Transcription
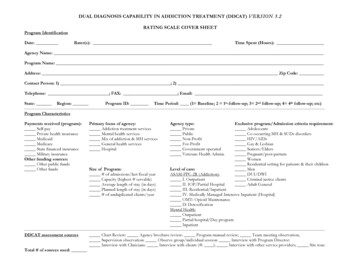
DUAL DIAGNOSIS CAPABILITY IN ADDICTION TREATMENT (DDCAT) V ER S IO N 3.2RATING SCALE COVER SHEETProgram IdentificationDate:Rater(s):Time Spent (Hours):Agency Name:Program Name:Address: Zip Code:Contact Person: 1) ; 2)Telephone: ; FAX: ; Email:State: Region:Program ID: Time Period: (1 Baseline; 2 1st-follow-up; 3 2nd follow-up; 4 4th follow-up; -----------------Program CharacteristicsPayments received (program):Self-payPrivate health insuranceMedicaidMedicareState financed insuranceMilitary insuranceOther funding sources:Other public fundsOther fundsPrimary focus of agency:Addiction treatment servicesMental health servicesMix of addiction & MH servicesGeneral health servicesHospitalSize of Program:# of admissions/last fiscal yearCapacity (highest # servable)Average length of stay (in days)Planned length of stay (in days)# of unduplicated clients/yearAgency type:PrivatePublicNon-ProfitFor-ProfitGovernment operatedVeterans Health Admin.Exclusive program/Admission criteria requirement:AdolescentsCo-occurring MH & SUDs disordersHIV/AIDsGay & dential setting for patients & their childrenMenDUI/DWICriminal justice clientsAdult GeneralLevel of care:ASAM-PPC-2R (Addiction):I. OutpatientII. IOP/Partial HospitalIII. Residential/InpatientIV. Medically Managed Intensive Inpatient (Hospital)OMT: Opioid MaintenanceD: DetoxificationMental Health:OutpatientPartial hospital/Day -----------------------------DDCAT assessment sourcesChart Review: Agency brochure review: Program manual review; Team meeting observation;Supervision observation: Observe group/individual session: Interview with Program Director:Interview with Clinicians: Interview with clients (#: ); Interview with other service providers; Site tour.Total # of sources used:
DUAL DIAGNOSIS CAPABILITY IN ADDICTION TREATMENT PROGRAMS (DDCAT) V ER SION 3.2RATING SCALE1AOSI. PROGRAMSTRUCTUREIA. Primary focus ofagency as stated in themission statement(If program has mission,consider programmission)IB. Organizationalcertification & licensure.2Addiction Only3DDC5DDEPrimary focus isaddiction, co-occurringdisorders are treatedPrimary focus onpersons with cooccurring disorders.Is certified and/orlicensed to provide bothPermits only addictiontreatmentHas no actual barrier, butstaff report there to becertification or licensurebarriers.Has no barrier toproviding mental healthtreatment or treating cooccurring disorderswithin the context ofaddiction treatmentIC. Coordination andcollaboration withmental health services.No document of formalcoordination orcollaboration.Meets the SAMHSAdefinition of minimalCoordination.Vague, undocumented,or informal relationshipwith MH agencies, orconsulting with a staffmember from thatagency.Meets the SAMHSAdefinition ofConsultation.Formalized anddocumentedcoordination orcollaboration withmental health agency.Meets the SAMHSAdefinition ofCollaboration.ID. Financial incentives.Can only bill foraddiction treatments orfor persons withsubstance use disorders.Could bill for eitherservice type if substanceuse disorder is primary,but staff report there tobe barriers. –OR- Partialreimbursement for MHservices availableCan bill for either servicetype, however, substanceuse disorder must beprimary.2314Formalized coordination& collaboration, and theavailability of casemanagement staff, orstaff exchange programs(variably used)Meets the SAMHSAdefinition ofCollaboration and hassome informalcomponents consistentwith Integration.Most services areintegrated within theexisting program, orroutine use of casemanagement staff orstaff exchange programs.Meets the SAMHSAdefinition of Integration.Can bill for addiction ormental health treatments,or the combinationand/or integration.452
3AOSII. PROGRAMMILIEUIIA. Routine expectationof and welcome totreatment for bothdisordersIIB. Display anddistribution of literatureand patient educationalmaterials.DDCDDEExpects substance usedisorders only, refer ordeflect persons withmental health disordersor symptoms.Documented to expectsubstance use disordersonly (e.g. admissioncriteria, targetpopulation), but haveinformal procedure toallow some persons withmental health problemsto be admitted.Expect substance usedisorders, and, withdocumentation, acceptsmental health disordersby routine and if mildand relatively stable.Program formallydefined like DDC butclinicians and programinformally expects andtreats both disorders, notwell documented.Clinicians and programexpect and treat bothdisorders, welldocumented.Addiction or peersupport (e.g. AA) onlyAvailable for bothdisorders but notroutinely offered orformally available.Available for bothmental health &substance use disorders,but distribution is lessfor mental healthproblems.Available for bothmental health &substance use disorderswith equivalentdistribution.Available for theinteraction between bothmental health andsubstance use disorders.12345
4AOSIII. CLINICALPROCESS:ASSESSMENTIIIA. Routine screeningmethods for psychiatricsymptomsDDCDDEPre-admission screeningbased on patient selfreport.Decision based onclinician inference frompatient presentation orby history.Pre-admission screeningfor symptom &treatment history, currentmedications,suicide/homicide historyprior to admission.Routine set of standardinterview questions forMH using genericframework, e.g. ASAMPPC (Dimension III) or“Biopsychosocial” datacollection.Screen for mental healthproblems usingstandardized or formalinstruments withestablished psychometricproperties.Standardized or formalinstruments for bothmental health andsubstance use disorderswith establishedpsychometric properties.IIIB. Routine assessmentif screened positive forpsychiatric symptomsOngoing monitoring forappropriateness orexclusion from programFormal mental healthassessment, if necessary,typically occurs.Psychiatric diagnoses arenot made or recordedMental health diagnosisvariably recorded inchart.Increased capacity toaccess follow-up mentalhealth assessments,although notstandardized or routine.Mental health diagnosismore frequently recordedbut inconsistentlyStandardized or formalintegrated assessment isroutine in all cases.IIIC. Psychiatric andsubstance use diagnosesmade and documented.More detailedbiopsychosocialassessment, mental statusexam, each cliniciandrivenMental health diagnosticimpressions made andrecorded variably.IIID. Psychiatric andsubstance use historyreflected in medicalrecord.Collection of substanceuse disorder history only.Standard form collectssubstance use disorderhistory only. Mentalhealth history collectedinconsistently.Routine documentationof both mental healthand substance usedisorder history in recordin narrative section.Specific section inrecorded dedicated tohistory and chronologyof course of bothdisorders.IIIE. Programacceptance based onpsychiatric symptomacuity: low, moderate,high.IIIF. Programacceptance based onseverity of persistenceand disability: low,moderate, high.Admits persons with noto low acuity.Admits persons inprogram with low tomoderate acuity, but whoare primarily stable.Admits persons inprogram with no to lowseverity of persistence ofdisabilityAdmits persons inprogram with low tomoderate severity.Specific section in recorddevoted to history andchronology of course ofboth disorders and theinteraction between themis examined temporally.Admits persons inprogram with moderateto high acuity, includingthose unstable in theirpsychiatric condition.Admits persons inprogram with moderateto high severityIIIG. Stage-wiseassessmentNot assessed ordocumented.Formal measure usedand routinelydocumented butfocusing on substanceuse disorders motivationonly.4Formal measure usedand routinelydocumented, focus onboth substance use andmental healthmotivation.51Assessed & documentedvariably by individualclinicianClinician assessed androutinely documented,focused on substance usedisorders motivation23Standard & routinemental health diagnosesconsistently made.
5AOSIV. CLINICALPROCESS:TREATMENTIVA. Treatment plans.DDCAddress addiction only(Mental health not listed)Variable by individualclinicianSubstance use disordersaddressed as primary,mental health assecondaryClinical focus in narrative(treatment plan orprogress note) on mentalhealth problem changeIVB. Assess and monitorinteractive courses ofboth disorders.No attention ordocumentation ofprogress with mentalhealth problemsVariable reports ofprogress on mentalhealth problems byindividual clinicians.IVC. Procedures forpsychiatric emergenciesand crisis management.No guidelines conveyedin any manner.Verbally conveyed inhouse guidelines.Documented guidelines:Referral or collaborations(to local mental healthagency or E/R)IVD. Stage-wisetreatmentNot assessed or explicitin treatment plan.Stage or motivationdocumented variably byindividual clinician intreatment plan.Stage or motivationroutinely incorporatedinto individualized plan,but no specific stage-wisetreatments.IVE. Policies andprocedures formedication evaluation,management, monitoringand compliance.Patients on medsroutinely not accepted.No capacities to monitor,guide or providepsychotropicmedications duringtreatment.Certain types of meds arenot acceptable. Or musthave own supply forentire treatment episode.Some capacity tomonitor psychotropicmedications.Present, coordinatedmedication policies.Some access toprescriber forpsychotropicmedications and policiesto guide the prescribingwithin the program isprovided. Monitoring ofthe medication is largelyprovided by theprescriber.123DDESystematic focus inavailable but variablyused.Address both as primary,both listed in planconsistently.Systematic focus isavailable but variablyused.Clear, detailed, andsystematic focus onchange in both substanceuse and mental healthdisorders.Routine capability, or aprocess to ascertain riskwith ongoing use ofsubstances; Maintain inprogram unlesscommitment iswarrantedStage or motivationroutinely incorporatedinto individualized plan,and formally prescribedand delivered stage-wisetreatments for bothsubstance use and mentalhealth issues.Clear standards androutine for medicatingprovider who is also astaff member andpresent on treatmentteams or administration.Full access to prescriberwith appropriateprescribing guidelines inplace. As a treatmentteam member, theprescriber informs theteam about themedication plan and theentire team can assistwith monitoring.5Stage or motivationroutinely incorporatedinto individualized plan,and general awareness ofadjusting treatments byindividual stage ofreadiness on substanceuse motivation only.Clear standards androutine for medicatingprovider who is also astaff member. Regularaccess to prescriber andguidelines for prescribingin place. The prescribermight more regularlyconsult with other staffregarding medicationplan and recruit otherstaff to assist withmedication monitoring4
6AOSIV. CLINICALPROCESS:TREATMENT (cont)IVF. Specializedinterventions withmental health content.DDCNot addressed inprogram contentBased on judgment byindividual clinician;Irregular penetration intoroutine servicesIVG. Education aboutpsychiatric disorder & itstreatment, andinteraction withsubstance use & itstreatment.IVH. Family educationand support.NoVariablyFor alcohol or drugproblems onlyIVI. Specializedinterventions to facilitateuse of peer supportgroups in planning orduring treatment.IVJ. Availability of peerrecovery supports forpatients with CODs.DDEIn program format asgeneralized intervention,e.g. stress management);More regular penetrationinto routine services.Routine clinicianadaptation of anevidence-based addictiontreatment (e.g. MI, CBT,TSF)Present in generic formatand content, anddelivered in individualand/or group formats.Some specializedinterventions byspecifically trainedclinicians in addition toroutine generalizedinterventions.Variably or by individualclinical judgmentMH issues regularly butinformally incorporatedinto family education orsupport sessions.Available as needed.Generic group on site forfamilies on substance useand mental issues,variably offered.Structured group withmore routine accessibilityNone used to facilitateeither use of addiction ormental health peersupportUsed variably by orinfrequently by individualclinicians, for individualpatients, mostly forfacilitation of addictionpeer support groupsPresent, generic formaton site, but no specific orintentional facilitationbased on mental healthproblems. More routinefacilitation of traditionaladdiction peer supportgroups (e.g. AA, NA)Not present, or if presentnot recommended.Off site, recommendedvariablyPresent, off site andfacilitated with contactpersons or informalmatching with peersupports in thecommunity, some cooccurring focus.3Present but variablefacilitation to peersupport groups targetingspecific mental healthissues, either totraditional peer supportgroups or those specificto both (e.g. DRA, DTR,etc).Present, off site,integrated into plan, androutinely documentedwith co-occurring focus.12Routine MH symptommanagement groups;Individual therapiesfocused on specificdisorders; Systematicadaptation of anevidence-based addictiontreatment (e.g. MI, CBT,TSF).Present specific contentfor specific disorder comorbidities, anddelivered in individualand/or group formats.4Routine and systematicco-occurring disorderfamily group integratedinto standard programformat. Accessed by themajority of families withco-occurring disorderfamily memberRoutine & specific toneed of co-occurringpersons, specialprograms on site,routinely targeted tospecific issues, either totraditional peer supportgroups or those specificto both (e.g. DRA).Present, on site,facilitated and integratedinto program (e.g. alumnigroups); Routinely usedand documented withco-occurring focus.5
7AOSV. CONTINUITYOF CAREVA. Co-occurringdisorder addressed indischarge planningprocess.DDCDDEBoth disorders seen asprimary, and plans madeand insured, on site, orby arrangement - off site,at least 80% of the time.Not addressedVariably addressed byindividual clinicians.Co-occurring disordersystematically addressedas secondary in planningprocess for off sitereferral.VB. Capacity to maintaintreatment continuity.No mechanism formanaging ongoing careof mental health needswhen addictiontreatment program iscompleted.No formal protocol tomanage mental healthneeds once program iscompleted, but someindividual clinicians mayprovide extended careuntil appropriate linkagetakes place; VariabledocumentationVC. Focus on ongoingrecovery issues for bothdisorders.NoIndividual cliniciandetermined.No formal protocol tomanage mental healthneeds once program iscompleted, but whenindicated, mostindividual cliniciansprovide extended careuntil appropriate linkagetakes place; RoutinedocumentationRoutine focus is onrecovery from addiction,mental health issues areviewed as potentialrelapse issues only.VD. Facilitation of peersupport groups for cooccurring disorders isdocumented and a focusin discharge planning,and connections areinsured to communitypeer recovery supportgroups.VE. Sufficient supplyand compliance plan formedications isdocumented.NoRarely, but addressed byindividual cliniciansNo medications in plan.1Formal protocol tomanage mental healthneeds indefinitely, butvariable documentedevidence that this isroutinely practiced,typically within the sameprogram or agency.Routine focus onaddiction recovery andmental health illnessmanagement andrecovery, both seen asprimary and ongoing.Yes, routine andsystematic, at least 80%of the time with focus onco-occurring disorderspeer support communityconnection (engagementin meetings or functionsoff-site).Yes, variable, but notroutine or systematic,focus on co-occurringdisorders peer supportcommunity connection(engagement in meetingsor functions off-site)Yes, 30-day or supply tonext appointment offsite.23Formal protocol tomanage mental healthneeds indefinitely andconsistent documentedevidence that this isroutinely practiced,typically within the sameprogram or agency.Maintains medicationmanagement in programwith provider.45
8AOSVI. STAFFINGVIA. Psychiatrist orother physician orprescriber ofpsychotropicmedications.DDCDDENo formal relationshipwith a prescriber for thisprogram.Consultant or contractoroff site.Consultant or contractoron site.Staff member, present onsite for clinical mattersonlyStaff member, present onsite for clinical,supervision, treatmentteam, and/oradministration.VIB. On site clinicalstaff members withmental health licensure(doctoral or masterslevel), or competency.No formal relationshipwith program.1-24% of clinical staffmembers.25-33% of clinical staffmembers.34-49% of clinical staffmembers.50% or more of clinicalstaff members.VIC. Access to mentalhealth supervision orconsultation.NoYes, off site byconsultant,undocumented.Yes, on site supervisionprovided PRN.Informal process.Yes, on site supervision.Provided regularly.Irregular documentation.Yes, on site, documentedregular supervisionsessions for clinicalmatters.VID. Case review,staffing or utilizationreview proceduresemphasize and supportco-occurring disordertreatment.NoVariable, by off siteconsultant,undocumented.Yes, on site, documentedas needed (PRN) andwith co-occurringdisorder issues.Yes. Documented,routine and systematiccoverage of co-occurringissues.VIE. Peer/Alumnisupports are availablewith co-occurringdisorders.NoPresent, but as part ofcommunity, androutinely available toprogram patients, eitherthru informalrelationships or moreformal connections suchas thru peer supportservice groups (e.g. AAhospital and institutionalcommittees; NAMI).3Present, on site, either aspaid staff, volunteers, orroutinely availableprogram “alumni”.1245
9AOSVII. TRAININGVIIA. Direct care staffmembers have basictraining in prevalence,common signs &symptoms, screening andassessment forpsychiatric symptomsand disorders.VIIB. Direct care staffmembers are crosstrained in mental healthand substance usedisorders, includingpharmacotherapies, andhave advancedspecialized training intreatment of personswith co-occurringdisorders.DDCDDENot trained in basicskills.Variably trained, notdocumented as part ofsystematic training plan,but encouraged bymanagement.Trained in basic skills peragency strategic trainingplan.Trained in these skills peragency strategic trainingplan, and also have someadvanced training inspecialized treatmentapproaches.Trained in these skills peragency strategic trainingplan, and also have staffwith advanced training inspecialized treatmentapproaches as part ofplan.Not trained, or notdocumented.At least 33% trained.At least 50% trainedAt least 75% are trainedAt least 90% are trained.ADDITIONAL SITE VISIT NOTES:DUAL DIAGNOSIS CAPABILITY IN ADDICTION TREATMENT PROGRAMS (DDCAT) V ER SION 3.2SCORING SUMMARY
10I. Program StructureA.B.C.D.Sum Total /4 SCOREII. Program MilieuA.B.Sum Total /2 SCOREIII. Clinical Process: AssessmentA.B.C.D.E.F.G.Sum Total /7 SCOREV. Continuity of CareA.B.C.D.E.Sum Total /5 SCOREIV. Clinical Process: TreatmentA.B.C.D.E.F.G.H.I.J.VI. StaffingA.B.C.D.E.Sum Total /10 SCOREDDCAT INDEX PROGRAM CATEGORY: SCALE METHODOVERALL SCORE (Sum of Scale Scores/7):DUAL DIAGNOSIS CAPABILITY:AOS (1 - 1.99)AOS/DDC (2 - 2.99)DDC (3 - 3.49)DDC/DDE (3.5 - 4.49)DDE (4.5 - 5.0)DDCAT INDEX PROGRAM CATEGORY: CRITERION METHOD% CRITERIA MET FOR AOS (# of “1” scores/35):% CRITERIA MET FOR DDC (# of “3 or ” scores/35):% CRITERIA MET FOR DDE (# of “5” scores/35):100%HIGHEST LEVEL OF DD CAPABILITY (80% or more):Sum Total /5 SCOREVII. TrainingA.B.Sum Total /2 SCORE
assessment, mental status exam, each clinician driven Formal mental health assessment, if necessary, typically occurs. Increased capacity to access follow-up mental health assessments, although not standardized or routine. Standardized or formal integrated assessment is routine in all cases. IIIC. Psychiatric and substance use diagnoses