Transcription
Quality DepartmentAtrial FibrillationGuideline TeamManagement of Acute Atrial Fibrillation and AtrialFlutter in Non-Pregnant Hospitalized AdultsTeam MembersJeffrey M Rohde, MD(Team Lead)Internal MedicineSarah E Hartley, MDInternal MedicineSarah Hanigan, PharmDPharmacy ServicesJules Lin, MDThoracic SurgeryLewis B Morgenstern, MDNeurology (Stroke)F Jacob Seagull, PhDMedical EducationDavid M Somand, MDEmergency MedicineDavid H Wesorick, MDInternal MedicineJames B Froehlich MD(Consultant)CardiologyThomas C Crawford, MD(Team Lead)CardiologyInitial Release:May, 2014Last Reviewed:June, 2017Inpatient ClinicalGuidelines OversightSarah E Hartley, MDDavid H Wesorick, MDF Jacob Seagull, PhDGuidelines for Clinical CareInpatientPatient Population. Adult hospitalized patients with Atrial Fibrillation and Flutter. This guidelineexcludes pregnant women.Objectives. The purpose of these inpatient care guidelines is to provide an evidence-based blue printfor the acute care of patients with atrial fibrillation (AF) and atrial flutter (AFL) at the University ofMichigan Health System. It is hoped that this standardization of care will result in improved patientoutcomes, shorter length of hospital stay, lower readmission rates, and overall cost savings for thesystem. This document will discuss evaluation of patients with new onset and recurrent AF/AFL,including indications for admission, rate vs. rhythm control strategies, and plan of care followingpatient’s discharge.Key PointsClinical PresentationPatients presenting with palpitations, irregular pulse, chest pain, dyspnea, fatigue, lightheadedness,syncope, cardio-embolic disease and new or recurrent heart failure should be evaluated for AF/AFL.While AF may be asymptomatic and found incidentally, AFL is usually highly symptomatic.DiagnosisElectrocardiogram (ECG) is essential in the diagnosis of AF/AFL. The initial evaluation is summarizedin Table 1 and should include: Physical examLaboratory evaluation: CBC, basic metabolic profile, magnesium, thyroid-stimulating hormone,and cardiac enzymes as indicatedImaging: Chest X-ray, echocardiogramContinuous telemetry monitoring in the hospitalTreatmentInitial treatment of AF/AFL depends on hemodynamic stability:Unstable AF/AFL (Figure 1) Begin resuscitation and consider other conditions contributing to instabilityIf instability due to AF/AFL - immediate direct current cardioversionStable AF/AFL (Figure 2):For more information:734- 936-0770 Regents of theUniversity of Michigan These guidelines should not beconstrued as including allproper methods of care orexcluding other acceptablemethods of care reasonablydirected to obtaining the sameresults. The ultimate judgmentregarding any specific clinicalprocedure or treatment must bemade by the physician in lightof the circumstances presentedby the patient.For ED patients: Screen for early cardioversion in the Emergency Department (Figure 4)Administer rate controlling agents as indicated (Table 4) – [I, B]- EP consult for uncontrolled rate despite adequate trial of rate controlling agentsConsider the appropriateness of a rhythm control strategy (Table 3) – [I, B]- If rhythm control strategy is appropriate/desired, consult EP and start immediateanticoagulation (Figure 3)Consider anticoagulation based on CHA2DS2-VASc score (Table 2, Figure 3) – [I, A].- The choice of anticoagulant will depend on the patients clinical circumstances and renalfunction (Figure 3)- Obtain Neurology consult prior to initiation of anticoagulation for patients with recentischemic stroke within the prior two weeks- Patients with valvular disease and those requiring concomitant treatment with dualantiplatelet therapy should be anticoagulated with warfarin- Target-specific oral anticoagulants are preferred over warfarin in many cases* Strength of recommendation:I generally should be performed; II may be reasonable to perform; III generally should not be performed.Levels of evidence reflect the best available literature in support of an intervention or test:A randomized controlled trials; B controlled trials, no randomization; C observational trials; D opinion of expert panel.
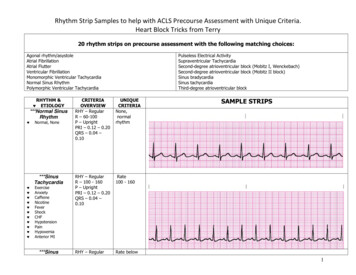
Figure 1: Acute management of UNSTABLE atrial fibrillation and atrial flutter (AF/AFL)ACS: Acute coronary syndrome; BNP: Brain natriuretic peptide; CBC: complete blood count; CCU: Cardiac Care Unit; COMP:comprehensive metabolic panel; CXR: chest radiograph; ECG: electrocardiogram; EP: electrophysiology; HR: heart rate; IV:intravenous; J: Joules; PE: Pulmonary embolism; RRT: rapid response team; SBP: systolic blood pressure; TSH: thyroidstimulating hormone; UA: urinalysis.Figure 2: Acute management of STABLE atrial fibrillation and atrial flutter with rapid ventricular response12
See Figure 2 notes on following page3
Figure 2 Notes:If BP does not tolerate these medications, see Table 4 (medications for rate control) and consider DCCV or EP/GeneralCardiology consult.Also, IV calcium channel blockers and IV beta blockers are not usually combined- if one is not effective, change to the other.2If patient spontaneously converts to normal sinus rhythm: If in the ED, provide outpatient EP follow-up within 2 weeks If inpatient, consider consulting EP in the hospital If a postoperative patient, consult General Cardiology (if AF/AFL is sustained for 24 hours) Consider a rate control agent (Table 4), depending on the pre- and post-conversion heart rate Consider the use of a 3 week event monitor after discharge to identify paroxysmal AF/AFL In all cases, consider anticoagulation (see Table 2 and Figure 3)3For patients with decompensated systolic heart failure: Consult cardiology, and consider digoxin or amiodarone for rate control.AV: atrioventricular; CAD: coronary artery disease; ECG: electrocardiogram; EP: electrophysiology; HR: heart rate; IV:intravenous; LV: left ventricular; WPW: Wolff–Parkinson–White.14
Figure 3: Management of anticoagulation therapy in atrial fibrillation and atrial flutter15
Figure 4: Emergency Department screening for early cardioversion of atrial fibrillation and atrial flutterCrCl: creatinine clearance; SBP: Systolic blood pressure.6
Table 1: Diagnostic evaluation of atrial fibrillation and atrial flutter Current electrocardiogram (ECG)Complete physical examCurrent Basic Metabolic Panel, Magnesium, complete blood count (CBC)Current thyroid stimulating hormone (TSH)Chest X-ray (CXR)Serial cardiac enzymes (Troponin, CK, CK-MB) as indicatedContinuous telemetry monitoringEcho within the past 6 months to assess for the presence and severity of structural heart diseaseTable 2: CHA2DS2VASc score and annual stroke riskCHA2DS2VAScCongestive heart failure (or Left ventricular systolicdysfunction)Hypertension: blood pressure consistently above140/90 mmHg (or treated hypertension on medication)Age 75 yearsDiabetes MellitusPrior Stroke or TIA or thromboembolismVascular disease (e.g. peripheral artery disease,myocardial infarction, aortic plaque)Age 65–74 yearsSex category (i.e. female gender)11212111CHA2DS2-VAScScore0123456789Stroke Risk(%/year)01.32.23.24.06.79.89.66.715.2Table 3: When to consider a rhythm control strategy for atrial fibrillation/flutter First occurrence of symptomatic AF/AFLOccurrence or recurrence of AF due to reversible cause (e.g. hyperthyroidism, pulmonary embolism, postoperativestate, pneumonia, acute coronary syndrome/acute myocardial infarction ACS/AMI)Hospital readmissions for AF/AFL or management of AF-related comorbiditiesAtrial Tachyarrhythmia-related symptoms despite adequate rate control, or inability to achieve adequate rate controlCardiomyopathy presumed to be secondary to tachycardiaYounger patients (age 65), even with minimally symptomatic or asymptomatic AF/AFL7
Table 4: Pharmacologic agents useful for rate control in patients with AF/AFLWhen to consider use?[level ofDrugrecommendation / levelof evidence]Calcium Channel BlockersDiltiazemSee Figure 2[Class I, LOE olWarnings/ContraindicationsIntravenous DosingCan cause hypotensionand AV nodal block.CI: BradycardiaCI: Systolic heart failureIV: 10-20 mg IVP bolus over 2 min.If HR remains 120, consider asecond bolus over 2 minutesThen start infusion at 5 mg/hr, titrateby 2.5 mg/hr every 30 minutes toHR, maximum dose 15 mg/hr[onset time 2-7 min]IV: 2.5-5 mg IVP over 2 minutes;second dose of 5-10 mg ( 0.15mg/kg) may be given 15-30 minutesafter the initial dose if patienttolerates, but does not respond toinitial dose; maximum total dose: 2030 mg.[onset time 3-5 min]120 to 360 mg dailyin divided doses;extended- releasepreparation isavailable [onset 2 to4 hours]Oral dosing: If HR 120 after 5 mg IV,consider oral dose of25 mg PO BID.If HR 120 after 10mg IV, consider oraldose of 50 mg POBID. If HR 120after 15 mg IV,consider oral dose of75 mg PO BID.[onset 4-6 hours]N/A Loading dosesare not necessary dueto rapid onset ofactionCan be used as analternative to diltiazem.[Class I, LOE B]Can cause hypotensionand AV nodal block.CI: Bradycardia.CI: Systolic heart failureSee Figure 2[Class I, LOE C]Can cause hypotension andAV nodal block. Avoid inpatients withbronchoconstriction oremphysema. Use withcaution in patients withdecompensated heartfailure.CI: Bradycardia.IV: 5 mg IVP every 10-20 minutesx3[onset time 5 min].Can cause hypotension andAV nodal block. Avoid inpatients with acute oractive airway obstruction/bronchoconstriction. Avoidin patients withdecompensated heartfailure.Relatively expensiveCI: Bradycardia.IV: 50 mcg/kg/minute infusion for 4minutes. Infusion may be continuedat 50 mcg/kg/minute or, if theresponse is inadequate, titratedupward in 50 mcg/kg/minuteincrements (increased no morefrequently than every 4 minutes) toa maximum of 200 mcg/kg/minute.[onset time 5 min]Can cause hypotension andAV nodal block. Avoid inpatients with acute orchronic airway obstruction/bronchoconstriction. Avoidin patients withdecompensated heartfailure.CI: Bradycardia.IV: 0.5-1 mg over 1 minute; mayrepeat, if necessary, up to a totalmaximum dose of 0.1 mg/kg[onset time 5 min]Best for use in situationswhere there is anindication to use a betablocker, but the patienta.) cannot take oralmedications, or b.) has alabile or tenuous bloodpressure (esmolol has ashort half-life, and itseffect can be quicklyhalted by stopping theinfusion).[Class I, LOE C]Consider for use inthyrotoxicosis[Class I, LOE C]8Oral dosing/ notesIf HR 120 results, start oralmetoprolol (see dosing suggestionsto right). If HR 120 after 15 mgIV metoprolol, consider an alternateagent such as diltiazem above.120 to 360 mg dailyin divided doses;extended-releasepreparation isavailable[onset 1 to 3 hours]Usual oral dose: 1030 mg/dose every 6-8hours
Table 4: Pharmacologic agents useful for rate control in patients with AF/AFL, continuedDrugOther agentsAmiodaroneDigoxinWhen to consider use?[level ofrecommendation / levelof evidence]Primarily functions as anantiarrhythmic (rhythmcontrol) agent, as shownin Appendix A. Usefulas a second line ratecontrol agent when firstline agents fail, usuallyin consultation withcardiology or EP. Maybe useful in patients withdecompensated systolicheart failure. Also maybe useful in situationswhen an accessorypathway is suspected.[Class IIa, LOE C]Second line rate controlagent, primarily becauseit tends to exert its ratecontrolling effect at rest,less so with exercise.Most useful incombination with a betablocker or a calciumchannel blocker,especially for patientswith systolic heartfailure, or in cases wherelow blood pressure is amajor issue (digoxindoes not lower bloodpressure).[Class I, LOE B]Warnings/ContraindicationsIntravenous DosingOral dosing/ notesCan cause hypotension(when givenintravenously), andpulmonary toxicity (sopatients with severe lungdisease are poorcandidates for long-termadministration).Relatively expensiveNote: This medication canresult in cardioversionwhen used for rate controlCI: Bradycardia.IV: 150 mg IV over 10 minutes.Follow up with an infusion of 1mg/min IV x 6 hours, then 0.5mg/min IV x 18 hours.[onset time 20min]EP or generalcardiology consultshould be requested iflong-term amiodaroneuse is contemplated.Can cause AV nodalblock, digoxin toxicity.CI: Bradycardia, renalfailureLoading dose:10-15 mcg/kg LBW – rounded tothe nearest 0.125mg (most averagesized patients should receive 1mg).Administer load in 3 divided dosesas 50%, 25%, 25% of the total doseQ6 hours (i.e. total dose given over12 hours).Daily Maintenancedose*:CrCl 30 – Avoid useCrCl 30-60 0.125mgCrCl 60 0.25mgReduce total calculated dose by25% for IV loading. Considerreduction in loading dose for thosewith renal insufficiency.[onset time 30-180min]Use digoxin in patientswith renalinsufficiency withgreat caution, or not atall. Follow serumdigoxin levels wheninitiating treatment.Levels should beobtained at least 6-8hours post dose toallow for distribution.Due to its long halflife steady stateconcentrations will notbe reached for 5-7days*Above may needadjustment in elderlyand IBW 80kg or 60kgCI: ContraindicationLOE: Level of EvidenceLBW: Lean Body Weight9
Clinical Problem and Management IssuesDefinitions and ClassificationAF and AFL are supraventricular tachyarrhythmias; AF ischaracterized by uncoordinated atrial activation withconsequent deterioration of atrial mechanical function.Typical AFL is a macro-reentrant atrial arrhythmia utilizingthe cavotricuspid isthmus. AFL may result from treatmentto prevent recurrent AF.IncidenceAtrial fibrillation (AF) and atrial flutter (AFL) are the mostcommon sustained arrhythmias in the U.S., affecting 2.5million adults with the majority of patients over the age of65. AF/AFL is associated with numerous comorbiditiesincluding hypertension, coronary artery disease, heartfailure, and valvular heart disease. The cost of direct care ofpatients with AF in the U.S. is an estimated 6.65 billionannually, the majority of which is attributed tohospitalizations due to rapid ventricular response, heartfailure, and stroke. There are over 150 admissions to theUMHS annually with the principle diagnosis of new-onsetAF, and there are many more than that for recurrent orchronic atrial fibrillation.Many of the recommendations in this document apply toboth AF and AFL, especially as they relate to ratecontrol and anticoagulation.There are a number of types of AF/AFL: Rationale for Recommendations AF/AFL is prevalent in the population of patients evaluatedin the Emergency Department and admitted to the UniversityHospital. Given the vast spectrum of patient presentationsand the breadth of treatment options, management of AFpatients is inherently complex. Patients presenting with AFmay receive inconsistent care. These guidelines have beendeveloped to assure consistent care delivery for patients withAF across the inpatient services. These guidelines areapplicable to all inpatients with notable exception of patientson the Cardiology, Cardiac Intensive Care or CardiacSurgery Services. First detected - new onsetParoxysmal – self-terminating, episodes generally last7 days or less (most less than 24 hours)Persistent – not self-terminating, episodes usually lastlonger than 7 days, or require cardioversionPermanent – cardioversion failed to acutely convert orwas not attemptedRecurrent – both paroxysmal AF/AFL and persistentAF/AFL may be recurrentPost-operative – Post-operative AF/AFL usuallyoccurs within one week of the surgical procedureCauses and Medical Conditions Associated withAF/AFLIncidence of AF/AFL increases with increasing age. Manypatients have structural heart disease such as coronary arterydisease (CAD), hypertensive heart disease, valvular heartdisease (especially mitral regurgitation or stenosis), dities include obesity with or without sleep apnea,diabetes, and bronchopulmonary disease. AF/AFL may becaused by “reversible” causes such as post-operative state,pneumonia, pulmonary embolism, or hyperthyroidism.DiagnosisElectrocardiographic documentation is essential to establishthe diagnosis of AF/AFL. AF is characterized by thereplacement of consistent P waves by rapid oscillations orfibrillatory waves that vary in amplitude, shape, and timing,associated with an irregular, frequently rapid ventricularresponse. Patients in AF/AFL can rarely have regular cardiaccycles (R-R intervals), in the presence of AV block,ventricular tachycardia, or AV junctional tachycardia.TreatmentClinical Approaches: Unstable and Stable AF/AFLAF may be detected on a 12 lead surface ECG, Holtermonitor (usually 24 or 48 hour recording), or event monitor(usually worn for up to 3 weeks). AF may or may not beassociated with rapid ventricular response depending onintrinsic atrio-ventricular conduction system, autonomictone, and medications.The approach to the evaluation and management of AF/AFLdepends on the clinical circumstances of the arrhythmia. Forinstance, patients with unstable AF/AFL require immediatesupportive care for stabilization, and often require emergentinterventions to terminate the arrhythmia (rhythm control).On the other hand, patients with stable AF/AFL may notrequire emergent treatment, but might need measures tocontrol their heart rate (rate control) and prevent strokes(anticoagulation). Stable patients may not always requireinterventions to terminate the arrhythmia (rhythm control),although that may be appropriate is some cases.AF may occur alone or be associated with other arrhythmias,notably AFL and atrial tachycardia (AT). AFL in the typicalform is characterized by a saw-tooth pattern of regular atrialactivation called flutter waves on the ECG, particularlyvisible in leads II, III, aVF, and V1.10
Because of the differences between these groups, thisguideline will divide the discussion into 2 sections: a code if needed. A trial of amiodarone with an intravenousloading dose of 150mg over 10 minutes followed by a1mg/min IV infusion can also be considered.Unstable AF/AFLStable AF/AFLThere are also special considerations for populationspresenting to the Emergency Department, or those whoexperience AF postoperatively (with special considerationfor thoracic surgery).If a patient with unstable AF/AFL is successfullycardioverted with resolution of clinical instability, postcardioversion treatment should then transition to diagnosticevaluation as directed by Table 1 as well as consideringanticoagulation (Figure 3) and placing an EP consult forassistance with long-term rhythm management of AF/AFL.Unstable AF/AFLStable AF/AFL with RVRAF/AFL can be defined as unstable when it results in alteredmental status, ischemic chest discomfort, acute heart failure,or other signs of shock or hemodynamic instability. Patientswith unstable AF/AFL require rapid stabilization.Differentiating between hemodynamic instability that is adirect result of the arrhythmia and instability in the setting ofAF/AFL but secondary to another cause (such as sepsis,hypovolemia, ACS or PE) will help to determine the focusof treatment efforts.Stable AF/AFL with rapid ventricular response (RVR) canbe defined as AF/AFL with HR 110 at rest with no signsof instability listed above. Stable AF/AFL can be new,chronic, or paroxysmal, and differentiating between theseclasses can have important long-term managementimplications. In this section, we will focus on the evaluationand management of any type of AF with RVR.Evaluation of New-Onset AF/AFL. The evaluation ofAF/AFL is intended to discover the cause of the arrhythmia,and clinical features of the patient that might impacttreatment (See Table 1).An overview of initial management of unstable AF isillustrated in Figure 1, and includes cardiac monitoring,supplying supplemental oxygen, obtaining large-bore IVaccess, and addressing intravascular volume depletion withIV fluid administration, provided the patient does not havean acute exacerbation of heart failure.Management of New-Onset AF/AFL. The management ofstable, new-onset AF/AFL with RVR can be divided intothese general categories:At the same time, a focused history and physical should beconducted, with special attention paid to the duration andnature of symptoms, comorbidities, and identifyingreversible causes of AF/AFL. Underlying causes ofhemodynamic instability other than the arrhythmia should besought and treated, including early resuscitation for sepsis,blood products for severe anemia, cardiac catheterization forACS, anticoagulation and possible thrombolysis forpulmonary embolism. Supportive treatment with vasoactiveagents may also be necessary. Although cardioversionshould be considered in such patients, it is important torecognize that many of the critically ill patients seen in theED may have chronic AF or additional comorbidities thatmay lead to failed or short-lived effects of cardioversion.The main focus should be placed at treating the underlyingcondition causing the hemodynamic instability. Often, several of these categories of treatment will beapplied, in parallel. However, the main goals of AF/AFLwith RVR management are symptomatic improvement (viarate/or rhythm control), and prevention of thromboemboliccomplications (with antiplatelet or anticoagulantmedications). An overview of the management of stableAF/AFL is illustrated in Figure 2.Treatment of underlying conditions. Patients withAF/AFL with RVR can have a number of underlying acuteconditions (infectious, hypovolemia, anemia, etc.) that maybe driving the tachycardic response. These should besuspected and appropriately evaluated early, as treatment ofthese underlying conditions is key to resolving the RVR insuch patients.In patients who are hemodynamically unstable as a result ofAF/AFL without other causes for shock or hypotension,immediate synchronized direct current cardioversion(DCCV) is first-line treatment. For AF, the recommendedinitial energy level is 200 joules (J), which can be increasedto 360 J if lower energy levels are unsuccessful. For AFL,the recommended initial energy level is 50 J, which can beincreased to 200 J if unsuccessful.If cardioversion is repeatedly unsuccessful, a STAT CCUconsult should be placed to help direct care. Resuscitativeefforts should also be escalated to include consideration ofrespiratory support, additional vasoactive agents, and callingTreatment of underlying conditionsConsideration of an accessory pathwayConsideration of rhythm controlControl of heart rateAnticoagulationConsideration of an accessory pathway. Some patientswith AF/AFL will present with features suggestive of anaccessory pathway associated with Wolff-Parkinson-White(WPW) Syndrome. The ECG of a patient with preexcitationduring AF/AFL typically shows varying degrees ofpreexcitation, variable RR intervals and variable (bizarre)QRS morphologies. This represents a special circumstance11
in the management of AF/AFL and necessitates an urgent EPconsult.Should a patient with rapid AF/AFL not achieve adequatecontrol of their heart rate following an initial trial of one ofthe IV AV nodal blockers, the initial medication should bestopped and the other class of IV AV node blockade shouldsubsequently be attempted prior to adding adjunctivemedications. If both IV calcium channel antagonists and IVbeta blockers prove to be ineffective, consultation with EP isrecommended. Co-administration of oral beta blockers andnon-dihydropyridine calcium channel antagonists for longterm heart rate control may be necessary, and is generallysafe with the appropriate monitoring.Drugs contraindicated in patients with accessory pathwaysinclude digoxin, and non-dihydropyridine calcium channelantagonists (e.g. verapamil, diltiazem), which slowconduction across the AV node, and can result in paradoxicalacceleration of the ventricular rate, hypotension, orventricular fibrillation. Beta blockers are ineffective and maycause hypotension. When the arrhythmia is associated withhemodynamic compromise, early DCCV is indicated (seeFigure 1). In hemodynamically stable patients withpreexcited AF/AFL, procainamide is recommended torestore sinus rhythm. Further management should be guidedby consultation with EP. Of note, any patient withpreexcitation and syncope, with or without history ofAF/AFL, warrants inpatient EP consultation.There are a few notable considerations for patients withsystolic heart failure and AF/AFL. Non-dihydropyridinecalcium channel blockers are best avoided altogether in thispopulation. Also, in decompensated heart failure, both betablockers and non-dihydropyridine calcium channelantagonists may acutely exacerbate heart failure symptoms.Cardiology consultation is recommended for patientspresenting with decompensated systolic heart failure andAF/AFL with RVR. Digoxin and amiodarone are both usefulrate control agents in this population. Of note, amiodaroneresults in increased plasma digoxin levels.Control of heart rate. Rate control medications slowconduction through the AV node, thus slowing ventricularrates in rapid AF/AFL. In the absence of channelantagonists and beta-blockers are most commonly used, andcan safely achieve rate control in most patients. For patientswith AF/AFL and mildly elevated heart rates of 100-119 atrest (or those with resting heart rates that increase to 130with activity), adjustment of oral rate controlling agents cansafely be undertaken (Table 4). For rapid AF/AFL withelevated heart rates of 120 at rest, acute rate control ispreferred and is best achieved with intravenous formulationsof AV nodal blocking agents as illustrated in Figure 2.Digoxin has been largely replaced by more effective AVnodal blockers, but remains useful as an adjunct in patientswith heart failure. Digoxin has little, if any effect on bloodpressure, so it can also be useful in hypotensive patients.However, digoxin tends to exert its rate controlling effect atrest, less so with exercise, which may result in rate control atrest with continued tachycardia with exertion.Beta blockers should be considered early for the treatment ofnew-onset, rapid AF/AFL. Beta blockers are very effectivefor rate control, achieving the specified heart rate endpointsin 70% of patients compared with 54% with use of calciumchannel antagonists in the Atrial Fibrillation Follow-upInvestigation of Rhythm Management (AFFIRM) trial. Betablockers also have additional indications for comorbiditiesthat are commonly found in patients with AF/AFL, such ashypertension, CAD, or heart failure, although they may notbe well tolerated by patients with acute bronchospasm orsevere emphysema. Metoprolol is usually administered as5mg IV doses that can be re-dosed every 10-20 minutes forup to three doses. Metoprolol may cause hypotension andshould not be used in the setting of a labile or tenuous bloodpressures. In this setting, esmolol infusion is preferred dueto its short onset of action and rapid clearance. Of note,propranolol is most useful in the setting of thyrotoxicosis.Amiodarone is known to slow ventricular rates duringAF/AFL. It is generally indicated only when maintenance ofsinus rhythm is desired given its significant toxicities, butcan be used for rate control in some circumstances.Table 4 provides a review of drugs used for control ofventricular rate in AF/AFL, their side effects, andcontraindications. Long-term control of heart rate isimportant to control symptoms and to prevent thedevelopment of a tachycardia-induced cardiomyopathy, as asustained, uncontrolled tachycardia may lead to deteriorationof ventricular function. Fortunately, this tachycardiainduced cardiomyopathy tends to resolve within 6 months ofrate or rhythm control.For heart rate that cannot be controlled well withmedications: consultation with EP should be obtained if thepatient’s heart rate is not controlled after 24 hours oftreatment with adequate IV AV nodal agents.Non-dihydropyridine calcium channel antagonists, such asdiltiazem and verapamil, are another effective class ofmedications for heart rate control in AF/AFL. Calciumchannel antagonists should be used in the setting of acontraindication to beta blockers such as an allergy orbronchoconstriction. Diltiazem, given its rapid onset, tendsto be more popular, and has been shown in a randomizedcontrolled trial to be more effective in controlling theventricular rate than amiodarone or digoxin.12Defining adequate rate control. Based on the results of theRACE II trial, a resting heart rate 110 bpm indicatesadequate rate control. Treatment to achieve strict rate controlof heart rate (80 bpm at rest or 110 bpm during a 6-minutewalk) is not beneficial compared to achieving a resting heartrate 110 bpm in patients with persistent AF/AFL who havestable ventricular function (left ventricular ejection fraction .40) and no or acceptable symptoms related to AF/AFL. Of
note, long-term ( 3 years) effects on ventricular functionwere not evaluated in this study, therefore periodicmonitoring of LV function is recommended.future paroxysms of AF/AFL, therefore we recommend closefollow-up and monitoring of these patients (see SpecialConsiderations: Postoperative AF/AFL, below). In mostcases, these patients may be treated as if they haveparoxysmal AF/AFL, a condition that poses a stroke risksimilar to chronic AF. For patients with AF/AFL that convertspontaneously, we recommend these considerations:Consideration of rhythm control. Rhythm controlshould be considered in the following clinical scenarios(Table 3): First Occurrence of AF/AFLOccurrence or recurrence of AF/AFL due to reversiblecause [e.g. post-operative state, pulmonary embolism,pneumonia, or acute coronary syndrome/acutemyocardial infarction (ACS/AMI)]Hospital readmissions for AF/AFLAF/AFL-related symptoms despite adequate ratecontrol, or failure to achieve rate control despite the useof appropriate medicationsCardiomyopathy presumed to be secondary totachycardiaYounger patients (age 65), even with minimallysymptomatic
CI: Systolic heart failure : IV: 2.5-5 mg IVP over 2 minutes; second dose of 5-10 mg ( 0.15 mg/kg) may be given 15-30 minutes after the initial dose if patient tolerates, but does not respond to initial dose; maximum total dose: 20-30 mg. [onset time 3-5 min] 120 to 360 mg daily in divided doses; extended-release preparation is available