Transcription
Central Bringing Excellence in Open AccessArchives of Emergency Medicine and Critical CareResearch Article*Corresponding authorMariam Mostafa Al-Werdani, Mansoura School ofBasic Life Support Knowledgeof Medical Students: A SingleFaculty Study in Egyptmedicine, Mansoura University, AlGomhoria St.,Mansoura, Al Daqahlia, Egypt, Tel: 201019044121,Email:Submitted: 23 September 2018Accepted: 12 November 2018Published: 13 November 2018ISSN: 2476-2016CopyrightMariam Mostafa Al-Werdani1*, Abdalrhman Mostafa Mokhtar1,Ahmed Khaled Ebead1, Enas El-Sherbeny2, Abdel-Hady ElGilany212Mansoura School of Medicine, Mansoura University, Egypt.Department of Public Health, Mansoura School of Medicine, Egypt 2018 Al-Werdani et al.OPEN ACCESSKeywords Basic life support; Cardiopulmonary resuscitation;Medical education; First aidAbstractAim of the study: To measure the levels of Basic Life Support (BLS) knowledge in medical students, Mansoura University, Egypt.Methods: Our cross-sectional study was carried out in Mansoura School of Medicine, Mansoura University, Egypt. Only Egyptian medical students fromthe subject-based learning system were allowed to participate. Using a self-reported questionnaire, we measured the number of students with good BLSknowledge, attending BLS courses, self-perceived ability to handle emergency situations, previous exposure to emergency situations, and the number ofstudents wanting to learn more about BLS as a part of their curriculum.Results: With a response rate of 85%, only 5% of the participants scored 50% or more in the questionnaire. Using a cut-off point of 8 (added 1 SD tothe mean BLS knowledge score), clinical students were 2.2 times (95% CI: 1.5 -3.1) more likely to achieve good BLS knowledge scores than preclinical students.Attending BLS courses, self-perceived ability to manage emergency situations, and being male were all independent predictors of good BLS knowledge scores,with adjusted Odd’s ratios of 1.7 (95% CI: 1.2-2.4), 2 (95% CI: 1.2-3.3), and 1.8 (95% CI: 1.3-2.6) respectively. Ninety-six percent of the study participantswanted to learn more about BLS as a part of their curriculum.Conclusions: Ninety-five percent of the students achieved poor BLS knowledge scores. Revisiting the BLS teaching strategies in the subject based systemis strongly encouraged. We advise medical students to take BLS courses to raise their knowledge levels.ABBREVIATIONSBLS: Basic Life Support; PS: Preclinical Students; CS: ClinicalStudentsINTRODUCTIONBasic life support (BLS) is a set of skills that are essential tothe general public, as they significantly raise the survival rateof emergency patients, especially those suffering from cardiacarrest, stroke and foreign body airway obstruction [1]. This is dueto their efficiency in increasing survival following out of hospitalcardiac arrest until expert medical help arrives [2,3].In the East Mediterranean Region (EMR), ischemic heartdisease is the leading cause of death causing 20.3% of totalmortalities in the EMR, while deaths from road traffic accidentsattribute to 3.1% of total mortality (across all age groups in bothsexes), further emphasizing the importance of BLS in savingthose lives [4,5]. Immediate Cardiopulmonary Resuscitation(CPR) is highly recommended and considered as the most usefulpreventive measure against cerebral injury after sudden cardiacarrest [6], so the recent guidelines of the European ResuscitationCouncil (ERC) highlight the critical role of bystander CPR inincreasing survival rate of patients with sudden cardiac arrest[7], which makes BLS knowledge and training essential for thepublic, not just for the medical personnel who are expected toperform BLS skills perfectly. Unfortunately, the literature showsprevalent poor BLS knowledge among medical students andjunior doctors [8–14], which indicates a defect in BLS teaching inthe current medical education systems.In Egypt, Mansoura School of Medicine has two teachingsystems: subject-based and problem based, with the subjectbased being the main one. It consists of three Pre-clinical years(students are taught academic subjects), 3 clinical years (clinicalsubjects), and one year of internship. BLS teaching is distributedthroughout the clinical years not as a separate subject but as partof other departments’ curricula i.e. Pediatrics, Toxicology andInternal medicine. Students are also introduced to some minoraspects of BLS in their preclinical years.To the best of the authors’ knowledge, there are scarcedata about BLS knowledge of medical students in Egypt. Thisprompted us to study the BLS knowledge of Egyptian medicalstudents and its associated factors, comparing the knowledgeof Clinical students (CS) to their preclinical peers (PreclinicalStudents: PS).Cite this article: Al-Werdani MM, Mokhtar AM, Ebead AK, El-Sherbeny E, El-Gilany AH (2018) Basic Life Support Knowledge of Medical Students: A SingleFaculty Study in Egypt. Arch Emerg Med Crit Care 3(2): 1044.
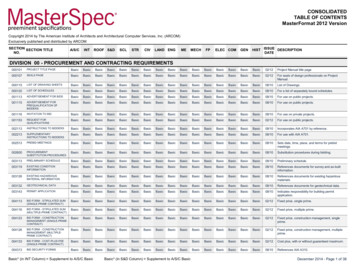
Al-Werdani et al. (2018)Email: Mariam.mostafat@gmail.com Central Bringing Excellence in Open AccessMETHODSLocation and duration: This study was conducted amongmedical students of Mansoura University, Mansoura, Al Dakahlia,Egypt from December 2017 to February 2018.Study design: a cross sectional study followed by acomparative study.Sample size and inclusion criteria: According to thedepartment of students’ affairs, the total number of students inMansoura medical school in 2016 was 6783 students: 3481 in thepreclinical years and 3302 in the clinical years. The sample sizewas calculated using epi info program assuming that the expectedfrequency of BLS knowledge is 50% the least required samplesize was 364 this was multiplied by two to compensate for thedesign effect of the cluster sampling method. The students wereselected through stratified cluster sampling with proportionalallocation. Participants had to be Egyptian students studying atthe subject-based system.We recruited students from the subjectbased system due to the following:1. The other system’s students were inaccessible to us.(main reason)2. Students from the Problem Based System (PBL) receivequality education, and a threemonth-emergency medicinecourse.3.Subject-based system is the main system in the school.4. Subject-based system students are more likely to continueworking in Egypt.Data collection: ethical approval was obtained from theInstitutional Review Board (IRB) of Mansoura faculty of medicine.During class time, data were collected using an anonymousself-administered structured questionnaire in English. Aninformed written consent was obtained from all students beforeparticipation; the collector informed them about aim of study andthat all collected data will be confidentially used for the purposeof this research only. The questionnaire was structured afterextensive literature review to collect relevant data. It was usedpreviously to assess BLS knowledge among Indian students [9].We modified the order of questions to start with theoretical thenclinical knowledge. The key answers of the questionnaire weremodified based on the opinion of public health and emergencyexperts. (S1,2)The structured questionnaire consisted of 3 parts:--Part onehad questions about the following variables:Taking previous BLS training courses, the students’ selfperceived ability to manage emergency situations andtheir willingness to learn more about BLS as part of thecurriculum.Part two consisted of 11 questions to assess BLStheoretical knowledge.Thesecovered the followingaspects of BLS:1- The abbreviation of BLS, AED (Automated ExternalDefibrillator) and EMS (Emergency Medical Service).2- Sequential steps of BLS (Checking for airway,Arch Emerg Med Crit Care 3(2): 1044 (2018)breathing, circulation) in unresponsive victims andtechniques of removing foreign body in chokingemergencies.3- CPR Techniques in different age groups.-Part three consisted of 9 questions structured to simulatereal life emergency situations.Statistical analysis: after excluding the incomplete responseforms, the data were analyzed on 664 responders with a responserate of 85%. The results were analyzed using key answers basedon the recent guidelines of the ERC [15].The data were statistically analyzed using Statistical Packagefor Social Sciences program (SPSS v24) – IBM company, NewYork, United States. Each question was scored (0, 1) with 1 for acorrect answer and 0 for an incorrect answer. We used a cut offvalue (mean BLS knowledge 1 SD 8) to divide the students into2 groups of good and poor BLS knowledge. We decided to use 8as a cut-off point to facilitate better comparisons across the studyparticipants (since the BLS knowledge scores were abysmallylow). There was no gold standard approach available to theauthors to study BLS knowledge and determine the optimum cutoff point for the questionnaire.Multivariate logistic regression analyses were used to identifyindependent variables associated with good BLS knowledge.Adjust Odds ratio at 95% confidence interval was calculated. Eachitem of the questionnaire was compared between preclinicaland clinical students using Pearson’s chi square test. The totalscore was then compared across the participant characteristicsusing the Independent sample t-test. P value less than 0.05 wasconsidered statistically significant.RESULTSA total of 662 students participated in the study, ofwhom383 were PS, and 279 were CS. Only five percent of thestudents scored more than 50% in the questionnaire. Table (1)describes the percentage of students achieving good knowledgescores in each study group. We encountered some significantgender differences, with a significantly higher percentage ofmale students achieving good knowledge scores. There was nosignificant difference between students who have been throughemergency situations compared to those who have not.In addition, a logistic regression was performed to ascertainthe effects of Academic year, Sex, BLS training course and Selfperceived ability to manage emergency situation (Table 2). Thelogistic regression model was statistically significant, χ2 16.8, p 0.0005, explaining 21.0% (Nagelkerke R2) of the variance in BLSknowledge, and correctly classified 69.3% of cases. CS were 2.2times more likely to have good BLS knowledge than PS. AttendingBLS training courses, thinking they can manage emergencysituations, and being male were independent predictors of goodBLS knowledge.Table (3) shows the 20-item-questionnaire, scanning forsignificant differences between the answers of PS and CS.Interestingly, PS performed significantly better in questions3 and 7, which asked about the location of chest compressionsin infants and their depth in children over one year while CS2/7
Al-Werdani et al. (2018)Email: Mariam.mostafat@gmail.com Central Bringing Excellence in Open AccessTable 1: Good BLS knowledge and its associated factors % in the Good knowledge column represents the % of students in the Total column with goodBLS knowledge while the % in the Total column represents the % of students out of the total number of participants(662).Total (662)Good knowledge (225)VariableX2P valueN (%)N (%)SexMaleFemale209 (31.6)90 (43.1)Attending BLS training course135 (29.8)Yes246 (37.2)Academic year416 (62.8)112 (45.5)Preclinical383 (57.9)101 (26.4)NoClinical453 (68.4)Exposure to emergency situation124 (44.4)Yes80 (38.5)No279 (42.1)113 (27.2)208 (31.4)454 (68.6)145 (31.9)Self-percieved ability to manage emergency situationsYesNo88 (13.3)574 (86.7)46 (52.3)179 (31.2)Students wanting to learn more about BLS as a part of their curriculumYesNo641 (96.8)21 (3.2)215 (33.5)10 (47.6)Table 2: Multivariate logistic regression of independent predictors of good BLS knowledge.PredictorβP value11.20.00123.2 0.00123.5 0.0012.70.115.1 0.0011.70.18AOR (95% CI)Academic yearClinicalPre-clinical0.79----Self-perceived ability to manage emergency situationsYesNo0.7Sex----Male0.62FemaleBLS training course---Yes0.54No----Constant % predicted 69.3%, Model c2 16.8, P 0.005 0.0010.0040.0010.0032.2(1.5 -3.1)r2 (1.2 -3.3)r1.8(1.3 – 2.6)r1.7 (1.2 –2.4)RTable 3: comparisons between clinical and preclinical students regarding items and total score of BLS knowledge.Question - no. (%)Preclinical(383)N (%)Clinical (279)N (%)P valueWhat Does "BLS" stand for?243 (63.4)238 (85.3) 0.001What is the location for chest compression in infant?102 (26.6)50 (17.9)0.009What is the location for chest compression?Depth of compression in adults during CPR.Depth of the compression in children over 1 year during CPR.Depth of compression in infant during CPR.Arch Emerg Med Crit Care 3(2): 1044 (2018)157 (41)149 (38.9)48 (12.5)45 (11.7)124 (44.4)105 (37.6)20 (7.2)16 (5.7)0.380.740.030.083/7
Al-Werdani et al. (2018)Email: Mariam.mostafat@gmail.com Central Bringing Excellence in Open AccessRate of chest compression in adult and children during CPR.96 (25.1)106 (38) 0.001In pediatric, compression ventilation ratio of CPR (If single rescuer).80 (20.9)66 (23.7)0.4In adult, compression ventilation ratio of CPR (If single rescuer).137 (35.8)What does "AED" stand for?What does "EMS" stand for?When you find someone unresponsive in the middle of the road, what will be your firstresponse? (Note: You are alone there).If you confirm somebody is not responding to you even after shaking and shouting at him,what will be your immediate action?How do you give rescue breathing in infants?If you and your friend are having food in a canteen and suddenly your friend starts expressingsymptoms of choking, what will be your first response?You are witnessing an infant who suddenly started choking while he was playing with the toy,you have confirmed that he is unable to cry (or) cough, what will be your first response.You are witnessing an adult unresponsive victim who has been submerged in fresh water andjust removed from it. He has spontaneous breathing, but he is unresponsive. What is the firststep?You noticed that your colleague has suddenly developed slurring of speech and weakness ofright upper limb. Which one of the following can be done?A 50-year-old gentleman with retrosternal chest discomfort, profuse sweating and vomiting.What is next?If you do not want to give mouth-to-mouth CPR the following can be done EXCEPT?Mean Score S.D.%: the percentage of correct answers out of the total number of preclinical/clinical studentsperformed in questions number 11-20 which were designed tosimulate real life situations.DISCUSSIONTo our disappointment, only 5% of the participants scoredmore than 50% in the questionnaire. This goes in line with otherstudies performed on medical students in the literature, whichshowed slightly better levels of good knowledge of 17%, and 19%in Pakistan and Netherlands respectively [9,12].Surprisingly, however, males scored significantly betterthan their female counterparts. Being male was even consideredan independent predictor of BLS knowledge according to ourregression model. This goes against previous literature thatstudied BLS knowledge in medical students or even in juniordoctors [11,14]. The gender inequality index (GII) in Egypt, SaudiArabia, and Pakistan during the time of our and the referencedstudies were 0.449 (2017), 0.234 (2017), and 0.575 (2010) [16].This suggests that the male female differences in BLS knowledgeattainment are not explained by gender inequality since SaudiArabia, with its astonishingly low GII of 0.234, had their femalesachieve better BLS knowledge scores than males. Pakistan hadfemales achieving higher than males as well, despite their high GIIof 0.575. Egypt, being the one in between (GII: 0.449), had highermale BLS scores than females. There are a lot of uncontrolledvariables coming with this suggestion however, so more researchshould be done to delineate the effect of gender inequality on BLSknowledge attainment across countries.Attending BLS courses significantly increased the numberof students with good knowledge scores, our regression modelshowed that it even works as an independent predictor of BLSknowledge. This is consistent with the literature; a previousArch Emerg Med Crit Care 3(2): 1044 (2018)51 (13.3)172 (44.9)152 (39.7)206 (53.8)86 (22.5)101 (26.4)50 (13.1)62 (16.2)91 (23.8)101 (26.4)168 (43.9)5.9 2.5134 (48)28 (10)162 (58.1)166 (59.5)180 (64.5)112 (40.1)101 (36.2)71 (25.4)58 (20.8)92 (33)73 (26.2)121 (43.4)7.25 2.50.0020.20.001 0.0010.006 0.0010.007 0.0010.130.0090.950.9 0.001study found an association between good first aid knowledgeand taking first aid courses, especially formal ones [14]. Anothercomparative study showed better BLS knowledge scores amongformally trained versus untrained medical students [17]. Somestudies, however, showed that there is no significant relationbetween previous training and good BLS knowledge [8,13].This difference in results might be due to the confounding effectof the time spent after training without rehearsal. Avisar et al.showed that retention of CPR skills goes down significantly whencomparing a 1-year-post-training group to a 2-year-post-trainingone [18]. That goes to show that the continuous rehearsal of BLSskills is quite important.Stating the obvious, there was a significant difference in BLSknowledge scores between CS and PS. This goes in accordancewith CS receiving BLS courses as part of their curriculum as wellas having better clinical awareness overall. Similarly, previousstudies revealed better BLS knowledge among senior medicalstudents [13,19]. PS showed significantly higher scores onquestions 4 and 7, which asked about chest compression locationand depth in infants, despite not taking any pediatric roundswhatsoever. This could be attributed to self-interests of studentsor extra-curricular activities related to pediatrics. Moreover,CS scored significantly better in questions 12-20, which weredesigned to simulate real life situations. This goes to show thatCS have developed realistic clinical awareness compared to theirpreclinical peers.Our findings showed no significant association between goodBLS knowledge and previous exposure to emergency situations.However, self-perceived ability to manage emergency situationswas significant in both the association with good BLS knowledge,and the regression model. One possible explanation of this is4/7
Al-Werdani et al. (2018)Email: Mariam.mostafat@gmail.com Central Bringing Excellence in Open Accessthe confounding effect of whether the student was prepared ornot when facing emergency situations i.e.: If the student wasnot prepared with good knowledge and skills, the emergencysituation may have traumatized the student, which affected his/her self-confidence. This explanation ties in with the findingsof a previous study conducted in France that found a positiveassociation between the number of exposure to cardiac arrestevents and self-confidence regarding BLS skills [20].In this study, 96% of students said they need to know moreabout BLS, and stated their willingness to learn more about it aspart of their curriculum. This falls in line with many studies inthe literature, including a study conducted on American studentswhere 64.2% thought that BLS should be included in theircurriculum [8,14,21].As for the limitations of this study, we only assessed thetheoretical BLS knowledge using a self-reported questionnaire.We did not assess the practical BLS knowledge. Another generallimitation of all self-reporting studies is the dependence onself-perception and lack of objectivity. In this study, suchvariables include self-perceived ability to manage emergencysituations, and the previous exposure to emergency situations. Additionally, this was a single faculty study, so its findings cannotbe generalized to other medical schools all over Egypt.CONCLUSIONOverall, students showed poor levels of BLS knowledge asseen in only 5% of them scoring over 50% in the questionnaire.This sheds the light on the need to revisit the currently followedteaching strategies in the subject based system. One strategywould be to add emergency department rounds to the curriculum,supported by continuous practice to achieve non-plummetingBLS knowledge and skill levels [22].ACKNOWLEDGEMENTSThis study was done as a part of the research division activitiesof Mansoura Students’ Scientific Association (MSSA), a memberin International Federation of Medical Students’ Association Egypt (IFMSA-Egypt). MSSA supported the study by helping withdata collection and entry (providing manpower, and materials).We thank Dr. Yasmeen Taalab for the useful discussions,and her expert opinion on the questionnaire items as one of theEuropean Resuscitation Council directors in Egypt.We also thank the following MSSA members for their effort indata collection and their support:HasnaaKeshk, Mohamed A. Basal, Ahmed Magdy, MaiSherif,MohamedElbaz, MarwaRaafat, Ahmed El-Shaer, SarahMisbah, Mustafa Naser, Amany Abdel Naeem, M. Magdi, EsraaSaleh, Amira Ahmed Mowannes, Khaled Mohamed Alaasr,Omnia Ahmed Elmahdy, SamaAmgadEleraki, MahmoudSamyAgeez, Abdelhamid, EsraaEmadMaghrabia, Shehab Ashraf,AbdelRahmanAmgadEleraki, Louay Nasr, Marwan Elsheikh,Noaman Mohamed NoamanHigazy, Nada MoustafaBedair,Mohamed Ahmed Sharaf El-Din, Mai Ali Mohammed.REFERENCES1. 2005 American Heart Association Guidelines for CardiopulmonaryArch Emerg Med Crit Care 3(2): 1044 (2018)Resuscitation and Emergency CardiovascularIntroduction. Circulation. 2005; 112(22 SUPPL.).Care.Part1:2. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, ChristensenEF, et al. Association of national initiatives to improve cardiac arrestmanagement with rates of bystander intervention and patient survivalafter out-of-hospital cardiac arrest. Jama. 2013; 310: 1377-1384.3. Pollack R, Brown S, Rea T, Aufderheide T, Barbic D,Buick JE, et al.Impactof Bystander Automated External Defibrillator Use on Survival andFunctional Outcomes in Shockable Observed Public Cardiac Arrests.Circulation. 2018; 137: 2104-2113.4.World Health Organization. WORLD HEALTH STATISTICS MONITORING HEALTH FOR THE SDGs. World Heal Organ 2016:1.121.5. Summary tables of mortality estimates by cause, age and sex, globallyand by region, 2000–2016. WHO.6. Kragholm K, Wissenberg M, Mortensen RN, Hansen SM, Malta HansenC, Thorsteinsson K, et al. Bystander Efforts and 1-Year Outcomes inOut-of-Hospital Cardiac Arrest. N Engl J Med. 2017; 376: 1737–1747.7. Perkins GD, Soar J, Monsieurs KG, Nolan J. Guidelines 2017 update :response to, In mountain and rural areas all CPR providers shouldperform chest compressions and rescue breaths for patients in cardiacarrest: Pharmacotherapy during cardiac arrest-When evidence-baseddata failed to be implemente. Resuscitation 2018; 0.8. Joseph N, Kumar GS, Babu YPR, Nelliyanil M, Bhaskaran U. Knowledgeof First Aid Skills Among Students of a Medical College in MangaloreCity of South India. Ann Med Health Sci Res. 2014; 4: 162–166.9. Chandrasekaran S, Kumar S, Bhat S, Saravanakumar, Shabbir M,Chandrasekaran V. Awareness of basic life support among medical,dental, nursing students and doctors. Indian J Anaesth. 2010; 54: 121.10. Reddy S, Doshi D, Reddy P, Kulkarni S, Reddy S. Awareness of BasicLife Support Among Staff and Students in a Dental School. J ContempDent Pract J Contemp Dent Pr 2013;1414:511–517.11. Al-Shamiri HM, Al-Maweri SA, Shugaa-Addin B, Alaizari NA, HunaishA. Awareness of basic life support among Saudi dental students andinterns. Eur J Dent 2017;11: 521–525.12. Tan ECTH, Severien I, Metz JCM, Berden HJJM, Biert J. First aid andbasic life support of junior doctors: A prospective study in Nijmegen,the Netherlands. Med Teach 2006;28:189–192.13. Mejia CR, Quezada-Osoria C, Moras-Ventocilla C, Quinto-Porras K,Ascencios-Oyarce C. Nivel de conocimientos sobre emergenciasm?dicas en estudiantes de medicina de universidades peruanas. RevPeru Med Exp Salud Publica 2011;28:202–209.14. Khan A, Shaikh S, Shuaib F, Sattar A, Samani SA, Shabbir Q, et al.Knowledge attitude and practices of undergraduate studentsregarding first aid measures. J Pak Med Assoc 2010;60:68–72.15. Perkins GD, Handley AJ, Koster RW, Castrén M, Smyth MA, OlasveengenT,et al. European Resuscitation Council Guidelines for Resuscitation2015: Section 2. Adult basic life support and automated externaldefibrillation. Resuscitation. 2015 Oct 1;95:81-99.16. Human Development Reports (1990-2017) by the United NationsDevelopment Programme.17. Abbas A, Bukhari SI, Ahmad F. Knowledge of first aid and basic lifesupport amongst medical students: a comparison between trainedand un-trained students. J Pak Med Assoc 2011;61:613–616.18. Avisar L, Shiyovich A, Aharonson-Daniel L, Nesher L. Cardiopulmonaryresuscitation skills retention and self-confidence of preclinical medicalstudents. Isr Med Assoc J 2013;15:622–627.19. Weller J, Robinson B, Larsen P, Caldwell C. Simulation-based training5/7
Al-Werdani et al. (2018)Email: Mariam.mostafat@gmail.com Central Bringing Excellence in Open Accessto improve acute care skills in medical undergraduates. N Z Med J2004;117:U1119.20. Freund Y, Duchateau F-X, Baker EC, Goulet H, Carreira S, Schmidt M, etal. Self-perception of knowledge and confidence in performing basiclife support among medical students. Eur J Emerg Med 2013;20:193–196.Arch Emerg Med Crit Care 3(2): 1044 (2018)21. Pillow MT, Stader D, Nguyen M, Cao D, McArthur R, Hoxhaj S.Perceptions of basic, advanced, and pediatric life support training in aunited states medical school. J Emerg Med 2014;46:695–700.22. Jurgens CY, Goodlin S, Dolansky M, Ahmed A, Fonarow GC, Boxer R, etal. Heart Failure Management in Skilled Nursing Facilities: A ScientificStatement from the American Heart Association and the Heart FailureSociety of America. vol. 8. 2015.6/7
Al-Werdani et al. (2018)Email: Mariam.mostafat@gmail.com Central Bringing Excellence in Open AccessCite this articleAl-Werdani MM, Mokhtar AM, Ebead AK, El-Sherbeny E, El-Gilany AH (2018) Basic Life Support Knowledge of Medical Students: A Single Faculty Study in Egypt.Arch Emerg Med Crit Care 3(2): 1044.Arch Emerg Med Crit Care 3(2): 1044 (2018)7/7
Faculty Study in Egypt. Arch Emerg Med Crit Care 3(2): 1044. *Corresponding author Mariam Mostafa Al-Werdani, Mansoura School of medicine, Mansoura University, AlGomhoria St., Mansoura, Al Daqahlia, Egypt, Tel: 201019044121, Email: Submitted: 23 September 2018 Accepted: 12 November 2018