Transcription
X-ray Imaging (XRI)Lectures on Medical BiophysicsLectures on Medical BiophysicsDept. Biophysics, Medical Faculty,Masaryk University in BrnoWilhelm Conrad Roentgen1845 - 1923Godfrey N. Hounsfield1919 - 2004X-ray Imaging (XRI)
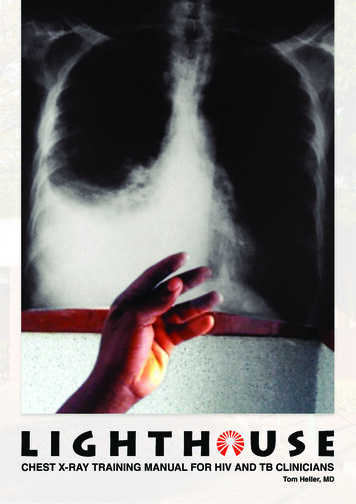
Lectures on Medical BiophysicsX-ray Imaging (XRI)X-Ray Imaging X-ray imaging (XRI) is still one of the most importantdiagnostic methods used in medicine. It provides mainlymorphological (anatomical) information - but may alsoprovide some physiological (functional) information. Its physical basis is the different attenuation of X-raysin different body tissues. We have to keep in mind that X-rays may lead to serioushealth effects (e.g., cancer) for both patients andhealthcare professionals (HCP). Thus, strict legal radiationprotection safety measures exist to avoid anyunnecessary harm to both patients and the HCP. We will2deal with them in a special lecture.
Lectures on Medical BiophysicsX-ray Imaging (XRI)Content of the Lecture Projection XRI devices Image formation Projection X-ray devices for special purposes CT Radiation dose and health risk3
Lectures on Medical BiophysicsX-ray Imaging (XRI)Projection XRI Devices4
Lectures on Medical BiophysicsX-ray Imaging (XRI)X-Ray Production – Low Power X-Ray Tubeused in Dental UnitsScheme of an X-ray tube. K – hot filament cathode, W – tungsten plate. 5
Lectures on Medical BiophysicsX-ray Imaging (XRI)High-Power Rotating Anode Tube6
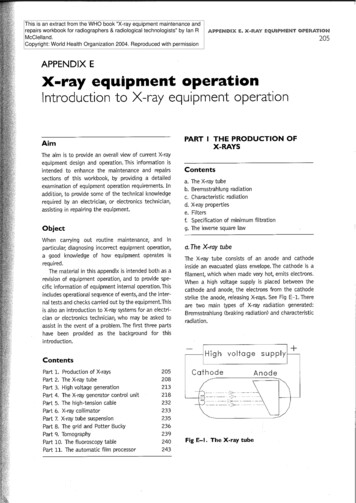
X-ray Imaging (XRI)Lectures on Medical BiophysicsProduction of X-rays An electron with an electric charge e (1.602·10-19 C) inan electrostatic field with potential difference U (voltage,in this case it is the voltage across the anode and thecathode) has potential energy Ep:Ep Ue In the moment just before impact of the electron ontothe anode, its potential energy Ep is fully transformedinto its kinetic energy EK. Thus:Ep EK Ue ½ mv2 On impact, the EK is transformed into x-ray photonenergy (less than 1%) and heat energy (99%). This heatcan damage the tube.7
X-ray Imaging (XRI)Lectures on Medical BiophysicsPhoton Energy and Tube Voltage If ALL the kinetic energy of the accelerated electronis transformed into a SINGLE X-ray photon, thisphoton will have energy:E hf Ue This is the maximum energy of the emitted photons.It is directly proportional to the voltage U across the,anode and cathode. Hence if we want to increase the energy of thephotons all we have to do is increase the voltage! The higher the energy of the photons the less theyare attenuated by the body - the higher thepenetration. This is important when imaging thickbody parts or fat patients!8
Lectures on Medical BiophysicsX-ray Imaging (XRI)Photon Energy HistogramNumber ofphotonswithcertainamount ofenergyE9
Lectures on Medical BiophysicsX-ray Imaging (XRI)Main Parts of the XRI Device X-ray tube Voltage-Current Generator:- High Voltage Transformer – supplies high voltage (up to 150kV)- Rectifier - produces unidirectional tube electron current- When increasing the magnitude of the electron beam current (bychanging the cathode heating) the photon fluence rate (i.e. numberof photons per unit area per second) of the X-ray beam increases however the energy of individual photons does not.- The energy of the individual photons can be increased byincreasing the voltage between the anode and cathode. Control panel – today most parameters of the device (includingvoltage and current) are controlled by means of a computer. It islocated outside the examination room or behind a shield made of glasscontaining lead (to protect the radiological assistant). Main mechanical parts: tube stand, examination table, grid forremoving scattered photons (‘Bucky’), X-ray detector: cassette with radiographic film and adjacentfluorescent screens (in radiography) or image intensifier (both on theway out) or flat panel digital detector (in fluoroscopy or in general).10
Lectures on Medical BiophysicsX-ray Imaging (XRI)Passage of X-rays through Patient's Body X-rays emitted from a small focal area of the anodepropagate in all directions. In the tube envelope,some low energy photons are absorbed. Furtherabsorption of these photons occurs in the primaryfilter, made of aluminium sheet. It absorbs low energyphotons which would be absorbed by surface tissuesand do not contribute to the image formation(unnecessary patient dose). X-ray beam is delimitedby rectangular collimator plates made of lead. The rays then pass through the body wheretransmission or absorption or scattering may occur.After that they pass through the grid, which is in frontof the detector to remove scattered photons as thesewould degrade the image.11
Lectures on Medical BiophysicsX-ray Imaging (XRI)Image Formation X-ray image is an analogy of a ‘shadow’ cast by asemitransparent and structured body illuminated bylight beam coming form an almost point source. Theimage is formed due to different attenuation of thebeam by the different body tissues and by projection ofthe structures on a film or an electronic X-ray detector. The image can be visualised by means of– Radiographic film / screen and subsequent development– Digital plate and displaying image on a PC monitor– Image intensifier and digital CCD camera connected to amonitor12
X-ray Imaging (XRI)Lectures on Medical BiophysicsAttenuation of RadiationA beam of X-rays (any radiation) passes through a substance:absorption scattering attenuationA small decrease of radiation intensity -dI in a thin substance layer isproportional to its thickness dx, intensity I of radiation falling on the layer,and a specific constant m:-dI I.dx.mAfter rewriting:dI/I -dx.mAfter integration:I I0e-mxI is intensity of radiation passed through the layer of thickness x, I0 is theintensity of incoming radiation, m is linear coefficient of attenuation [m-1]depending on kind of radiation, medium and its density.The mass attenuation coefficient m/r does not depend on the density.13
X-ray Imaging (XRI)Lectures on Medical BiophysicsCassettes for Radiographic FilmsFLUORESCENTscreens reducedose of radiationabout 50-times14
X-ray Imaging (XRI)Lectures on Medical BiophysicsDigital Imaging PlatesImaging plate consists of an arrayof very small sensorsMatrix of amorphous silicon(aSi) photodiode lightsensors„bucky“ – seeslide 24Phosphorescent layer of CsI (necessaryfor patient dose reduction as aSi is notgood absorber of X-rays)electronic signal15
Lectures on Medical BiophysicsX-ray Imaging (XRI)Image IntensifierR – X-ray tube, P - patient, O1 – primary picture on a fluorescentscreen, G – glass carrier, F – fluorescent screen, FK - photocathode,FE – focussing electrodes (electron optics), A - anode, O2 – secondaryimage on the anodic screen, V – video-camera. Individual parts are notproportionally depicted.16
Lectures on Medical BiophysicsX-ray Imaging (XRI)Different Ways how to Obtain DIGITAL Images(mammographic 5n1/department7.html
Lectures on Medical BiophysicsX-ray Imaging (XRI)Blurring of the ImageNo radiograph (an X-ray image) is absolutely sharp. Boundariesbetween tissues are depicted as a gradual change of grayscale. This non-sharpness (blurring) has several reasons:1)Movement blur – accidental, breathing, pulse waves, heartaction etc. They can be reduced by shorter exposure times withmore intense X-ray radiation.2)Geometric blur is caused by finite focal area (focus is not apoint). The rays fall on the boundary of differently absorbingmedia under different angles – blurring of their contoursappears3)The light emitted by fluorescent screens attached to the film ordigital detector does not only illuminate the corresponding partof the film or detector, but also spreads out to surroundingareas.18
Lectures on Medical BiophysicsX-ray Imaging (XRI)Geometric Blur (‘penumbra’)Geometric penumbra can be reduced by:-Choosing a small focal spot size (but it increases risk of damage totube anode by heating)- Decreasing the distance between the patient and the detector- Increasing the distance between the X-ray tube and the patient19
Lectures on Medical BiophysicsX-ray Imaging (XRI)Interactions of X-ray Photons withMatter: ABSORPTION by PhotoelectricEffect (PE) Photon disappears (‘is absorbed’) after hitting an atom and an electronis ejected from electron shell of the atom (typically K-shell). Part of thephoton energy hf is necessary for ionisation. Remaining part of thephoton energy changes into kinetic energy (1/2mv2) of the ejectedelectron. The electron knocks electrons out of atoms of the body andproduces ionization of these atoms. The Einstein equation forphotoelectric effect holds:hf Eb 1/2mv2,Eb is binding (ionisation) energy of the electron (called also work function). The probability for PE increases with proton number and decreaseswith increasing photon energy (this explains why lead is used forshielding and why higher energy beams are more penetrating)20
X-ray Imaging (XRI)Lectures on Medical BiophysicsPhotoelectric EffectSecondary electronPrimary photon21
Lectures on Medical BiophysicsX-ray Imaging (XRI)Interactions of X-ray Photons withMatter: Compton Scatter (CS) At higher energies of photons, the photon energy is not fullyabsorbed – a photon of lower energy appears. The bindingenergy of the electron Eb is negligible in comparison with thephoton energy. We can write:hf1 (Eb) hf2 1/2mv2, where f1 is frequency of incident photon and f2 is frequency ofthe scattered photon. CS is more probable than PE for primary photon energies 0.5 - 5MeV which explains why images at such energies would bepractically useless.22
Lectures on Medical BiophysicsX-ray Imaging (XRI)Compton ScatterSecondary electronPrimary photon23
X-ray Imaging (XRI)Lectures on Medical BiophysicsPrinciple of the Bucky GridThe Bucky grid stops a substantialpart of the scattered rays whilstallowing the useful photons to passthrough. However unfortunatelygrids also absorb part of the usefulradiation. Hence a higher amountof x-rays must be used to producea good image – this increases thedose of radiation to the patient.Hence for example grids are notused with thin children as the levelof scatter is low anyway.http://www.cwm.co.kr/pro213.htm24
Lectures on Medical BiophysicsX-ray Imaging (XRI)Use of the Contrast Agents The soft tissues only slightly differ in their attenuation.Therefore they cannot be distinguished in a commonradiograph. That is the reason for the use ofpharmaceuticals called contrast agents. The attenuation of certain tissues can be increased orlowered. Positive contrast is achieved by substanceshaving a high proton number as the probability of thephotoelectric effect is increased. A suspension ofbarium sulphate, “barium meal”, is used for imagingand functional examination of GIT. In examinations ofblood, biliary and urinary vessels etc. compounds withhigh content of iodine are used. Hollow inner body organs can be visualised by negativecontrast. Air or better CO2 can be used. The cavities arefilled by gas, inflated, so that they can be visualised asstructures of very low attenuation (pleural space,peritoneum, brain chambers).25
X-ray Imaging (XRI)Lectures on Medical BiophysicsPositive and Negative ContrastHorseshoe kidney –positive rast image of theappendix – diverticulosis –combination with .jpgPneumoencephalograph– negative contrast –history of roanatomy/slide/k42.jpg
Lectures on Medical BiophysicsX-ray Imaging (XRI)Devices for Special Uses - Examples Dental X-ray devices Mammographic devices Angiography (image subtraction systems,formerly image intensifier based; nowincreasingly digital detector based)27
Lectures on Medical BiophysicsX-ray Imaging (XRI)X-ray Devices in mic screening lix-9000.htmX-ray image of adental implant28
Lectures on Medical BiophysicsX-ray Imaging (XRI)MammographyMammography is the process of using low-dose X-rays (usuallyaround 0.7 mSv) to examine the female breast. It is used to look fordifferent types of tumours and cysts. In some countries routine (annualto five-yearly) mammography of older women is encouraged as ascreening method to diagnose early breast cancer. It is normal to uselow energy (soft) X-rays (molybdenum anode).29
Lectures on Medical BiophysicsX-ray Imaging (XRI)Digital Subtraction Angiographyhttp://zoot.radiology.wisc.edu/ block/Med Gallery/ia dsa.html30
Lectures on Medical BiophysicsX-ray Imaging (XRI)Computerised Tomography - CT The first patient was examined by this method inLondon, 1971. The apparatus was invented by English physicistHounsfield, (together with American Cormack, Nobelaward for medicine, 1979)31
Lectures on Medical BiophysicsX-ray Imaging (XRI)Principle of CT Principle: The CT scanner is a complexinstrument for measuring the X-rays attenuationin individual voxels (volume analogies of pixels)in narrow slices of tissues. Method of measurement: A narrow fan-beam ofX-rays is passed through the body and themerging radiation measured by an arc ofdetectors. This is repeated at different angles tillenough information is available to be able tocalculate the attenuation coefficient in the patientvoxels. A „map“ of attenuation is calculated – atomogram.32
X-ray Imaging (XRI)Lectures on Medical BiophysicsExamples of CT ScansMetastatic lesions in brainExtensive subcapsular haematomaof spleen in patient after umcdept/emergency/apr7xr1a.html33
Lectures on Medical BiophysicsX-ray Imaging (XRI)Advantages of CT over Projection XRI Much higher contrast than projection XRI - 0.5%difference in attenuation can be resolvedbecause:– Almost total elimination of effects of scatter– X-ray measurements are taken from many angles Thus, we can see and examine different softtissues. No overlapping of anatomical structures Less distortion as measurements are takenfrom many angles34
X-ray Imaging (XRI)Lectures on Medical BiophysicsFour Generations of CT1. Generation3. Generation2. Generation4. Generation35
Lectures on Medical BiophysicsX-ray Imaging (XRI)Principle of Spiral (3D) CTX-ray tube and detectors revolve around the shifting patient36
Lectures on Medical BiophysicsX-ray Imaging (XRI)Multislice CT and Cone beam CTFast 3D reconstruction is possible37
X-ray Imaging (XRI)Lectures on Medical BiophysicsHounsfield (CT) UnitsIn order to simplify calculations we use HounsfieldScale units (HU) for amount of attenuation.On this simplified scale water is 0 HU, air is -1000 HU,compact bone is about 1000 HU.A scale of 2000 HU is available for CT examination ofbody tissues. In most cases, it is senseless to attributethem to all of the grey scale levels (our eye is able todistinguish only about 250 levels of grey). Most of thesoft tissue HU values range from 0 to 100. Thus weuse only limited „diagnostic window“ of these units inpractice, e.g. from -100 to 100.W – waterHU T – tissuek 100038
Lectures on Medical BiophysicsX-ray Imaging (XRI)„Diagnostic Window“ of HU http://www.teaching-biomed.man.ac.uk/student projects/2000/mmmr7gjw/technique8.htm39
Lectures on Medical BiophysicsX-ray Imaging (XRI)3D CT - Color ducts/carestream-onsight-3d-extremity-system40
Lectures on Medical BiophysicsX-ray Imaging (XRI)Some Typical Doses From natural sources: 2 mSv per year Chest X-ray: 1 mSv Fluoroscopy: 5 mSv CT Scan: 10 mSv Medical doses are increasing with ‘better besafe than sorry’ medicine and the ease ofuse of modern imaging devices (e.g., spiralCT compared to conventional CT).41
Lectures on Medical BiophysicsX-ray Imaging (XRI)Appendix: Dental RadiographyDevices
Lectures on Medical BiophysicsX-ray Imaging (XRI)Direct Digital Dental RadiographySensor consists ofphotodiode matrixcovered with a scintillatorlayer. Wireless sensorsnow available (usingbluetooth or wifi).43
Lectures on Medical BiophysicsX-ray Imaging (XRI)Intra-Oral Image44
Lectures on Medical BiophysicsX-ray Imaging (XRI)Orthopantomographic (OPG) Unit45
Lectures on Medical BiophysicsX-ray Imaging (XRI)Extraoral OPG Image46
Lectures on Medical BiophysicsX-ray Imaging (XRI)Extraoral Cephalometric Image47
Lectures on Medical BiophysicsX-ray Imaging (XRI)Radiation Protection Considerations Low individual dose but high collective dosetechnique, particularly since many youngpatients Protect eye and thyroid (sometimes latter closeto or exposed to direct beam) As the dose, and therefore the risk to thedeveloping fetus is so low there is nocontraindication to radiography of women whoare or may be pregnant providing that it isclinically justified. Very Good reference is:– RP136 European guidelines on radiation protectionin dental radiology - The safe use of radiographs in48dental practice. 2004. EU publication.
Lectures on Medical BiophysicsX-ray Imaging (XRI)Dose Optimisation for Intraoral Devices– Constant power (CP) generator– filter: 1.5mm Al up to 70kV to reduce skin dose– Rectangular collimator recommended (if round-end collimatorused, beam diameter 60mm at patient end of cone)– Digital devices need lower dose than film Protocol– use 60kV with CP generator– minimum SSD 200mm (cone should ensure this)– There is no need to use a lead protective apron (to protectgonads, except in rare cases) even in cases of pregnantpatients. However in the case of pregnant patients, the use ofa lead apron continues to be used in some states as it mayreassure the patient– Some have suggested using thyroid collar for young patients(in CZ they use it even for adults)49
Lectures on Medical BiophysicsX-ray Imaging (XRI)Converting Round Collimators toRectangularThe UK’s Ionising Radiation(Medical Exposure)Regulations 2000recommend the use ofrectangular collimation tolimit the radiation dose apatient receives duringroutine dental X-rays.DENTSPLY’s RinnUniversal Collimator justclips onto any roundheaded long-cone X-rayunit, converting it fromround to the recommendedrectangular collimation, inone easy step.50
Lectures on Medical BiophysicsX-ray Imaging (XRI)Dose Optimisation in OPG Devices:– CP (constant power) generators– Automatic exposure control– Dead-man type switch Protocol:– Proper patient positioning and immobilisation toavoid repeats (e.g., in case of OPG chin rests onplastic support, head held by plastic earpieces,head surrounded by plastic guard)– Limit field size to area of interest– Thyroid collar inappropriate as it interferes with thebeam in the case of OPG (note however oftennecessary in the case of cephalometry)51
Authors:Vojtěch Mornstein, Carmel J. CaruanaContent collaboration:Ivo HrazdiraPresentation design:Lucie MornsteinováLast revision: December 2018
Lectures on Medical Biophysics X-ray Imaging (XRI) 2 X-Ray Imaging X-ray imaging (XRI) is still one of the most important diagnostic methods used in medicine. It provides mainly morphological (anatomical) information - but may also provide some physiological (functional) information. Its physical basis is the different attenuation of X-rays

![[AWS Black Belt Online Seminar] AWS X-Ray](/img/17/20200526-blackbelt-x-ray.jpg)