Transcription
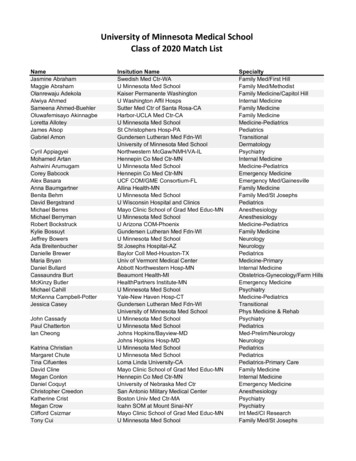
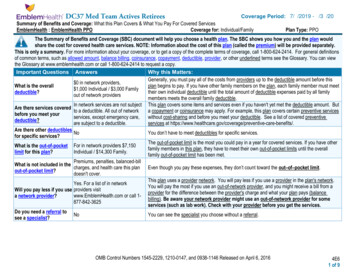
DC37 Med Team Actives RetireesCoverage Period: 7/1/2019 - 6/30/2020Summary of Benefits and Coverage: What this Plan Covers & What You Pay For Covered ServicesCoverage for: Individual/FamilyEmblemHealth : EmblemHealth PPOPlan Type: PPOThe Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the plan wouldshare the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be provided separately.This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, call 1-800-624-2414. For general definitionsof common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider, or other underlined terms see the Glossary. You can viewthe Glossary at www.emblemhealth.com or call 1-800-624-2414 to request a copy.Important Questions AnswersWhy this Matters:Generally, you must pay all of the costs from providers up to the deductible amount before this 0 in network providers,plan begins to pay. If you have other family members on the plan, each family member must meetWhat is the overall 1,000 Individual / 3,000 Familytheir own individual deductible until the total amount of deductible expenses paid by all familydeductible?out of network providersmembers meets the overall family deductible.In network services are not subject This plan covers some items and services even if you haven't yet met the deductible amount. ButAre there services coveredto a deductible. All out of networka copayment or coinsurance may apply. For example, this plan covers certain preventive servicesbefore you meet yourservices, except emergency care,without cost-sharing and before you meet your deductible. See a list of covered preventivedeductible?are subject to a deductible.services at e-benefits/.Are there other deductiblesNoYou don’t have to meet deductibles for specific services.for specific services?The out-of-pocket limit is the most you could pay in a year for covered services. If you have otherWhat is the out-of-pocket For in network providers 7,150family members in this plan, they have to meet their own out-of-pocket limits until the overallIndividual / 14,300 Family.limit for this plan?family out-of-pocket limit has been met.Premiums, penalties, balanced-billWhat is not included in thecharges, and health care this plan Even though you pay these expenses, they don’t count toward the out–of–pocket limit.out-of-pocket limit?doesn't cover.This plan uses a provider network. You will pay less if you use a provider in the plan's network.Yes. For a list of in networkYou will pay the most if you use an out-of-network provider, and you might receive a bill from aWill you pay less if you use providers visitprovider for the difference between the provider's charge and what your plan pays (balancewww.EmblemHealth.com or call 1a network provider?billing). Be aware your network provider might use an out-of-network provider for some877-842-3625services (such as lab work). Check with your provider before you get the services.Do you need a referral toNoYou can see the specialist you choose without a referral.see a specialist?OMB Control Numbers 1545-2229, 1210-0147, and 0938-1146 Released on April 6, 20164E61 of 9
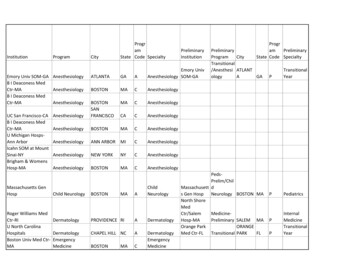
All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.CommonMedical EventIf you visit a healthcare provider’s officeor clinicIf you have a testWhat You Will PayServices You May NeedNetwork ProviderOut-of-Network Provider(You will pay the least)(You will pay the most)Primary care visit to treat 25 Adult visit / 0 DependentAfter deductible is met, 30%an injury or illnesschild visitcoinsurance 25 Adult visit / 0 DependentAfter deductible is met, 30%Specialist visitchild visitcoinsurancePreventiveAfter deductible is met, 30%care/screening/No chargecoinsuranceimmunizationDiagnostic test (x-ray,blood work) 25 Adult visit / 0 Dependentchild visitAfter deductible is met, 30%coinsuranceImaging (CT/PET scans,MRIs)Generic drugs (Tier 1)Preferred brand drugs(Tier 2)Non-preferred branddrugs (Tier 3) 25 Adult visit / 0 Dependentchild visitNot coveredAfter deductible is met, 30%coinsuranceNot coveredNot coveredNot coveredNot coveredNot coveredNot coveredNot covered 50 co-pay/visitsAfter deductible is met, 30%coinsuranceIf you need drugs totreat your illness orconditionMore information aboutprescription drugcoverage is available atwww.EmblemHealth.com. Specialty drugsFacility fee (e.g.,ambulatory surgeryIf you have outpatientcenter)surgeryPhysician/surgeon feesIf you need immediatemedical attentionEmergency room careEmergency medicaltransportationUrgent careNo Charge 150 co-payNot Available 25 Adult visit / 0 Dependentchild visitAfter deductible is met, 30%coinsurance 150 co-payCovered at 100% of Usualand Customary ChargeAfter deductible is met, 30%coinsurance*Limitations, Exceptions, & OtherImportant Radiology services, e.g. X-ray, are coveredunder the Imaging benefit and Imaging costshare applies. Radiology services require precertification.Pre-certification requiredPre-certification required-----None----Applies to facility charge, waived if admitted.-----None---------None-----* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.4E62 of 9
CommonMedical EventIf you have a hospitalstayIf you have mentalhealth, behavioralhealth, or substanceabuse needsIf you are pregnantServices You May NeedFacility fee (e.g., hospital 0 co-pay per admissionroom)Physician/surgeon feeNo chargeOutpatient services 25 Adult visit / 0 Dependentchild visitInpatient services 0 co-pay per admissionOffice visitsNo chargeChildbirth/deliveryNo chargeprofessional servicesChildbirth/delivery facility 0 co-pay per admissionservicesHome health careRehabilitation servicesIf you need helprecovering or haveother special healthneedsWhat You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least)(You will pay the most)Habilitation servicesSkilled nursing careNo chargeAfter deductible is met, 30%coinsuranceAfter deductible is met, 30%coinsuranceAfter deductible is met, 30%coinsuranceAfter deductible is met, 30%coinsuranceAfter deductible is met, 30%coinsuranceAfter deductible is met, 30%coinsuranceAfter deductible is met, 30%coinsuranceAfter deductible is met, 30%coinsuranceInpatient: 0 co-pay per admissionAfter deductible is met, 30%Outpatient: 25 Adult visit / 0coinsuranceDependent child visitInpatient: 0 co-pay per admissionAfter deductible is met, 30%Outpatient: 25 Adult visit / 0coinsuranceDependent child visitAfter deductible is met, 30% 0 co-pay per confinementcoinsuranceDurable medicalequipmentNo chargeNot coveredHospice servicesNo chargeNot covered7/9/2019- 12/31/2019*Limitations, Exceptions,& OtherImportant InformationPre-certification required-----None----Up to 20 family visits for substance abuseservicesPre-certification required-----None---------None---------None----200 visits per calendar year. Pre-certificationrequired.Inpatient: 30 days per calendar year.Outpatient: 30 visits per calendar year forPhysical Therapy and 10 visits per calendaryear for Speech Therapy.60 days per calendar year. Pre-certificationrequired.Pre-certification required when amount isgreater than 2,000210 days per lifetime. Pre-certificationrequired.* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.4E63 of 9
CommonMedical EventIf your child needsdental or eye careServices You May NeedWhat You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least)(You will pay the most)7/9/2019- 12/31/2019*Limitations, Exceptions,& OtherImportant InformationChildren’s eye exam 0 co-payNot coveredOne eye exam covered every 12 monthsthrough participating EyeMed/ CPS providersChildren’s glasses 130 frame allowance. Standardsingle, bifocal or trifocal lenses: 0Not coveredco-pay. Contact lenses availablein lieu of eyeglassesAvailable through participating EyeMed/ CPSproviders: Frames covered every 12 months,lenses covered every 12 monthsChildren’s dental checkupNot coveredNot covered* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.4E64 of 9
Excluded Services & Other Covered Services:Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Hearing aids Acupuncture Long-term care Private-duty nursing Cosmetic surgery Most coverage provided outside the United States. Routine foot care Dental careSee www.emblemhealth.com Weight loss programs Non-emergency care when traveling outside the U.S.Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Bariatric surgery Infertility treatment Routine eye care Chiropractic careYour Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for thoseagencies is: New York State Department of Financial Services at 1-800-342-3736 or www.dfs.ny.gov/, U.S. Department of Health and Human Services at1-877-267-2323 x1565 or www.cciio.cms.gov, U.S. Department of Labor, Employee Benefits Security Administration at 1-866-444-3272 html or www.dol.gov/ebsa/healthreform. Other options may be available to you too, including buying individualor SHOP insurance coverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call1-800-318-2596 or NY State of Health Marketplace at 1-855-355-5777 or www.nystateofhealth.ny.gov.Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called agrievance or appeal. For more information about your right, look at the explanation of benefits you will receive for that medical claim. Your plan documents alsoprovide complete information to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, or assistance,contact:EmblemHealthBy Phone:Please call the number on your ID card.In writing:EmblemHealthGrievance and Appeals DepartmentP.O. Box 2801New York, NY 10116-2807Website: www.emblemhealth.comFor All Coverage TypesNew York State Department of Financial ServicesBy Phone: 1-800-342-3736In writing:New York State Department of Financial ServicesConsumer Assistance UnitOne Commerce PlazaAlbany, NY 12257Website: www.dfs.ny.gov* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.4E65 of 9
For HMO CoverageNew York State Department of HealthBy Phone: 1-800-206-8125In writing:New York State Department of HealthOffice of Health Insurance ProgramsBureau of Consumer Services – Complaint UnitCorning Tower – OCP Room 1607Albany, NY 12237Email: managedcarecomplaint@health.ny.govWebsite: www.health.ny.govConsumer Assistance ProgramNew York State Consumer Assistance ProgramBy Phone: 1-888-614-5400In writing:Community Health Advocates633 Third Avenue, 10th FloorNew York, NY 10017Email: cha@cssny.orgWebsite: www.communityhealthadvocates.orgFor Group Coverage:U.S. Department of LaborEmployee Benefits Security Administration at 1-866-444-EBSA (3272)Website: www.dol.gov/ebsa/healthreformDoes this plan provide Minimum Essential Coverage? YesIf you don’t have Minimum Essential Coverage for a month, you’ll have to make a payment when you file your tax return unless you qualify for an exemption from therequirement that you have health coverage for that month.Does this plan meet the Minimum Value Standards? YesIf your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace.Language Access Services:Navajo (Dine): Dinek'ehgo shika at'ohwol ninisingo, kwiijigo holne' ––––––––To see examples of how this plan might cover costs for a sample medical situation, see the next –––––––* For more information about limitations and exceptions, see the plan or policy document at www.emblemhealth.com/sbc.4E66 of 9
This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will bedifferent depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost sharingamounts (deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion ofcosts you might pay under different health plans. Please note these coverage examples are based on self-only coverage.Peg is having a babyManaging Joe’s type 2 diabetesMia’s Simple Fracture9 months of in-network pre-natal care and ahospital delivery)(a year of routine in-network care of a wellcontrolled condition)(in-network emergency room visit and follow upcare)n The plan’s overall deductiblen Specialist (cost sharing)n Hospital (facility) cost sharingn Other cost sharingn The plan’s overall deductiblen Specialist (cost sharing)n Hospital (facility) cost sharingn Other cost sharing 0 25 0 96This EXAMPLE event includes services like:Specialist office visits (prenatal care)Childbirth/Delivery Professional ServicesChildbirth/Delivery Facility Services Diagnostictests (ultrasounds and blood work) Specialistvisit (anesthesia) 12,800Total Example CostIn the example, Peg would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn’t coveredLimits or exclusionsThe total Peg would pay is 0 500 0 96 596 0 25 0 4,313This EXAMPLE event includes serviceslike: Primary care physician office visits(including disease education)Diagnostic tests (blood work)Prescription drugsDurable medical equipment (glucose meter)Total Example CostIn the example, Joe would pay:Cost SharingDeductiblesCopaymentsCoinsuranceWhat isn’t coveredLimits or exclusionsThe total Joe would pay isn The plan’s overall deductiblen Specialist (cost sharing)n Hospital (facility) cost sharingn Other cost sharing 0 25 150 162This EXAMPLE event includes services like:Emergency room care (including medicalsupplies)Diagnostic test (x-ray)Durable medical equipment (crutches)Rehabilitation services (physical therapy) 7,400 0 820 0 4,313 5,133Total Example CostIn the example, Mia would pay:Cost SharingDeductiblesCopaymentsCo-insuranceWhat isn’t coveredLimits or exclusionsThe total Mia would pay isThe plan would be responsible for the other costs of these EXAMPLE covered services. 1,900 0 763 0 162 9254E67 of 9
GETTING HELP IN A LANGUAGEOTHER THAN ENGLISHATTENTION: This is an important document. If you need help to understand it, please call the telephone numbermarked “customer service” on the back of your member ID card [TTY/TDD: 711]. We can give you an interpreterfor free in the language you speak.Español (Spanish)ATENCIÓN: Este es un documento importante. Si necesita ayuda para entenderlo, llame al número telefónicomarcado “customer service” que se encuentra en el dorso de su tarjeta de identiicación de miembro [TTY/TDD:711]. Le podemos proporcionar un intérprete que habla su idioma sin ningún costo.中文 (Traditional �員卡背面標記為“customer 人員。Pусский (Russian)ВНИМАНИЕ! Это важный документ. Если у Вас возникли трудности с пониманием этого документа и Вамнеобходима помощь, позвоните по телефону отдела обслуживания клиентов (customer service), указанномуна обратной стороне Вашей идентификационной карточки [служба текстового телефона (TTY/TDD): 711]. Мыможем бесплатно предоставить Вам переводчика, который говорит на Вашем языке.Kreyòl Ayisyen (Haitian Creole)ATANSYON: Sa a se yon dokiman ki enpòtan. Si ou bezwen èd pou konprann li, tanpri rele nimewo ki make “customerservice” nan do kat ID manm ou [TTY/TDD: 711]. Nou kapab ba ou yon entèprèt gratis nan lang ou pale a.한국어 (Korean)주의: 이것은 중요한 문서입니다. 이 문서를 이해하는 데 도움이 필요하시면 회원ID 카드의 뒷면에“customerservice” 라고 표시된 전화번호[TTY/TDD: 711]로 연락해 주십시오. 저희는 귀하가 사용하는 언어에 대해 무료통역사를 제공할 수 있습니다.Italiano (Italian)ATTENZIONE. Questo è un documento importante. Per qualsiasi chiarimento telefoni all “customer service” alnumero stampato sul retro della Sua tessera (per i non udenti: 711). Possiamo mettere a disposizione gratis uninterprete nella Sua lingua. ( אידיש Yiddish)(Yiddish) שידיא גערופן נומבער טעלעפון ם דע רופט ביטע , פארשטיין צו עס הילף דארפט איר אויב . דאקומענט וויכטיגע א איז דאס customer” ביטע רופט דעם טעלעפון נומבער גערופן , אויב איר דארפט הילף עס צו פארשטיין . איז א וויכטיגע דאקומענט דאס : מעלדונג : מעלדונג שפראך וואס איר די אין פריי איבערזעצער אן געבן אייך קענען מיר .[TTY/TDD:711] קארטל אייער אויף “customer. מיר קענען אייך געבן אן איבערזעצער פריי אין די שפראך וואס איר רעדט .[TTY/TDD: 711] אויף אייער קארטל service”“service. רעדט বাাংলা �ি আকর্ষণ করছি: এটি একটি গুরুত্বপূর্ণ নথি। এটি বুঝতে আপনার যদি সাহায্যের প্রয়োজন হয়, তাহলে অনুগ্রহ করে আপনার মেম্বার আইডি �িঠেআক্ষ“customerণ করটি: এিservice”একি ুুবপূণষ নটি।নম্এিবুঝতে আপনারাজনকথাহ বলেন, োহতলঅনুরজন্হ যকতরচিহ্নিত টেলিফোনবরে [TTY/TDD:711] যটদকল করুসাহাতেরন। আপনি ��িনামূআপনারল্যে �ন কাতিদোভাষীদিতে পারি। “customer service” টিটিে মেটলত ান নবতর [TTY/TDD: 711] কল কুন। আপটন ময ভা্া কিামেবারষ র ��ারPolski(Polish)জয টবনােূতে আেরা আপনাতক একজন মদাভা্ী টদতে পাটর।UWAGA: To jest ważny dokument. Jeżeli potrzebujesz pomocy w celu zrozumienia jego treści, zadzwoń do„customer service” pod numer telefonu podany na odwrocie karty identyikacyjnej ubezpieczonego (member IDcard) [TTY/TDD: 711]. Możemy bezpłatnie zapewnić usługi tłumacza języka, którym się posługujesz.(ARABIC) ةيبرعلا هابتنا : ةمهم ةقيثو هذه . اهاوتحم مهفل ةدعاسم ىلإ ةجاحب تنك اذإ ، « ـب هيلإ راشملا مقرلاب لاصتالا ىجرٌي customer service” ىلع [ كتيوضع ةقاطب رهظ TTY/TDD:711]. ًاناجم اهثدحتت يتلا ةغللاب كل يروف مجرتم ريفوت اننكمُي .Group Health Incorporated (GHI), HIP Health Plan of New York (HIP), HIP Insurance Company of New York and EmblemHealth Services Company, LLC areEmblemHealth companies. EmblemHealth Services Company, LLC provides administrative services to the EmblemHealth companies.10-8812 8/16
Français (French)ATTENTION : ce document est important. Si vous avez besoin d’aide pour en comprendre le contenu, veuillezcomposer le numéro «customer service » au dos de votre carte de membre [Sourds et malentendants : 711].Nous pouvons mettre gratuitement à votre disposition un interprète dans votre langue.(Urdu) ودرا ںید ہجوت : « مرک ہارب وت ےہ ترورض یک ددم ےیل ےک ےنھجمس ےسا وک پآ رگا ۔ےہزیواتسد مہا کیا ہی customer service» یئاو یٹ یٹ[ ےہ جرد رپ تشپ یک ڈراک یڈ یئآ ربمم ےک پآ وج ںیرک لاک رپ ربمن ےلاو / یڈ یڈ یٹ : 711] نابز وج پآ ۔ ۔ںیہ ےتکسرک مہارف مجرتم تفم وک پآ مہ ںیم سا ںیہ ےتلوب Tagalog (Tagalog)NANAWAGAN NG PANSIN: Ito ay isang mahalagang dokumento. Kung kailangan mo ng tulong para maintindihanito, pakitawagan ang numero ng telepono na minarkahang “customer service” sa likod ng inyong ID card ngmiyembro [TTY/TDD: 711]. Maaari ka naming bigyan ng libreng interpreter sa wikang iyong sinasalita.Ελληνικά (Greek)ΠΡΟΣΟΧΗ: Αυτό το έγγραφο είναι σημαντικό. Εάν χρειάζεστε βοήθεια για να το κατανοήσετε, καλέστε μας στοναριθμό που σημειώνεται ως «customer service» στο πίσω μέρος της κάρτας της συνδρομής σας [αριθμός για άτομα μεπροβλήματα ακοής (ΤΤΥ/TDD): 711]. Μπορούμε να σας προσφέρουμε δωρεάν διερμηνεία στη μητρική σας γλώσσα.Shqip (Albanian)VINI RE: Ky është një dokument i rëndësishëm. Nëse ju nevojitet ndihmë për ta kuptuar, ju lutemi telefononi nënumrin ku shkruhet “customer service”, i cili gjendet ne anen e pasme të kartës tuaj identiikuese të anëtarësisë[Shërbimi rele TTY/TDD: 711]. Ne mund t’ju ofrojmë pa pagesë një përkthyes në gjuhën që lisni ju.NOTICE OF NONDISCRIMINATION POLICYEmblemHealth complies with applicable Federal civil rights laws and does not discriminate on the basis of race,color, national origin, age, disability, or sex. EmblemHealth does not exclude people or treat them differentlybecause of race, color, national origin, age, disability, or sex.EmblemHealth: Provides free aids and services to people with disabilities to communicate effectively with us, such as:– Qualiied sign language interpreters– Written information in other formats (large print, audio, accessible electronic formats, other formats) Provides free language services to people whose primary language is not English, such as:– Qualiied interpreters– Information written in other languagesIf you need these services, please call the telephone number marked “customer service” on the back of yourmember ID card. TTY/TDD: 711.If you believe that EmblemHealth has failed to provide these services or discriminated in another way on the basisof race, color, national origin, age, disability, or sex, you can ile a grievance with EmblemHealth Grievance andAppeals Department, PO Box 2844, New York, NY 10116, or call the telephone number marked “customer service”on the back of your member ID card. (Dial 711 for TTY/TDD services.) You can ile a grievance in person, by mailor by phone. If you need help iling a grievance, EmblemHealth’s Grievance and Appeals Department is available tohelp you. You can also ile a civil rights complaint with the U.S. Department of Health and Human Services, Oficeof Civil Rights electronically through the Ofice of Civil Rights Complaint Portal, available at ocrportal.hhs.gov/ocr/portal/lobby.jsf or by mail or phone at U.S. Department of Health and Human Services, 200 IndependenceAvenue SW, Room 509F, HHH Building, Washington, DC 20201; 1-800-368-1019, (dial 1-800-537-7697 for TTYservices).Complaint forms are available at hhs.gov/ocr/ofice/ile/index.html.
through participating EyeMed/ CPS providers Children's glasses 130 frame allowance. Standard single, bifocal or trifocal lenses: 0 co-pay. Contact lenses available in lieu of eyeglasses Not covered Available through participating EyeMed/ CPS providers: Frames covered every 12 months, lenses covered every 12 months Children's dental check-up