Transcription
The Contamination ControlPlan in Facility ValidationScott SuttonABSTRACT(2). As an indication, the word "contamination" or itsvariants appears no fewer than 24 times in 21 CPR 211.One of the most frequent causes of drug recalls, lack ofsterility assurance, relates directly to the inability of themanufacturer to document adequate protection againstcontamination by adventitious bioburden (see ref. 3 fora historical review and ref. 4 for a biotech case study).The validation master plan (VMP) should includea clear description of the contamination controlplan and how not only the control mechanisms (i.e.,cleaning, sanitization, and sporicidal treatment) butalso the monitoring programs (i.e., environmentalmonitoring, water, gas, and process) contribute tomaintaining and monitoring the state of control forthe facility.Historically, diverse markets such as pharmaceuticals, medical devices, diagnostics, and personal careproducts have operated under different CGMPs. However, the considerations for contamination control aresimilar and can be approached from the perspectiveof root cause analysis (4). This type of "cause-andeffect" diagram can be an excellent tool in the determination of likely routes of contamination after thefact during an investigation. It can also be used as aproactive learning tool for the development of thecontamination control plan (see Figure 1). For thosemore comfortable with Six Sigma procedures, this canbe revisited as an Ishikawa diagram (Figure 2) . Themain point here is to identify, and come to agreement,on the likely causes of potential problems.Another proactive approach in risk managementthat is widely used to good effect is the use of failurerisk mode evaluation analysis (FMEA), which can beextremely useful in determining the most importantaspects of control for your process (6).The contamination control plan is central to goodmanufacturing practice (GMP) because it describesthe procedures and policies designed to create products under controlled conditions. The contaminationcontrol plan covers all phases of a facility's status and,therefore, plays a major part in the master validationplan. The author provides an overview of the contamination control plan as it applies to facility validation.INTRODUCTIONDevelopment of a contamination control plan is critical to the success of aseptic, terminal sterilization,and non-sterile manufacturing facilities . This is mostobvious in the aseptic arena, where the US Food andDrug Administration has issued clear regulatory guidance on the need for control of contamination at allstages of the process (1). What is less obvious is theeven greater need for a plan to address contaminationcontrol in non-sterile manufacturing. This need forcontamination control in non-sterile manufacturingonly becomes obvious after a problem has arisen,frequently a problem in contamination control thatrequires product recall. The challenge in non-sterileproduction is different from that in aseptic production. In aseptic production, the intention is to excludeall microorganisms from the finished product. Innon-sterile production, the intention is to control thetypes and numbers of microorganisms in the finishedproducts. Recent regulatory action has extended thisconsideration even into the realm of personal careproducts (e.g., cosmetics, toiletries, and soaps).Contamination control is central to compliance; thewhole point of current good manufacturing practice(CGMP) is to produce safe and effective medicationsABOUT THE AUTHOR. he f oun der an d pnnCipa· · I consu Itanto f M 1·cro b'10 1ogy Networ k, Inc. (h ttp://b'1t. 1y/n62yF G) . He ·IS a recogScott Sutton 1stFor more. Author.mformatlon,go togxpandjvt.com/bios42. .n1zed consultant and tramer w1th emphasis 1n GMP, 1nvest1gat1ons, environmental mon1tonng, and contam 1nat1on control[as well as microbiology laboratory audits and operations . He may be reached by e-mail at scott.sutton@microb iol.org orby phone at 1.585.594.8273.jOURNAL OF VALIDATION TECHNOLOGY[SPRING 2012]ivthome.com
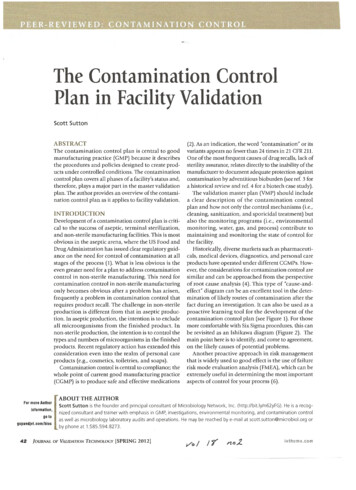
11Figure 1: Example fishbone" diagram for contaminated product.Cause & Effect Diagram for Potential Causes ofContaminated ProductProficiencyNot ReviewedRegularly\ ----L'----,.,.--- . - Operato;:ali : ectivelyRaw Material/ComponentsContaminated on SamplingRaw Material/ComponentsContaminated on StorageInadequate PPE(foot, coat, face, hair)Training Programnot in place:L -r- .:!L . - ;! ----:-.1Contaminated Product ISampling Hold CompromisedInappropriate Materials ofConstruction (difficult to sanitize,particulate generation, etcAir QualityCompromisedInadequatePest ControlIneffective/Sanitization AgentsIncompatibility misedProduct ContactSurfacesThese programs, and the protocols governing theoverall contamination control program, are essentialin documenting the rationale and methods used toaccomplish three tasks: minimizing the bioburdenthroughout the manufacturing processes; minimizingthe level of batch residual crossover contamination;minimizing the level of cleaning material residualcontamination.Phases of Manufacturing OperationThe contamination control plan must take intoaccount different stages of facility operational status.At a minimum, these will include: Commissioning and initial startup Ongoing operations Shutdown for regular maintenance Startup after scheduled shutdown.These phases will not have the same level of PONENTS OF A STRONGCONTAMINATION CONTROL PLAN 'Contamination ofCleaning, - - - - - - ' - - - - - - - - - , ImplementsOther Water Issues Standing Water Dripping Pipes/1 --"'--.::-----""'---Shift of EnvironmentalBioburden fromSensitive toResistant Specieslot-to-lot Cleaning Ineffective Carry-Over Residuals BioburdenNon-Product ContactSurfacesPiping Issues(dead-legs, reverseinclines, etc)Sampling ErrorInadequate Removalof Visible Debris,Organic loadTransfer/SamplingIssuesHold times not validated(process as well asequipment cleanand dirty holds)Inadequate Separationof "Clean" and"Dirty" OperationsInadequate ProtectionFrom UncontrolledEnvironmenttamination control. A good plan will discuss the concerns specific to each of these phases.Validated M ethodsAll measures ofbioburden in a facility will be indirect.Bacterial cells cannot be counted on a surface or in theair. The microorganisms must be transferred to an agarplate (or some other mechanism) and colony formingunits (CFUs) counted. If the assumption is made thatthe transfer of microorganisms from the air or from asurface to agar is consistent, then these numbers can beused to estimate trends over time. This assumes that thenutrient agar is capable of growing the microorganismsto visible colonies. As residual disinfectant on a surfacemay impede the growth of microorganisms, neutralizersare frequently incorporated into the growth media (i.e.,Dey-Engley Agar, Microbial Content Test Agar -MCTA,etc.). The contamination control plan should describethe sampling methods used, and how these methodsare to be validated for the conditions of use (7)./OURNAL OF VALIDATION TECHNOLOGY[SPRING 2012]43
Figure 2: Example Ishikawa diagram for contaminated product.Cause & Effect Diagram for Potential Causes ofContaminated Product"6M"Raw Material/ComponentsReceived Contaminated .,Inadequate handsanitizationNo Evidenceof TrainingPoor Personal Hygiene/(piercings, jewelry, - .- L -----.,.- --makeup, illness)Raw Material/ComponentsContaminated on SamplingRaw Material/ComponentsContaminated on StorageLack of AirQuality Control IHVAC-HEPA CompromisedOperatorsIneffectivelyTrainedTraining Programnot in placeInadequate PPE(foot, coat, face, hair)Inappropriate Materials ofConstruction (difficult to sanitize,particulate generation, etcAir QualityCompromisedProficiencyNot ReviewedRegularlyInadequatePest ControlCompressedGasesCompromisedIncompatibility ofCleaning-SanitizationAgentsProduct ContactSurfacesShift of EnvironmentalBioburden fromSensitive toResistant Species""'Lot-to-Lot Cleaning Ineffective Carry-Over""\. Residua ls BioburdenNon-Product ContactSurfacesOther Water Issues Standing Water Dripping PipesManagementThe facility should be disinfected regularly usingvalidated sanitizers and sporicides. The contamination control plan should describe the methods fortesting and rationale for acceptance of materials tobe used in the ongoing program of disinfection. Theplan should ideally describe the in vitro or laboratory tests to evaluate the sanitizers, including theidentification of the most resistant microorganismsfound in the facility as well as the most difficult-todisinfect materials in the facility. This is also wherethe method for on-going evaluation of the sanitizersbased on environmental monitoring data will berecorded. The choice of disinfection regimens shouldbe reevaluated annually from data collected in theenvironmental monitoring program to determine thecontinued efficacy of the regimens. The contamina44l ---0::.,;::-- /'--/IneffectiveSanitization AgentsWater GenerationSystem CompromisedPiping Issues(dead-legs, reverseinclines, etc)Sampling ErrorInadequate Removalof Visible Debris,Organic Load]OURNAL OF VALIDATION TECHNOLOGY(SPRING 2012],.Hold times not validated----(process as well asequipment cleanand dirty holds)'Contamination ofCleaningImplementsTransfer/SamplingIssues Inadequate Separationof "Clean" and"Dirty" OperationsInadequate ProtectionFrom UncontrolledEnvironmenttion control plan should describe how this evaluationshould occur.It is also critical to have appropriate microbiological methods for the relevant specifications-platecounts less than 20 CPU are notoriously unreliable.Traditionally the "countable range" for a standardsized petri dish is 25-250 (or 30-300) CPU/plate. Theselower limits (limits of quantification) are routinelyignored when setting product and environmentalspecifications, sacrificing accuracy and precision.Similarly, the upper limit (250 or 300 CPU/plate)are set for particular microorganisms on standardsized plates, smaller plates, or organisms that producelarger colonies will have lower numbers as there upperlimit, requiring dilutions as appropriate to measurethe same specification.ivthome.com
Know the EnemyA successful contamination control plan is gearedto providing the most useful information on themicroorganisms present while at the same time showing fiscal responsibility. The FDA aseptic processingguidance document recommends genetic identification of all organisms isolated from the manufacturing environment on a regular basis (1) . This isa laudable goal, but few of us have anything nearthe required budget to accomplish this task, and inall honesty, it is reasonable to wonder if it is reallynecessary. The numbers of CFU from validated sites(i.e., viable air and surface, non-viable) is sufficientto provide a measure of the state of control of thefacility. However, periodic cataloging of the residentmicroflora (at least to the species level) will providea good check on the continued effectiveness of thedisinfectants in use and is recommended in the FDAaseptic processing guidance document (8). Shifts ofbioburden to spore forming microorganisms will bestrong evidence of the need for use of a sporicidalagent. Occasionally, this effort will also pick upshifts among non-spore-forming organisms-thisis not due to "resistance" but rather ecological shiftstowards species more naturally resistant to the disinfectant in use.The considerations in the non-sterile facility aresimilar, as there needs to be proof that the sanitization program used is effective and the regular use ofsporicidal agents are appropriate. The contamination control plan must address how the sanitizationprogram will be monitored for efficacy.Control Incoming BioburdenThe first step in any control program is to controlcontamination at the very beginning of the process.This includes raw materials (e.g., excipients, activepharmaceutical ingredient [API], and water) and theprimary containers. All materials should be tested forincoming bioburden against documented acceptancecriteria. Part of the incoming bioburden will also beany water used as an excipient to the process . TheGMP guidelines for pharmaceuticals, biologics, medical devices, and diagnostics all provide instructionon this point.Appropriate GowningThe gowning methods and materials are of criticalimportance to minimization of contamination. Theprimary source of contamination in most controlledareas will be the personnel, and the contaminationgxpandjvt.comcontrol plan must address personnel barriers tocontamination whether the manufacturing processis designed for aseptic or non-sterile manufacturing facilities. All personnel should be well trainedin appropriate gowning practice and behavior. Thecontamination control plan should describe therationale for the level of gowning chosen, the frequency of gown cleaning, behavior of the operatorsin the controlled rooms, and the acceptable gownmaterials for the type of manufacturing process.This discussion will, of course, be different betweencontamination control plans among different typesof aseptic, terminal sterilization, and non-sterilemanufacturing facilities.TrainingOperator training is critical to contamination control.No supervisor can be present at all locations and at alltimes . Each operator must be aware of his or her rolein contamination control and how to minimize therisk to batch integrity. Minimal skill sets in relation toproduct protection and sampling should be describedby job function in the contamination control plan.This is most effectively accomplished using a welldesigned and enforced standard operating procedure(SOP) system (9).Controlled EnvironmentsControl and monitoring of the environment isanother critical element of the contamination control plan. Large portions of this can be addressedby the corporate environmental monitoring (EM)master plan, which provides rationale and consistency for a single EM philosophy across thedifferent facilities of the corporation, or the siteenvironmental master plan (EMP), which providesconsistency and detailed instruction for the variousmanufacturing buildings at a given site. However,the contamination control plan should cite therelevant documents and their role in contamination control.The appropriate EMP for non-sterile manufacturesand for API manufacturers is not well defined froma regulatory sense. There are no strong recommendations such as those seen for the environmentalmonitoring of aseptic facilities; however, the absenceof regulatory guidance is not the same thing as theabsence of need for the activity. EM is useful for determining the state of control of the facility and so isan important part of the monitoring program for allmanufacturers (7).]OURNAL OF VALIDATION TECHNOLOGY[SPRING 2012}45
Validated Sanitizationand Sporicidal ProceduresThe efficacy of the sanitizers and sporicides usedin the program must be demonstrated in a studydesigned to test their efficacy on the materials ofconstruction and against resident microorganismsfound in the facilities governed by the contamination control plan. This can be done optimally in thefollowing four-step process: Suspension test of efficacy. This is a screeningeffort using the candidate agents against labstrains of indicator organisms as well as a variety of the microorganism species found in thefacility. The goal of this assay is to determinethe "most resistant" microorganism(s) for thenext step. Coupon study. Using the representative organisms (e.g., gram positive, gram negative, sporeformer, yeast and mold) and organism(s)identified in the previous study, test the efficacy of the sanitizing agents on coupons ofmaterials found in the facility. The purposeof this test is to demonstrate efficacy on thesematerials using the appropriate applicationprocedures. "Mock" sanitization study. This study providesreal-world evidence of efficacy. Let a representative room go untouched for a period of time tobecome "contaminated." Take bioburden samplesthroughout the room, then sanitize the surfacesand repeat the bioburden sampling. The samplestaken after cleaning should be far less contaminated than the first set. Confirm efficacy from environmental monitoring. The final step in validating the sanitizationprogram will be ongoing evidence that the program allows the facility to operate in a state ofcontrol.The sanitization program will ideally consist ofa qualified disinfectant and sanitizing agent, usedappropriately (concentration and contact dwell timeobserved) as the primary agent. This will then beperiodically rotated with the use of a sporicidal agent(also validated for effectiveness) (10, 11).Well-Defined and UnderstoodManufacturing ProcessesThe manufacturing process should be evaluatedfor its potential to limit or eliminate bioburden .The two common methods for performing thisis either a hazard analysis, critical control point46]OURNAL OF VALIDATION TECHNOLOGY[SPRING 2012)(HACCP)-type or a FMEA approach. The use oforganic solvents, heat, or other inhospitable activities can greatly reduce bioburden of a process. Thecontribution of compression (and associated shear),for example, should be evaluated for a potentialreduction in risk of excessive microbial contamination, the contribution of the finished productwater activity should also contribute to this analysis. Process bioburden reduction steps should befactored into the contamination control plan on aprocess-by-process basis.Of particular importance in this evaluation forthe potential for microbial contamination of theprocess are cleaning steps, equipment hold times,HVAC, control level of environments for critical tasks,open-system versus closed-system operations, andbioburden monitoring (among others specific to theprocess). As an example of the importance of the bioburden control point issue, there is a strong regulatory expectation in Europe that products sterilizedby filtration should have a pre-filtration bioburdenof not more than 10 CFU/100 mL immediately beforethe sterilizing filter (or be subjected to dual filtrationin series) (12).Finally, the contamination control plan should citethe need for clear SOPs on all aspects of manufacturing, monitoring, and control. These SOPs are criticalfor training, documentation, and batch release.Minimization of Batch ResidualCross-Over ContaminationThe contamination control plan should also addressthe potential for a batch to be contaminated by material from the previous batch manufactured using thatequipment. Obviously, the contamination controlplan should describe the methods by which this likelihood is minimized .The concern over batch residual cross-over is mostrelevant when there is more than one product manufactured at a site. This concern has little to do withthe sterility of the finished product and is relevant tosterile and non-sterile manufacturers alike.Minimization of CleaningMaterial Residual ContaminationValidation of cleaning procedures is essential todemonstrate not only that the cleaning procedureeffectively cleans and sanitizes the manufacturingequipment, but also that residual cleaning material isremoved to prevent contamination of the next batchmanufactured.ivthome.com
DANGER SIGNS INCONTAMINATION CONTROLCompliance professionals should be vigilant whencontrolling contamination in aseptic, sterile, and nonsterile manufacturing. The development of a contamination control plan, when done correctly, is beneficialin the control of contamination in manufacturing.4. Schleh, M. , et al., "Effectiveness of Upstream BarrierTechnologies for Inactivation of Adventitious Contaminants of Cell Culture," Amer Pharm Rev 13(7) :72-76,2010.5. Sartain, E. and Polarine, J., "Prevention of MicrobialContamination.," Pharm Technol. 35(6) :62-65, 2011.6. Sutton, S., "Successful Microbiological Investigations,"Amer Pharm Rev. 74(2):34-42, 2011.7. Sutton, S., "The Environmental Monitoring Program In aGMP Environment,"] GXP Compliance. 14(3):22-30, 2010.8. Sutton, S.V.W. and Cundell, A.M., "Microbial Identification in the Pharmaceutical Industry," Pharm Forum.30(5):1884-1894, 2004.9. Sutton, S., "The Importance of a Strong SOP System Inthe QC Microbiology Lab," J GXP Compliance, 14(2):44 52, 2010.10. Martinez, J., "The Rotation of Disinfectants Principle:True or False?" Pharm Technol. 33(2) :58-71, 2009 .11. Sutton, S.V.W., "Disinfectant Rotation- A Microbiolo gist's View," Controlled Environ., pp. 9-14, July 2005 .12. EMEA, CPMP/QWP/486/95 , Note for Guidance onManufacture of the Finished Dosage Form, 1996.13. Donald, T., "Vaccines Pulled Due to Potential Contamination," Contamination Control. 4(1):12- 13, 2008.14. Suvarna, K., et al., "Case Studies of Microbial Contamination in Biologic Product Manufacturing," Amer PharmRev. 14(1) :50-56, 2011 .15. Macdonald, G. Tabletting delay caused lethal allopurinol contamination, say HK chiefs . Decision News Media,2009. http://www.in-pharmatechnologist.com/content/view/ print/ 23918916. Yang, C., et al., "Nosocomial Outbreak ofTwo Strains ofBurkholderia cepacia Caused by Contaminated Heparin (Letters to the Editor)," Hosp Infect Soc. 69(4) :398-400, 2008 .17. FDA, "FDA acts to prevent contamination problemswith Triad antiseptic products," fda .gov, 2011. http://www.fda.gov/N ewsEvents/ N ewsroom/PressAnnouncements/ucm249706.htm JVTREFERENCESARTICLE ACRONYM LISTINGThe compliance professional should be vigilant in termsof contamination control-this is a sure area of regulatoryenforcement interest and one where the short-sightedmight be tempted to institute "cost-savings." Frequentmanifestations of cost savings mentality deal with validation aspects-the sanitizer and cleaning qualifications inparticular can be expensive. The temptation is real to pullback from a full program-for example, accepting withoutconfirmation bioburden information on incoming rawmaterials, assuming efficacy of sanitizers, neglectingto clean floors and other non-product contact surfaces(especially in non-sterile production) and other relativelyhigh-cost "overhead" activities. These activities are notoptional safeguards to be ignored with impunity, as several companies have come to realize as oflate (13-17).A second major area to be constantly examining isin the general topic of consistency. A well-constructedcontamination control plan will include reasons forvarious activities . For example, if facility "scrubs" arerequired in a non -sterile production, there is a reasonfor this that should be described. Requiring all operators to be in scrubs and booties is not consistent withallowing maintenance personnel to enter the area inboots, denims, and flannel shirt for a "quick signatureon a work order." Likewise, requiring shoe covers (booties) to protect against tracking soil organisms throughthe facility is not effective if operators fail to change thebooties during the day (i.e., entering, leaving, going tolunch/restroom, walking in them until they hang intatters from their ankles). Consistency is key.CONCLUSION1. FDA, Guidance for Industry: Sterile Drug Products Producedby Aseptic Processing-Current Good Manufacturing Practice, 2004.2. Oji, RT, "Regulatory Aspects Concerning the QualityControls of Microbiological and Non-viable Particulate Contamination in Pharmaceutical Manufacturing,"Amer Pharm Rev. 7(1):18,20,22,68, 2004.3. Prince, H. and Prince, D., "Contamination Control: TheLife and Death of Bacteria and Other Germs," ContractPharma. pp.2 - 7, June Active Pharmaceutical IngredientCurrent Good Manufacturing PracticeColony Forming UnitsEnvironmental MonitoringUS Food and Drug Admin istrationFailure Risk Mode Evaluation AnalysisHazard Ana lysis, Critical Control PointMicrobial Content Test Agar (Soybean CaseinDigest Agar with Lecithin)Standard Operating ProcedureJOUR NA L OF VA LIDATION TECHNOLOGY[SPRI NG 20 12)47
The contamination control plan is central to good manufacturing practice (GMP) because it describes the procedures and policies designed to create prod ucts under controlled conditions. The contamination control plan covers all phases of a facility's status and, therefore, plays a major part in the master validation plan.