Transcription
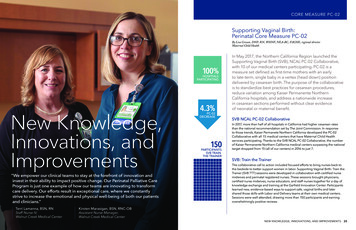
CORE MEASURE PC-02Supporting Vaginal Birth:Perinatal Core Measure PC-02By Lisa Cowan, DNP, RN, WHNP, NEA-BC, FACHE, regional directorMaternal Child Health100%HOSPITALSPARTICIPATINGNew Knowledge,Innovations, andImprovements“We empower our clinical teams to stay at the forefront of innovation andinvest in their ability to impact positive change. Our Perinatal Palliative CareProgram is just one example of how our teams are innovating to transformcare delivery. Our efforts result in exceptional care, where we constantlystrive to increase the emotional and physical well-being of both our patientsand clinicians.”Terri Lamanna, BSN, RNStaff Nurse IV,Walnut Creek Medical Center24NURSING REPORT 20184.3%PC-02DECREASE150PARTICIPANTSSVB TRAINTHE TRAINERIn May 2017, the Northern California Region launched theSupporting Vaginal Birth (SVB), NCAL PC-02 Collaborative,with 10 of our medical centers participating. PC-02 is ameasure set defined as first-time mothers with an earlyto late-term, single baby in a vertex (head down) positiondelivered by cesarean birth. The purpose of the collaborativeis to standardize best practices for cesarean procedures,reduce variation among Kaiser Permanente NorthernCalifornia hospitals, and address a nationwide increasein cesarean sections performed without clear evidenceof neonatal or maternal benefit.SVB NCAL PC-02 CollaborativeIn 2017, more than half of all hospitals in California had higher cesarean ratesthan the national recommendation set by The Joint Commission. In responseto those trends, Kaiser Permanete Northern California developed the PC-02Collaborative with all 15 medical centers that have Maternal Child Healthservices participating. Thanks to the SVB NCAL PC-02 Collaborative, the numberof Kaiser Permanente Northern California medical centers surpassing the nationaltarget dropped from 15 (all of our centers) in 2016 to just 7.SVB: Train the TrainerThe collaborative call to action included focused efforts to bring nurses back tothe bedside to better support women in labor. Supporting Vaginal Birth: Train theTrainer (SVB TTT) sessions were developed in collaboration with certified nursemidwives and perinatal registered nurses. These sessions brought physicians,certified nurse midwives, nurse educators, and staff nurses together for a day ofknowledge exchange and training at the Garfield Innovation Center. Participantslearned new, evidence-based ways to support safe, vaginal births and latershared those skills with Labor and Delivery teams at their own medical centers.Sessions were well attended, drawing more than 150 participants and earningoverwhelmingly positive reviews.Kirsten Marasigan, BSN, RNC-OBAssistant Nurse Manager,Walnut Creek Medical CenterNEW KNOWLEDGE, INNOVATIONS, AND IMPROVEMENTS25
THE FIRST 48Improving Care Coordination for Home Healthand Hospice PatientsBy Danielle W. Franklin, MSOD, PMO, project manager, San Jose Medical CenterSusan Sanfacon, MBA, BSN, RN, service director, Santa Clara Home Health & HospiceWhen Kaiser Permanente Santa ClaraHome Health and Hospice sought tostreamline their workflow, project leadersDanielle Franklin, MSOD, PMO, andSue Sanfacon, MBA, BSN, RN, launcheda highly collaborative, inquiry-drivenimprovement process. In less than oneyear, rates for start of care within 48 hoursclimbed from 64 to 91 percent — anincrease of nearly 30 percent.Katrina Cabalfin, RN, staff nurse II, San Francisco Medical Center practices a hands-on demonstrationat the Supporting Vaginal Birth event in June 2018.Rising to Meet a ChallengePositive ResultsKaiser Permanente Northern California nursing,physician, and midwifery leaders used standardperformance improvement methodology,engagement, and multidisciplinary collaboration toidentify key drivers of preventable cesarean sectionsand implement solutions to better support vaginalbirths. The initiative focused on 4 strategies:sharing of data, chart review, development andspread of protocols and checklists, and laborsupport skill-building.Since we know the first cesarean section createssignificant medical consequences for futurepregnancies, we have shifted our culture tosupporting vaginal births. As of October 2018, theNCAL Supporting Vaginal Birth PC-02 Collaborativehas affected an overall reduction of the PC-02 rateby 4.3 percent. This equates to the preventionof approximately 670 cesarean births per yearthroughout Kaiser Permanente Northern California.Cesarian Birth NTSV PC-02Strategic Focus and Methodology30%CMDC Q4Q1PC-02 NTSV C-Sections Results26In 18 monthsNCAL decreasedPC-02 rate byNURSING REPORT 2018Q22017Q3Q4Q12018670Q2Reduction inCesarean BirthsKaiser Permanente Santa Clara Home Health andHospice is a parent agency with oversight of San Jose,Redwood City, and Santa Clara home health andhospice patients. The center’s intake department isresponsible for processing referrals for all 3 sitesin preparation for start of care (SOC) appointments.For some time, Santa Clara Home Health andHospice had struggled to keep up with growingdemand for home health and hospice care needswithin its service area. The persistent challenge metits match when project manager Danielle Franklinteamed up with service director Sue Sanfacon inearly November 2017.Drawing from her expertise in organizationaldevelopment, Franklin worked with Sanfacon tolaunch an all-hands-on-deck investigation into theagency’s workflow challenges. Every step of theprocess would be examined — from the momentreferrals were received to first patient contact.Investigation and InquirySanta Clara Home Health and Hospice’s intaketo start of care is a complex, multi-step process,involving many team members, multiple roles,and 3 different sites. Franklin and Sanfacon knewa successful outcome would come from open andhonest collaboration, and input from every teammember involved in the process.Following an interactive kick-off meeting, theyinitiated 2 weeks of one-on-one interviews. The pairmet with intake nurses, intake clerks, home healthnurses, specialists, and site directors. Collectively,these ground-level professionals have an accurateview of the agency’s daily workings. As those closestto the work, they also hold the key to a successfultransformation.One-on-one interviews were followed by 2 weeks ofobservation. Workflow and work roles were carefullyreviewed. The project team noted any workaroundsthat might have developed and collaborated withteam members on what might make certain taskseasier or more efficient.It Takes a Crew to Right a ShipAfter 4 weeks of interviews, observation, andcollaboration, the team proposed some dramaticworkflow changes. First, the agency’s single referralintake funnel was split into 3 tracks. This changeaccelerated site assignment and start of care.In the new intake process, referrals were assignedimmediately to their appropriate geographic site: SanJose, Redwood City, or Santa Clara. Dedicated intakeclerks and intake RNs were assigned to each site,working side by side to process referrals and start ofcare. Metrics to identify areas for development as wellas successes also were put into place.Reception of the proposal were extremely positive.Everyone’s voice had been included and they feltinvested in the outcome. As the new processestook effect, the plan’s positive impact quicklybecame apparent.NEW KNOWLEDGE, INNOVATIONS, AND IMPROVEMENTS27
% of Patients within 48 Hours110%100%90%80%70%60%50%40%30%20%SURGICAL SITE INFECTION MarchAprilMayJuneJulyThe number of SOCs 48 hours increased from64% to 91% betweenNovember 2017and September 2018.Aug2018Number of POSOCInternal Starts of Care within 48 Hours (RWC, SCL, SJO) ov2017DecJan2018Feb March AprilMayJuneJuly 5/dayBetween November 2017and September 2018Aug2018Bundle Improves Care Outcomes in Perioperative CasesBy Tammy Peacock, DNP, RN, NEA-BC, CENP, CPPS, LSSBB, surgical outcomes improvement managerJenny Mendenhall, BSN, RN, CHSE, clinical education and nursing practice consultant, Perioperative ServicesClaire Spanbock, MSN, RN, CNOR, regional director Perioperative ServicesAccording to a 2017 study, the incidenceof surgical site infection (SSI) isapproximately 160,000–300,000 casesannually in the United States. The financialburden of these infections is substantialand one of the costliest of all hospitalacquired infections. Estimated costsvary from 3.5 to 10 billion annuallyin the U.S. Moreover, SSI instancesincrease emergency department visitsand hospital readmissions, and extendhospital stays by 9.7 days per infection.An estimated 60 percent of thesecases can be prevented with the useof evidence-based measures.Internal Number of Physician Ordered Starts of Care (RWC, SCL, SJO) c-ChartIntroduction of the SSI BundleThe Proof is in the DataThe Kaiser Permanente Northern California SurgicalSite Infection (SSI) bundle was rolled out in October2018. It was developed by an interdisciplinary teammade up of clinicians and staff which includednurses and physicians from across the region.Components of the SSI bundle include:Within one year, Santa Clara Home Health’sworkflow improvement project’s successis indisputable. Prior to kick-off, start-ofcare appointments within 48 hours wereat 64 percent. In just ten months, the rateof start-of-care within 48 hours climbedto 91 percent — a remarkable 27 percentimprovement.Franklin and Sanfacon credit their entireteam’s participation, ingenuity, and creativeproblem solving skills. Franklin adds, “Thesecret sauce to this project (and frankly anyproject) is the complete trust of the team,leaders, and sponsors. We worked togetherto find the very best outcome, focusing onpossibilities, not barriers.”28NURSING REPORT 2018“When you explain thatthe measures we take aredesigned to reduce therisk of infection, patientsfeel good about that.”— Sherri Souza, RN, staff nurse IV,Fremont Medical Center CO2 monitoring to assess CO2 levels priorto surgery Hair clipping outside the operating room,and only when needed Surgical skin prep applied in a standard,consistent manner Pre-op chlorhexidine (CHG) wipes appliedby the pre-op nurse during a skin assessment Antibiotics administered as prophylaxis(and re-administered when needed) at theappropriate dose and timing A warming device, or normothermia, applied to allpatients in pre-op, in intra-op, and to hypothermicpatients in the post-anesthesia care unit Surgical hand scrub applied in a standard,consistent mannerThe First 48 Home Health Initiative team gathered in redwoods for theproject kickoff event.NEW KNOWLEDGE, INNOVATIONS, AND IMPROVEMENTS29
morning, and George feels chilled. The nurses getGeorge ready for surgery. He is weighed, bodyhair on his hip is clipped and cleaned again withCHG wipes, and he blows into a CO2 monitor. Thenurse congratulates George on quitting smoking.He is covered with a warm, inflatable blanket, whichthe nurse explains will help prevent an infectionpost-surgery. The anesthesia provider explains thatGeorge will receive weight-based antibiotics beforethe surgery. He explains that this, too, will help withinfection prevention. When the nurse comes to takeGeorge to the operating room, he is not worriedabout Purdy. He knows he should be home with herlater that night.The SSI Bundle Is Making an ImpactMembers of the Fremont Medical Center Perioperative Services team.Meet GeorgeGeorge is not real — but his story is drawn from actualpatient experiences. His experience, featuring 2different surgical scenarios, illustrates the dramaticdifference Kaiser Permanente’s SSI bundle can make.George is 68 and lives on his own. His wife died2 years ago after a long illness. He smokes, isoverweight, and needs his right hip replaced afteryears of arthritis. George is scheduled for a total hiparthroplasty tomorrow, however, he is concerned forhis cat Purdy. George’s neighbor Steve has promisedto check in on the cat while George is in the hospital,but George remains focused on Purdy’s well-being.Scenario 1:Pre-SSI Bundle ImplementationGeorge was told not to eat or drink anything themorning of surgery, so he begins that day bysmoking an extra cigarette. George did not showerlast night or this morning, because no one has toldhim it is important to shower before surgery. Stevetakes George to the hospital, and they smoke on the30NURSING REPORT 2018way. It is blustery and cold this January morning, andGeorge feels chilled. At the hospital the nurses arecheerful but busy, and George does not ask for anextra blanket. When the nurse comes to take Georgeto the operating room, he is cold, hungry, unkempt,and worried about Purdy. George’s surgeon doesnot routinely prescribe weight-based antibiotics, andorders an insufficient dose.The SSI Bundle was tested at 2 pilot sites in June2017 and significantly improved SSI rates at thosefacilities. As a result, the bundle was shared with all21 hospitals in December 2017 and has resulted ina 22 percent decrease in SSIs in 2018. We continueto look at innovative and evidence-based practicesthat will help to continue to improve the care of ourpatients and members who receive surgical care inthe Northern California Region.“Yes, I have the tools Ineed. I used illustrationsand demonstrationsat our staff meeting tocreate awareness of thepossible causes of SSIsand likewise how easyit is to keep them fromhappening.”— Charlene Wade, RN, clinical and informaticseducator, San Jose Medical CenterSSI Pilot Start1.051.00Scenario 2:Post-SSI Bundle Implementation0.95The morning of surgery George has stoppedsmoking because he has been advised that givingup smoking, even for a short amount of time, willhelp his post-op recovery. He is concerned abouthis cat, Purdy, and wants to get home as soon aftersurgery as possible. He is told he should expectto go home the same day of surgery. George hasshowered the night before, and before dressinghe cleans his hip with the CHG wipes provided tohim by his medical team. George’s neighbor Stevetakes him to the hospital, and knows that Georgehas quit smoking, so they do not smoke. It is a cold0.90WHERE WEARE neDec2015JuneDec2016JuneDec2017KP NCAL NSQIP Risk Adjusted Odds Ratios: All Cases SSINEW KNOWLEDGE, INNOVATIONS, AND IMPROVEMENTS31
PEDIATRIC IMMUNIZATIONSImproving Immunization RatesBy Dawn Belardinelli, MD, chief of pediatrics, South San Francisco PediatricsLee Ann M Wise, MS, RN, CNL, director of pediatrics and allergy, San Rafael PediatricsErrikka Richard, LVN, licensed vocational nurse, South San Francisco PediatricsAs a national leader for childhoodimmunization delivery, The PermanenteMedical Group knows immunizationsare the cornerstone of prevention forall children. When working to increaseimmunization rates in a service areawith historically high refusal, it’simportant to look for opportunitiesthroughout the entire delivery process,and never make assumptions. Followingis one story of how a team of front-linenurses and physicians applied provenbest practices to great success.Look Past Perceived ObstaclesIn 2015, Lee Ann Wise accepted the role ofdirector of Kaiser Permanente San Rafael’sPediatric Department. She brought with hermore than 20 years of pediatric nursingexperience in an inpatient setting.At the time of Wise’s arrival, San Rafaelhad challenges meeting the HEDIS(Healthcare Effectiveness and Data andInformation Set) measure for childhoodimmunizations. HEDIS is a nationalimmunization benchmark, triple-weightedin TPMG performance measures.Immunization rates were thought to below because of Marin County’s historicallysignificant rate of immunization refusal. Wiseencouraged her team to look past externalobstacles and collaborate to find internalsolutions for improvement. As it turned out,San Rafael’s challenges had less to do with thearea’s refusal rates than previously thought.32NURSING REPORT 2018Collaborating with Leadersin Immunization RatesWise looked to pediatric departments throughoutNorthern California for inspiration. Knowing thatKaiser Permanente South San Francisco is a leader inchildhood immunization, she reached out to DawnBelardinelli, MD, chief of Pediatrics. Dr. Belardinellialso serves as Regional Immunization PerformanceImprovement Lead. Along with her team, includingErrikka Richard, LVN, Dr. Belardinelli invited Wiseand her department chief, Otto Von Franque, MD, tovisit South San Francisco for a day of TD 67%78%Errikka Richard, LVN, Lea Ann Wise, RN, and Dawn Belardinelli, MD, discuss current immunization rate performanceat the San Rafael Medical Offices.70%REGIONALTOTALTOTAL70% REGIONALTARGETYTD RATE68%2018 ChildCombo10*10*VaccinationRates2018 ChildComboVaccination Rates*National metric measuring % of children who by their 2ndbirthday have received 10 recommended vaccination dosages.From the moment they arrived, Wise and Dr. VonFranque noticed that South San Francisco’s teamhad internal systems in place contributing to theirsuccess. The department had effectively removedall internal obstacles to immunization: the injectionschedule was open to families a full year in advance,there was a consistent process for “fail to keep”immunization appointments, and families werenever turned away. Members were vaccinated inthe moment, every time.Improving What We Can ControlBack in San Rafael, obstacles were quickly removed.Wise and Dr. Von Franque followed South SanFrancisco’s lead and partnered with their LVN teamto implement the best practices they had seen inaction. “The most enlightening part of this journey,”Wise revealed, “was recognizing the opportunitiesfor process improvement that were already availableto us. Rather than referring families to upcoming fluclinics, we made vaccines available on the weekendsand offered shots immediately upon request.Success in Best PracticesImmunization rates immediately climbed as theentire San Rafael pediatric team worked togetherto mirror South San Francisco’s model. Not onlydid San Rafael’s rates dramatically improve, theyhave consistently surpassed the goal, achieving asustained change in habits that will help preventchildren from contracting a vaccine-preventableillness. Wise credits her team of front-line nurses.“Our success is 100 percent nurse-driven,” she adds.“They are completely invested in this important workand have embraced the changes, because they wereequal partners on this journey.”The partnership forged between San Rafaeland South San Francisco continues today. The2 departments are collaborating to improvepediatric immunization rates across the entireregion. Dr. Belardinelli adds, “We’re workingtogether to realize Kaiser Permanente’s visionthat no Kaiser Permanente Northern Californiachild is harmed by a preventable infection.”NEW KNOWLEDGE, INNOVATIONS, AND IMPROVEMENTS33
The Kaiser Permanente Northern California Surgical Site Infection (SSI) bundle was rolled out in October 2018. It was developed by an interdisciplinary team made up of clinicians and staff which included nurses and physicians from across the region. Components of the SSI bundle include: CO 2 monitoring to assess CO 2 levels prior to surgery