reports (QRURs) began in 2011- Method A & B measures reported in 2012, 2014, and 2015 Supplemental QRURs- Only Method A measures reported in 201115
PRIOR STAKEHOLDERFEEDBACK AND THE ROLEOF CLINICIAN FEEDBACKIN DEVELOPING COSTMEASURES16
Stakeholder Input Gathered to DatePostings Related to Existing CMSEpisode Groups (Method A and B) CMS Episode Groups Posting(October 2015) Supplemental CMS EpisodeGroups Posting (April 2016)Technical Expert Panel (TEP) Serves a high-level advisory roleand provides guidance on overalldirection of measure development Includes representatives fromspecialty societies, academia,healthcare administration, andpatient advocacy organizations Meetings in August 2016,December 2016, March 2017, andAugust 2017Posting Related to CostMeasure Development December 2016 posting of costmeasure development paper anddraft list of episode groups andtrigger codes Public comment period closedApril 24, 2017 Listening Session on April 5, 2017to solicit feedback on the costmeasure development processClinical Committee (CC) Makes recommendations aboutclinical specifications for episodegroups Initial input activities occurred inAugust-September 2016 70 clinical experts from 50 professional societies Provided expert input to developdraft list of episode groups andtrigger codesRulemaking 2017 Quality Payment ProgramProposed Rule (May 2016) 2017 Quality Payment ProgramFinal Rule with Comment Period(November 2016) 2018 Quality Payment ProgramProposed Rule for Year 2 (June2017)Clinical Subcommittees (CS) Builds upon the feedback receivedthrough the first CC in AugustSeptember 2016 The 7 CS that began work in May2017 represent the first of multiplewaves of 18 CS being convenedfor this project Includes 145 clinical experts fromover 95 professional societies Provide clinical input to build outprocedural and acute inpatientmedical condition episode groups17
Key Points from Stakeholder Feedback Defining episode groups and cost measures must yield actionable informationthat can guide improvements to patient care Attribution of claims and episodes to clinicians should be clear and credible atthe time of service and should consider patient relationship Assignment of costs to episode groups should only hold cliniciansaccountable for patient outcomes that are within the scope implied by theirclinical role Cost measures should account for patient complexity through appropriate riskadjustment Cost measures must be aligned with quality measures to promote delivery ofhigh-quality and efficient care Broad stakeholder feedback is crucial to the development and implementationprocess, and more input will be solicited, including targeted stakeholder input thataccomplishes the following:-Include adequate preparation materials and time, achieve greater transparency, notduplicate efforts among different activities, and incorporate feedback loops acrossSubcommittees18
Cost Measure Development Approach DirectlyIncorporates Stakeholder Input on Every Component1.Defining an episode group: TEP #1 and #3: Provided guidance on essential concepts for defining an episode group and how toprioritize episode groups for development Clinical Committee #1: Identified conditions/procedures for episode groups, selected trigger codes Clinical Subcommittees (Wave 1): Reviewed and refined draft list of episode groups and triggercodes2.Attributing to clinicians: TEP #2: Provided feedback on potential rules for attributing episode groups to clinicians Clinical Subcommittees (Wave 1): Recommended rules to assign clinician responsibility for episodes3.Assigning costs: TEP #2: Provided input on approaches for assigning costs to episode groups Clinical Subcommittees (Wave 1): Selected which claims are counted in episode costs4.Risk adjusting: TEP #4: Provided feedback on potential risk adjustment approaches Clinical Subcommittees (Wave 1): Identified relevant patient characteristics for use in statisticalmodels5.Aligning with quality: TEP #1 and #3: Provided feedback on approaches for aligning of cost and quality Clinical Subcommittees (Wave 1): Considered potential for aligning cost with quality when selectingepisode groups to develop and providing input on triggers19
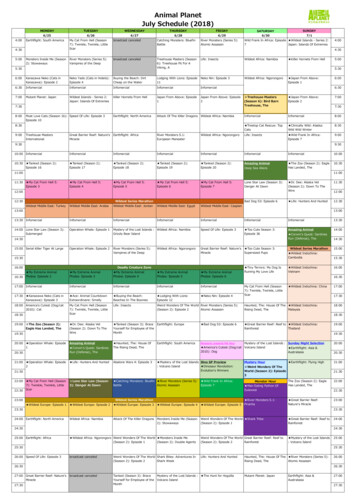
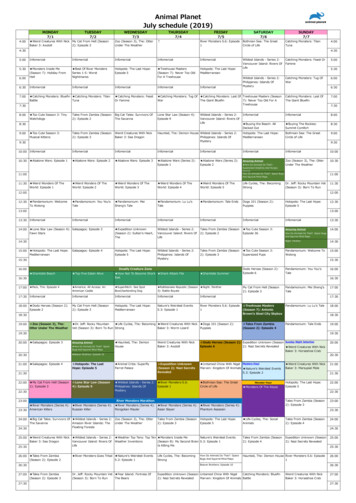
Dec. 2016 Acute Condition and ProceduralEpisode Groups Mapped to 18 Clinical AreasNo.Clinical AreaTotal # of Proceduraland Acute EpisodeGroups# of ProceduralEpisode Groups# Acute InpatientMedical ConditionEpisode Groups1Musculoskeletal Disease Management — Non-Spine222112Cardiovascular Disease Management181263Gastrointestinal Disease Management — Medical and Surgical11564Pulmonary Disease Management110115Oncologic Disease Management — Medical and Surgical7706Neuropsychiatric Disease Management6067Peripheral Vascular Disease Management5508Urologic Disease Management5509Renal Disease Management40410Head and Neck Disease Management22011Infectious Disease Management20212Musculoskeletal Disease Management — Spine22013Dermatologic Disease Management11014Endocrine Disease Management10115Hematologic Disease Management10116Opthalmologic Disease Management11017Pain Management11018Rheumatologic Disease Management10120
Clinical Subcommittees Will Develop One orMore Episode Groups Within Their Clinical Areas Goal is to involve a full range of clinicians to develop the episode groupspertinent to a given clinical area (in order of priority selected bysubcommittee itself) For example, the Cardiovascular Disease Management Subcommitteemay include the following types of clinicians: Cardiology Vascular Surgery Family Medicine Cardiac Electrophysiology Critical Care (Intensivist) Physician Assistant Cardiac Surgery Intensive CardiacRehabilitation Nurse Practitioner Interventional Cardiology Diagnostic Radiology Thoracic Surgery Anesthesiology Emergency Medicine Geriatric Medicine Internal Medicine Certified Registered NurseAnesthetist Licensed Clinical SocialWorker Clinical Nurse Specialist21
Example: MIPS – New Cost MeasureDevelopment for Orthopaedic Surgeons New Cost Measure: Knee Arthroplasty Clinical Committee Composed of Orthopaedic Surgeons Affiliated with:-American Academy of Orthopaedic Surgeons-American Orthopaedic Association-American Orthopaedic Foot and Ankle Society-American Association of Hip and Knee Surgeons-American Orthopaedic Society for Sports Medicine-American Shoulder and Elbow Surgeons-Arthroscopy Association of North America22
List of New Cost Measures Routine Cataract Removal with Intraocular Lens (IOL) Implantation Screening/Surveillance Colonoscopy Knee Arthroplasty ST-Elevation Myocardial Infarction (STEMI) with Percutaneous CoronaryIntervention (PCI) Revascularization for Lower Extremity Chronic Limb Ischemia Elective Outpatient Percutaneous Coronary Intervention (PCI) Intracranial Hemorrhage or Cerebral Infarction Simple Pneumonia with Hospitalization23
FIELD TESTING24
Overview of Field Testing Field testing is the process of collecting broad-based public commentsbefore consideration of the eight episode-based cost measures’ for potentialuse in the Quality Payment Program Feedback will be taken into consideration for measure refinement and futuremeasure development activities. Field testing will take place from October 16 to November 15, 2017 Feedback is sought on: Draft measure specificationsField test reportsSupplemental documentation25
Online Feedback Survey Stakeholders will be able to provide feedback through an online survey To make it easy for all stakeholders to provide feedback, the survey willconsist of:-Multiple choice/select answersFree text responsesAn option to skip all questions and attach a comment in PDF or Word format This survey will open on October 16 and close at midnight on November measures-field-testing26
WHAT SUPPORTIS AVAILABLE?27
Technical Assistance for CliniciansCMS has free resources and organizations on the ground to provide help toclinicians who are participating in the Quality Payment Program:28
The Quality Payment Program Service Centeris also available to help:qpp.cms.govCMS has organizations on the ground to provide help to clinicianswho are eligible for the Quality Payment Program:TCPITransforming Clinical Practice Initiative (TCPI): TCPI is designed to support more than 140,000 clinicianpractices over the next 4 years in sharing, adapting, and further developing their comprehensive qualityimprovement strategies. Clinicians participating in TCPI will have the advantage of learning about MIPSand how to move toward participating in Advanced APMs. Click here to find help in your area.QIN-QIOsQuality Innovation Network (QIN)-Quality Improvement Organizations (QIOs): The QIO Program’s14 QIN-QIOs bring Medicare beneficiaries, providers, and communities together in data-driven initiativesthat increase patient safety, make communities healthier, better coordinate post-hospital care, andimprove clinical quality. More information about QIN-QIOs can be found here.APMLearningSystemsIf you’re in an APM: The Innovation Center’s Learning Systems can help you find specialized informationabout what you need to do to be successful in the Advanced APM track. If you’re in an APM that is not anAdvanced APM, then the Learning Systems can help you understand the special benefits you havethrough your APM that will help you be successful in MIPS. More information about the Learning Systemsis available through your model’s support inbox.29
30
Measure Development December 2016 posting of cost measure development paper and draft list of episode groups and trigger codes Public comment period closed April 24, 2017 Listening Session on April 5, 2017 to solicit feedback on the cost measure development process Rulemaking 2017 Quality Payment Program Proposed Rule (May 2016)