Transcription
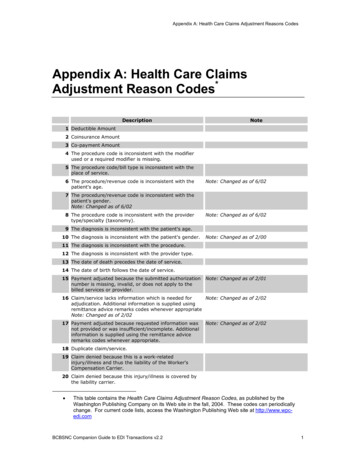
Appendix A: Health Care Claims Adjustment Reasons CodesAppendix A: Health Care ClaimsAdjustment Reason Codes*DescriptionNote1 Deductible Amount2 Coinsurance Amount3 Co-payment Amount4 The procedure code is inconsistent with the modifierused or a required modifier is missing.5 The procedure code/bill type is inconsistent with theplace of service.6 The procedure/revenue code is inconsistent with thepatient's age.Note: Changed as of 6/027 The procedure/revenue code is inconsistent with thepatient's gender.Note: Changed as of 6/028 The procedure code is inconsistent with the providertype/specialty (taxonomy).Note: Changed as of 6/029 The diagnosis is inconsistent with the patient's age.10 The diagnosis is inconsistent with the patient's gender.Note: Changed as of 2/0011 The diagnosis is inconsistent with the procedure.12 The diagnosis is inconsistent with the provider type.13 The date of death precedes the date of service.14 The date of birth follows the date of service.15 Payment adjusted because the submitted authorizationnumber is missing, invalid, or does not apply to thebilled services or provider.Note: Changed as of 2/01Note: Changed as of 2/0216 Claim/service lacks information which is needed foradjudication. Additional information is supplied usingremittance advice remarks codes whenever appropriateNote: Changed as of 2/0217 Payment adjusted because requested information wasnot provided or was insufficient/incomplete. Additionalinformation is supplied using the remittance adviceremarks codes whenever appropriate.Note: Changed as of 2/0218 Duplicate claim/service.19 Claim denied because this is a work-relatedinjury/illness and thus the liability of the Worker'sCompensation Carrier.20 Claim denied because this injury/illness is covered bythe liability carrier. This table contains the Health Care Claims Adjustment Reason Codes, as published by theWashington Publishing Company on its Web site in the fall, 2004. These codes can periodicallychange. For current code lists, access the Washington Publishing Web site at http://www.wpcedi.comBCBSNC Companion Guide to EDI Transactions v2.21
Appendix A: Health Care Claims Adjustment Reasons CodesDescriptionNote21 Claim denied because this injury/illness is the liabilityof the no-fault carrier.22 Payment adjusted because this care may be covered by Note: Changed as of 2/01another payer per coordination of benefits.23 Payment adjusted because charges have been paid byanother payer.Note: Changed as of 2/0124 Payment for charges adjusted. Charges are coveredunder a capitation agreement/managed care plan.Note: Changed as of 6/0025 Payment denied. Your Stop loss deductible has notbeen met.26 Expenses incurred prior to coverage.27 Expenses incurred after coverage terminated.28 Coverage not in effect at the time the service wasprovided.Note: Inactive for 004010, since 6/98.Redundant to codes 26&27.29 The time limit for filing has expired.30 Payment adjusted because the patient has not met therequired eligibility, spend down, waiting, or residencyrequirements.Note: Changed as of 2/0131 Claim denied as patient cannot be identified as ourinsured.32 Our records indicate that this dependent is not aneligible dependent as defined.33 Claim denied. Insured has no dependent coverage.34 Claim denied. Insured has no coverage for newborns.35 Lifetime benefit maximum has been reached.Note: Changed as of 10/0236 Balance does not exceed co-payment amount.Note: Inactive for 00304037 Balance does not exceed deductible.Note: Inactive for 00304038 Services not provided or authorized by designated(network/primary care) providers.Note: Changed as of 6/0339 Services denied at the time authorization/precertification was requested.40 Charges do not meet qualifications for emergent/urgentcare.41 Discount agreed to in Preferred Provider contract.Note: Inactive for 00304042 Charges exceed our fee schedule or maximumallowable amount.43 Gramm-Rudman reduction.44 Prompt-pay discount.45 Charges exceed your contracted/ legislated feearrangement.46 This (these) service(s) is (are) not covered.Note: Inactive for 004010, since 6/00. Usecode 96.47 This (these) diagnosis(es) is (are) not covered,missing, or are invalid.Note: Changed as of 6/0048 This (these) procedure(s) is (are) not covered.Note: Inactive for 004010, since 6/00. Usecode 96.49 These are non-covered services because this is aroutine exam or screening procedure done inconjunction with a routine exam.50 These are non-covered services because this is notdeemed a medical necessity' by the payer.BCBSNC Companion Guide to EDI Transactions v2.22
Appendix A: Health Care Claims Adjustment Reasons CodesDescriptionNote51 These are non-covered services because this is a preexisting condition52 The referring/prescribing/rendering provider is noteligible to refer/prescribe/order/perform the servicebilled.Note: Changed as of 10/9853 Services by an immediate relative or a member of thesame household are not covered.54 Multiple physicians/assistants are not covered in thiscase .55 Claim/service denied because procedure/treatment isdeemed experimental/investigational by the payer.56 Claim/service denied because procedure/treatment hasnot been deemed proven to be effective' by the payer.57 Payment denied/reduced because the payer deems theinformation submitted does not support this level ofservice, this many services, this length of service, thisdosage, or this day's supply.Note: Inactive for 004050. Split into codes150, 151, 152, 153 and 154.Note: Changed as of 2/0158 Payment adjusted because treatment was deemed bythe payer to have been rendered in an inappropriate orinvalid place of service.59 Charges are adjusted based on multiple surgery rulesor concurrent anesthesia rules.Note: Changed as of 6/0060 Charges for outpatient services with this proximity toinpatient services are not covered.61 Charges adjusted as penalty for failure to obtain second Note: Changed as of 6/00surgical opinion.62 Payment denied/reduced for absence of, or exceeded,pre-certification/authorization.Note: Changed as of 2/0163 Correction to a prior claim.Note: Inactive for 00304064 Denial reversed per Medical Review.Note: Inactive for 00304065 Procedure code was incorrect. This payment reflectsthe correct code.Note: Inactive for 00304066 Blood Deductible.67 Lifetime reserve days. (Handled in QTY, QTY01 LA)Note: Inactive for 00304068 DRG weight. (Handled in CLP12)Note: Inactive for 00304069 Day outlier amount.70 Cost outlier - Adjustment to compensate for additonalcosts.Note: Changed as of 6/0171 Primary Payer amount.Note: Deleted as of 6/00. Use code 23.72 Coinsurance day. (Handled in QTY, QTY01 CD)Note: Inactive for 00304073 Administrative days.Note: Inactive for 00305074 Indirect Medical Education Adjustment.75 Direct Medical Education Adjustment.76 Disproportionate Share Adjustment.77 Covered days. (Handled in QTY, QTY01 CA)Note: Inactive for 00304078 Non-Covered days/Room charge adjustment.79 Cost Report days. (Handled in MIA15)Note: Inactive for 00305080 Outlier days. (Handled in QTY, QTY01 OU)Note: Inactive for 00305081 Discharges.Note: Inactive for 00304082 PIP days.Note: Inactive for 003040BCBSNC Companion Guide to EDI Transactions v2.23
Appendix A: Health Care Claims Adjustment Reasons CodesDescriptionNote83 Total visits.Note: Inactive for 00304084 Capital Adjustment. (Handled in MIA)Note: Inactive for 00305085 Interest amount.86 Statutory Adjustment.Note: Inactive for 004010, since 6/98.Duplicative of code 45.87 Transfer amount.88 Adjustment amount represents collection againstreceivable created in prior overpayment.Note: Inactive for 004050.89 Professional fees removed from charges.90 Ingredient cost adjustment.91 Dispensing fee adjustment.92 Claim Paid in full.Note: Inactive for 00304093 No Claim level Adjustments.Note: Inactive for 004010, since 2/99. In004010, CAS at the claim level is optional.94 Processed in Excess of charges.95 Benefits adjusted. Plan procedures not followed.Note: Changed as of 6/0096 Non-covered charge(s).97 Payment is included in the allowance for anotherservice/procedure.Note: Changed as of 2/9998 The hospital must file the Medicare claim for thisinpatient non-physician service.Note: Inactive for 00304099 Medicare Secondary Payer Adjustment Amount.Note: Inactive for 003040100 Payment made to patient/insured/responsible party.101 Predetermination: anticipated payment uponcompletion of services or claim adjudication.Note: Changed as of 2/99102 Major Medical Adjustment.103 Provider promotional discount (e.g., Senior citizendiscount).Note: Changed as of 6/01104 Managed care withholding.105 Tax withholding.106 Patient payment option/election not in effect.107 Claim/service denied because the related or qualifyingclaim/service was not previously paid or identified onthis claim.Note: Changed as of 6/03108 Payment adjusted because rent/purchase guidelineswere not met.Note: Changed as of 6/02109 Claim not covered by this payer/contractor. You mustsend the claim to the correct payer/contractor.110 Billing date predates service date.111 Not covered unless the provider accepts assignment.112 Payment adjusted as not furnished directly to thepatient and/or not documented.Note: Changed as of 2/01113 Payment denied because service/procedure wasprovided outside the United States or as a result ofwar.Note: Changed as of 2/01; Inactive forversion 004060. Use Codes 157, 158 or159.114 Procedure/product not approved by the Food and DrugAdministration.Note: Changed as of 2/01115 Payment adjusted as procedure postponed or canceled.BCBSNC Companion Guide to EDI Transactions v2.24
Appendix A: Health Care Claims Adjustment Reasons CodesDescriptionNote116 Payment denied. The advance indemnification noticesigned by the patient did not comply withrequirements.Note: Changed as of 2/01117 Payment adjusted because transportation is onlycovered to the closest facility that can provide thenecessary care.Note: Changed as of 2/01118 Charges reduced for ESRD network support.119 Benefit maximum for this time period has beenreached.120 Patient is covered by a managed care plan.Note: Inactive for 004030, since 6/99. Usecode 24.121 Indemnification adjustment.122 Psychiatric reduction.123 Payer refund due to overpayment.Note: Inactive for 004030, since 6/99.Refer to implementation guide for properhandling of reversals.124 Payer refund amount - not our patient.Note: Inactive for 004030, since 6/99.Refer to implementation guide for properhandling of reversals.125 Payment adjusted due to a submission/billing error(s).Additional information is supplied using the remittanceadvice remarks codes whenever appropriate.Note: Changed as of 2/02126 Deductible -- Major MedicalNote: New as of 2/97127 Coinsurance -- Major MedicalNote: New as of 2/97128 Newborn's services are covered in the mother'sAllowance.Note: New as of 2/97129 Payment denied - Prior processing information appearsincorrect.Note: Changed as of 2/01130 Claim submission fee.Note: Changed as of 6/01131 Claim specific negotiated discount.Note: New as of 2/97132 Prearranged demonstration project adjustment.Note: New as of 2/97133 The disposition of this claim/service is pending furtherreview.Note: Changed as of 10/99134 Technical fees removed from charges.Note: New as of 10/98135 Claim denied. Interim bills cannot be processed.Note: New as of 10/98136 Claim Adjusted. Plan procedures of a prior payer werenot followed.Note: Changed as of 6/00137 Payment/Reduction for Regulatory Surcharges,Assessments, Allowances or Health Related Taxes.Note: New as of 2/99138 Claim/service denied. Appeal procedures not followedor time limits not met.Note: New as of 6/99139 Contracted funding agreement - Subscriber is employed Note: New as of 6/99by the provider of services.140 Patient/Insured health identification number and namedo not match.Note: New as of 6/99141 Claim adjustment because the claim spans eligible andineligible periods of coverage.Note: Changed as of 6/00142 Claim adjusted by the monthly Medicaid patient liability Note: New as of 6/00amount.143 Portion of payment deferred.Note: New as of 2/01144 Incentive adjustment, e.g. preferred product/service.Note: New as of 6/01BCBSNC Companion Guide to EDI Transactions v2.25
Appendix A: Health Care Claims Adjustment Reasons CodesDescriptionNote145 Premium payment withholdingNote: New as of 6/02146 Payment denied because the diagnosis was invalid forthe date(s) of service reported.Note: New as of 6/02147 Provider contracted/negotiated rate expired or not onfile.Note: New as of 6/02148 Claim/service rejected at this time because information Note: New as of 6/02from another provider was not provided or wasinsufficient/incomplete.149 Lifetime benefit maximum has been reached for thisservice/benefit category.Note: New as of 10/02150 Payment adjusted because the payer deems theinformation submitted does not support this level ofservice.Note: New as of 10/02151 Payment adjusted because the payer deems theinformation submitted does not support this manyservices.Note: New as of 10/02152 Payment adjusted because the payer deems theinformation submitted does not support this length ofservice.Note: New as of 10/02153 Payment adjusted because the payer deems theinformation submitted does not support this dosage.Note: New as of 10/02154 Payment adjusted because the payer deems theinformation submitted does not support this day'ssupply.Note: New as of 10/02155 This claim is denied because the patient refused theservice/procedure.Note: New as of 6/03156 Flexible spending account paymentsNote: New as of 9/03157 Payment denied/reduced because service/procedurewas provided as a result of an act of war.Note: New as of 9/03158 Payment denied/reduced because theservice/procedure was provided outside of the UnitedStates.Note: New as of 9/03159 Payment denied/reduced because theservice/procedure was provided as a result ofterrorism.Note: New as of 9/03160 Payment denied/reduced because injury/illness was the Note: New as of 9/03result of an activity that is a benefit exclusion.161 Provider performance bonusNote: New as of 2/04Note: New as of 2/04162 State-mandated Requirement for Property andCasualty, see Claim Payment Remarks Code for specificexplanation.163 Claim/Service adjusted because the attachmentreferenced on the claim was not received.Note: New as of 6/04164 Claim/Service adjusted because the attachmentreferenced on the claim was not received in a timelyfashion.Note: New as of 6/04A0 Patient refund amount.A1 Claim denied charges.A2 Contractual adjustment.Note: Inactive for version 004060. UseCode 45 with Group Code 'CO' or useanother appropriate specific adjustmentcode.A3 Medicare Secondary Payer liability met.Note: Inactive for 004010, since 6/98.BCBSNC Companion Guide to EDI Transactions v2.26
Appendix A: Health Care Claims Adjustment Reasons CodesDescriptionNoteA4 Medicare Claim PPS Capital Day Outlier Amount.A5 Medicare Claim PPS Capital Cost Outlier Amount.A6 Prior hospitalization or 30 day transfer requirement notmet.A7 Presumptive Payment AdjustmentA8 Claim denied; ungroupable DRGB1 Non-covered visits.B2 Covered visits.Note: Inactive for 003040B3 Covered charges.Note: Inactive for 003040B4 Late filing penalty.B5 Payment adjusted because coverage/programguidelines were not met or were exceeded.Note: Changed as of 2/01B6 This payment is adjusted when performed/billed by this Note: Changed as of 2/01type of provider, by this type of provider in this type offacility, or by a provider of this specialty.B7 This provider was not certified/eligible to be paid forthis procedure/service on this date of service.Note: Changed as of 10/98B8 Claim/service not covered/reduced because alternativeservices were available, and should have been utilized.B9 Services not covered because the patient is enrolled ina Hospice.B10 Allowed amount has been reduced because acomponent of the basic procedure/test was paid. Thebeneficiary is not liable for more than the charge limitfor the basic procedure/test.B11 The claim/service has been transferred to the properpayer/processor for processing. Claim/service notcovered by this payer/processor.B12 Services not documented in patients' medical records.B13 Previously paid. Payment for this claim/service mayhave been provided in a previous payment.B14 Payment denied because only one visit or consultationper physician per day is covered.Note: Changed as of 2/01B15 Payment adjusted because this procedure/service is not Note: Changed as of 2/01paid separately.B16 Payment adjusted because New Patient' qualificationswere not met.Note: Changed as of 2/01B17 Payment adjusted because this service was notprescribed by a physician, not prescribed prior todelivery, the prescription is incomplete, or theprescription is not current.Note: Changed as of 2/01B18 Payment denied because this procedure code/modifierwas invalid on the date of service or claim submission.Note: Changed as of 2/01B19 Claim/service adjusted because of the finding of aReview Organization.Note: Inactive for 003070B20 Payment adjusted because procedure/service waspartially or fully furnished by another provider.Note: Changed as of 2/01B21 The charges were reduced because the service/carewas partially furnished by another physician.Note: Inactive for 003040B22 This payment is adjusted based on the diagnosis.Note: Changed as of 2/01BCBSNC Companion Guide to EDI Transactions v2.27
Appendix A: Health Care Claims Adjustment Reasons CodesDescriptionNoteB23 Payment denied because this provider has failed anaspect of a proficiency testing program.Note: Changed as of 2/01D1 Claim/service denied. Level of subluxation is missing or Note: Inactive for 004010, since 2/99. Useinadequate.code 16 and remark codes if necessary.D2 Claim lacks the name, strength, or dosage of the drugfurnished.Note: Inactive for 004010, since 2/99. Usecode 16 and remark codes if necessary.D3 Claim/service denied because information to indicate ifthe patient owns the equipment that requires the partor supply was missing.Note: Inactive for 004010, since 2/99. Usecode 16 and remark codes if necessary.D4 Claim/service does not indicate the period of time forwhich this will be needed.Note: Inactive for 004010, since 2/99. Usecode 16 and remark codes if necessary.D5 Claim/service denied. Claim lacks individual lab codesincluded in the test.Note: Inactive for 004010, since 2/99. Usecode 16 and remark codes if necessary.D6 Claim/service denied. Claim did not include patient'smedical record for the service.Note: Inactive for 004010, since 2/99. Usecode 16 and remark codes if necessary.D7 Claim/service denied. Claim lacks date of patient's most Note: Inactive for 004010, since 2/99. Userecent physician visit.code 16 and remark codes if necessary.D8 Claim/service denied. Claim lacks indicator that x-rayis available for review.'Note: Inactive for 004010, since 2/99. Usecode 16 and remark codes if necessary.D9 Claim/service denied. Claim lacks invoice or statementcertifying the actual cost of the lens, less discounts orthe type of intraocular lens used.Note: Inactive for 004010, since 2/99. Usecode 16 and remark codes if necessary.D10 Claim/service denied. Completed physician financialrelationship form not on file.Note: Inactive for 003070, since 8/97. Usecode 17.D11 Claim lacks completed pacemaker registration form.Note: Inactive for 003070, since 8/97. Usecode 17.Note: Inactive for 003070, since 8/97. UseD12 Claim/service denied. Claim does not identify whoperformed the purchased diagnostic test or the amount code 17.you were charged for the test.D13 Claim/service denied. Performed by a facility/supplier in Note: Inactive for 003070, since 8/97. Usewhich the ordering/referring physician has a financialcode 17.interest.D14 Claim lacks indication that plan of treatment is on file.Note: Inactive for 003070, since 8/97. Usecode 17.D15 Claim lacks indication that service was supervised orevaluated by a physician.Note: Inactive for 003070, since 8/97. Usecode 17.D16 Claim lacks prior payer payment information.New as of 06/04 Inactive as of version5010. Use code 16 with appropriate claimpayment remark code [N4].D17 Claim/Service has invalid non-covered days.Note: Inactive as of version 5010. Usecode 16 with appropriate claim paymentremark code [M32, M33].D18 Claim/Service has missing diagnosis information.Note: Inactive as of version 5010. Usecode 16 with appropriate claim paymentremark code [MA63, MA65].D19 Claim/Service lacks Physician/Operative or othersupporting documentationNote: Inactive as of version 5010. Usecode 16 with appropriate claim paymentremark code [M29, M30, M35, M66].D20 Claim/Service missing service/product information.Note: Inactive as of version 5010. Usecode 16 with appropriate claim paymentremark code [M20, M67, M19, MA67].W1 Workers Compensation State Fee Schedule AdjustmentBCBSNC Companion Guide to EDI Transactions v2.2Note: New as of 2/008
Appendix A: Health Care Claims Adjustment Reasons CodesBCBSNC Companion Guide to EDI Transactions v2.29
Appendix A: Health Care Claims Adjustment Reasons Codes Description Note 83 Total visits. Note: Inactive for 003040 84 Capital Adjustment.(Handled in MIA) Note: Inactive for 003050 85 Interest amount. 86 Statutory Adjustment. Note: Inactive for 004010, since 6/98.