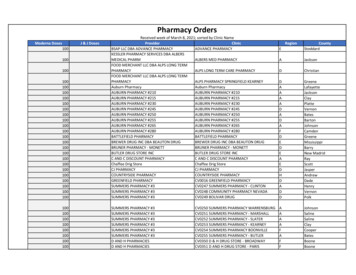
Transcription
Codeof Ethics2018SAFE EFFECTIVE PHARMACY PRACTICE
The principles and clausesof the Code of Ethics 2018(the Code) express theresponsibilities and professionalvalues that are fundamental tothe pharmacy profession; care ofthe patient, professional integrityand professional competence.
ContentsThe Pharmacy Council (Te Pou Whakamana Kaimatu o Aotearoa) 4Code of Ethics 4Relevant legislation 5Legal authority of the Code of Ethics 5Key Terms 6Te Reo Māori 6Principle 1: A pharmacist makes the health and wellbeingof the patient their first priority. 8Principle 2: A pharmacist practises and promotespatient-centred care. 9Principle 3: A pharmacist exercises professional judgement inthe interests of the patient, family, whānau and thewider community. 10Principle 4: A pharmacist acts with honesty and integrityand maintains public trust and confidence inthe profession. 11Principle 5: A pharmacist only practises under conditionswhich uphold the professional independence,judgement and integrity of themselves and others. 12Principle 6: A pharmacist demonstrates a commitment tocontinual professional and personal developmentto enhance pharmacy practice. 13Principle 7: A pharmacist works collaboratively with othersto deliver patient-centred care and optimisehealth outcomes. 14Schedule to the Code of Ethics 15Back to contents
Pharmacy Council of New Zealand – Code of Ethics 20184Code of Ethics 2018Pharmacists are health professionals who ensure safe and quality useof medicines and optimise health outcomes by contributing to patientassessment and to the selection, prescribing, monitoring and evaluation ofmedicine therapy. Pharmacists may work with varying levels of responsibilityand in different settings, including clinical practice, education, researchand industry.The Pharmacy Council(Te Pou Whakamana Kaimatu o Aotearoa)The Pharmacy Council of New Zealand (the Pharmacy Council) is the statutoryauthority that governs the practice of pharmacists. “The Pharmacy Council hasa statutory responsibility to set standards of competence and ethical conductto be observed by members of the profession.” The Pharmacy Council’sprimary concern in discharging its functions under the Health PractitionersCompetence Assurance Act 2003 is the protection of the health and safety ofmembers of the public.Code of EthicsThe principles and clauses of the Code of Ethics 2018 (the Code) express theresponsibilities and professional values that are fundamental to the pharmacyprofession; care of the patient, professional integrity and professionalcompetence. The Code also reflects and addresses the context of healthcarein New Zealand, for example, health disparities, a diverse population, theprinciples of the Code of Health and Disability Services Consumers’ Rights,the Treaty of Waitangi and Te Tiriti o Waitangi.The main purpose of the Code is to articulate the professional and ethicalvalues to which all pharmacists should conform and can expect of theircolleagues.The Code is also: a source of education and reflection for those entering the professiona guide for the public on the conduct expected of pharmacists, anda framework against which breaches of professional conduct can bejudged.Back to contents
Pharmacy Council of New Zealand – Code of Ethics 20185The Code is not intended to be exhaustive anddoes not provide guidance on every situation“The Code appliesencountered in professional practice.A pharmacist is professionally accountableto all pharmacists,for their practice, which means beingirrespective of whetherresponsible for their actions or inaction,they treat, care for orno matter what advice or direction ainteract directly withmanager or another professional gives them.patients and theTheir professional and ethical principles,public.”embodied in this Code, should be the basisfor making decisions, particularly where theymay experience a conflict of interest or competingprofessional responsibilities.The Code applies to all pharmacists, irrespective of whether they treat, carefor or interact directly with patients and the public. Breaches of the Codeshould be brought to the attention of the Registrar of the Pharmacy Council,and pharmacists have a professional obligation to report breaches.Relevant legislationThe Code of Ethics 2018 should be read alongside legislative and professionalobligations. A list is provided in the Schedule to the Code of Ethics.Legal authority of the Code of EthicsThe Code of Ethics 2018 is prescribed by the Pharmacy Council of NewZealand pursuant to Section 118(i) of the Health Practitioners CompetenceAssurance Act 2003 and comes into effect from 12 March 2018.The Code of Ethics 2018 replaces the Code of Ethics 2011. Content has beenrevised, to account for changes in technology and legislation, to be moreprinciple-based, and to align with the Pharmaceutical Society of Australia’sCode of Ethics 2017.Back to contents
Pharmacy Council of New Zealand – Code of Ethics 20186Key TermsThe terms used in this document are generally consistent with terms used inlegislation, and in the Pharmacy Council’s standards, protocols, statementsand guidelines. Some key terms and new terms are defined here to ensurethe document is clear. Digital health: The use of technology in healthcare, for example,electronic health records and referrals, electronic prescribing, real-timetechnology, and wearable devices. Patient: Any person receiving any health or disability products andservices from the pharmacy or other place from which services areprovided by the pharmacist. Pharmacist: A health practitioner who is registered with the PharmacyCouncil of New Zealand in the scope of practice of a pharmacist. In theCode any reference to a pharmacist also refers to an intern pharmacist. Scope of practice: The Pharmacy Council’s description of theprofessional services that registered pharmacists and intern pharmacistsmay undertake. An intern pharmacist will be supervised by a registeredpharmacist. The scope of practice is outlined in the CompetenceStandards for the Pharmacy Profession.Te Reo Māori Te Tiriti o Waitangi: The Treaty of Waitangi whānau ora: a focus on whānau self-managing and living healthylifestyles in a self-determined manner.whānau: families and individuals descended from a common ancestor;from a Māori perspective this would extend beyond the nuclear familyand to include cousins, grandparents and other relations, as well as nonbiological family.Back to contents
Pharmacy Council of New Zealand – Code of Ethics 20187Introduction to the principles andclauses of the Code of Ethics 2018The principles are all equally important and the clauses andexplanations are to provide additional guidance to supporteach principle. The principles are grouped in three themes,care, integrity and competence.CareIntegrityCompetenceCollectively, Principles1 to 3 place the careof patients first,and recognise thatpharmacists also havea role in supportingfamily, whānau, thewider community andpublic health.Principles 4and 5 addressprofessionalintegrity.Principles 6and 7 are aboutprofessionalcompetency.Back to contents
Pharmacy Council of New Zealand – Code of Ethics 20188Principle 1: A pharmacist makes the health andwellbeing of the patient their first priority.Te kaimātau rongoā – Ko te mea tuatahi, ko te oranga, ko temanaaki tangata.Principle 1 places the health and wellbeing of patients at the centre of allpharmacy practice.A pharmacist:A. Fulfils their duty of care to the patientfirst and foremost.B. Ensures that their duty of care is notcompromised by other interests andmanages potential conflicts in theinterests of the patient.C. Exercises compassion and caretowards patients and the public in aculturally safe and responsive manner.D. Supports people who are vulnerableand tailors provision of careaccordingly.E. Promotes patient health, well-being,and whānau ora.F. Acts to prevent harm to the patientand the public.G. Promotes the safe, judicious andefficacious use of medicines, andprevents the supply of unnecessaryand/or excessive quantities ofmedicines, or any product which maycause harm.Back to contentsH. Before recommending, supplying orpromoting a medicine, complementaryand/or alternative medicine or otherhealthcare product or service,considers available evidence, andonly supplies a product when satisfiedthat it is appropriate, and the personunderstands how to use it correctlyand safely.I. Promotes continuity of care forpatients across health sectors andproviders, through appropriate referraland sharing of information.J. Recognises patients’ health status,abilities, cultural and social needsand provides or facilitates access toprofessional services delivered bythe pharmacist or other appropriateservices.
Pharmacy Council of New Zealand – Code of Ethics 20189Principle 2: A pharmacist practisesand promotes patient-centred care.Te kaimātau rongoā – Ko te whakamana, ko te manaakiā tangata whaiora, ko te whakamōhio te mea nui.Principle 2 articulates that pharmacists must display respect for patients andrespect diversity by avoiding discrimination on any grounds. They must alsoenable and involve the patient in making choices.A pharmacist:A. Respects and protects the autonomy,dignity and privacy of patients.E. Consults with an appropriate carer orappointed agent where the patientlacks the capacity to provide consent,B. Recognises and respects patients'or wishes to have whānau or otherdiversity, cultural knowledge and skills,support.gender, beliefs, values, characteristicsand lived experience, and does notF. Respects the patient’s choice,discriminate on any grounds.including the right to refuse treatment,care or advice, or to withdraw consentC. Encourages patients to participateat any time.in shared decision-making throughrespectful conversations, and assistsG. Safeguards and respects theby providing information and adviceconfidentiality of patients’ informationrelevant to the patient's clinical needswith appropriate security andin culturally appropriate language,safeguards applied to digital and harddetail and format.copy information.D. Explains the options available,including the risks and benefits, byproviding information that is impartial,relevant, up-to-date and independentof any personal commercialconsiderations to help patients makeinformed decisions.Back to contentsH. Refers patients to alternativeproviders if personal moral or religiousbeliefs prevent the pharmacist fromproviding a professional service, andappropriately facilitates continuityof care.
Pharmacy Council of New Zealand – Code of Ethics 201810Principle 3: A pharmacist exercises professionaljudgement in the interests of the patient, family,whānau and the wider community.Te kaimātau rongoā – Ko te matatikatanga, ko te pono o te kaimātaurongoā ki te tangata whaiora me te hāpori, te tino kaupapa.Principle 3 supports the pharmacist’s role in providing equitable andsafe access to resources, recognition of Te Tiriti o Waitangi, avoidanceof discrimination, and participation in public health initiatives.A pharmacist:A. Supports the right of all people, toaccess culturally safe and responsive,high quality professional services.B. Must recognise the status of Māoriand Te Tiriti o Waitangi in the NewZealand health sector and takeappropriate steps to recognise andrespond appropriately to the healthneeds of Māori including inequitiesin health and access to healthcareservices.C. Facilitates timely access to, andpromotes equitable use of,healthcare resources.D. Demonstrates financial stewardshipof both public funding and paymentscontributed by patients.Back to contentsE. Promotes and participates in publichealth initiatives.F. Promotes professional andenvironmental responsibility andaccountability for the control,procurement, preparation, handling,supply, storage and disposal ofmedicines and other healthcareproducts.G. Contributes to the achievement of theobjectives of New Zealand nationalhealthcare strategies.H. Contributes to public safety byparticipating in pharmacovigilance (forexample, reporting of adverse events)and risk management activities.
Pharmacy Council of New Zealand – Code of Ethics 201811Principle 4: A pharmacist acts with honestyand integrity and maintains public trust andconfidence in the profession.Te kaimātau rongoā – Ko te pono, ko te tapu, ko tewhakamāramatanga, te mana o te kaimātau rongoā.Principle 4 requires pharmacists to manage professional and business arrangementsensuring practice environments support the interests of the patient. It also sets principlesfor communicating about medicines, complementary and alternative medicines and otherhealthcare products and services.A pharmacist:A. Demonstrates accepted standards ofprofessional and personal behaviourin person and in any communicationby post, courier, and electronicmeans (for example, social media anddigital health).B. Provides services in an appropriateenvironment which reflects thecharacter and health-related nature ofthe profession.C. Provides accurate, truthful, relevant,and independent information in anappropriate form that is not misleadingto patients, the public and/or otherhealthcare professionals.D. Will not abuse their professionalposition or exploit the vulnerability orlack of knowledge of others.E. Responds honestly, openly,courteously and promptly tocomplaints and criticism.F. Avoids conflicts of interest by notoffering, requesting, or acceptingincentives, gifts, hospitality orreferrals and by not entering businessBack to contentsarrangements that may affect, orbe seen to affect, their professionalindependence or judgement, or limitpatients’ free choice of who they useto provide healthcare services.G. Declares and manages any actual,perceived or potential conflicts ofinterest in a clear, easy to understand,open and timely manner.H. Ensures that when providing anymedicine, complementary andalternative medicine, or otherhealthcare product or service, that thehealth and wellbeing of the patient orconsumer is the primary consideration,and that the benefit of use outweighsthe risk.I. Does not engage in advertising,promotion or supply of goods orservices that could include misleadingor unsubstantiated claims, and/ orundermine public trust in theprofession.J. Ensures business practices areconducted primarily in the bestinterests of patient and public health.
Pharmacy Council of New Zealand – Code of Ethics 201812Principle 5: A pharmacist only practises underconditions which uphold the professionalindependence, judgement and integrity ofthemselves and others.Te kaimātau rongoā – Kia whai tika, kia mau ki te mana o te ao o ngākaimātau rongoā.Principle 5 sets out that the pharmacist is responsible for their professionaldecisions, delegating work appropriately, compliance with legal obligationsand health and safety laws, and for good communication within thepharmacy profession and between all health professionals.A pharmacist:A. Exercises professional autonomy,objectivity and independence.G. Is responsible for actions of staff undertheir supervision.B. Must not override the professionalautonomy of another pharmacist orother healthcare professional unlesspatient safety is compromised.H. Raises concerns and takes appropriatesteps if policies, systems, workingconditions or the actions of othersmay compromise patient care orpublic safety.C. Fulfils all legal obligations.D. Ensures that all professionalactivities are covered by appropriateprofessional indemnity arrangements.E. Behaves in a manner that clearlydemonstrates responsibility andaccountability for all decisions madeand actions taken in their professionalpractice.F. Communicates with team membersregarding each person's responsibilityand line of reporting, and onlydelegates tasks to team members withappropriate qualifications, ability andexperience.Back to contentsI. Behaves with respect, anddemonstrates effective communicationand cooperation with all teammembers and other healthprofessionals.
Pharmacy Council of New Zealand – Code of Ethics 201813Principle 6: A pharmacist demonstratesa commitment to continual professionaland personal development to enhancepharmacy practice.Te kaimātau rongoā – Kia whakapiki te mātaurangao ngā kaimātau rongoā, ki tō rātou umanga, hei puāwai.Principle 6 requires a pharmacist to commit to ongoing professional development anddevelopment of the profession. They must maintain up-to-date knowledge of clinicalpractice, relevant legislation, regulations, codes and Pharmacy Council standards,protocols, statements and guidelines. They must also support colleagues and referunethical or harmful behaviour to the Pharmacy Council or the relevant authority.A pharmacist:A. Maintains contemporary knowledgeof evidence-based practice.B. Manages personal health andwellbeing to ensure there is nonegative impact on professionalpractice.C. Is accountable for practisingsafely and providing professionalservices only within their own scopeof practice, and for maintainingprofessional competence relative tothis scope of practice.D. Commits to lifelong learning and selfdevelopment consistent with theirrole, responsibility and their scope ofpractice.Back to contentsE. Commits to the development andenhancement of the professionand participates in activities to thateffect, for example: staff training;acting as a preceptor; mentoringstudents, interns and colleagues;and promoting the roles andresponsibilities of pharmacists topatients, the community and otherhealth professionals.F. Recognises behaviour in themselvesor colleagues which indicates a needfor referral, advice or support, andexercises their statutory obligationsto limit their own practice accordingly,or to make a health referral of acolleague.
Pharmacy Council of New Zealand – Code of Ethics 201814Principle 7: A pharmacist works collaborativelywith others to deliver patient-centred care andoptimise health outcomes.Te kaimātau rongoā – Kia mahi tahi, ko te whakawhanaungatanga o tekatoa, i roto i te ao oranga, te ngako o te manaaki ā tangata whaiora.Principle 7 requires a pharmacist to collaborate with their patients andother health professionals to deliver improved health outcomes and timelycoordinated care.A pharmacist:A. Plans and manages professionalactivities according to the needs ofpatients and the public.B. Exercises independence andprofessional judgement working withintheir scope of practice when providingsupport and advice to other healthprofessionals.C. Respects and acknowledgesthe expertise of other healthprofessionals.D. Establishes good workingrelationships with other healthprofessionals and others to enableconsultation, communication andcollaboration to optimise healthoutcomes with the patient.Back to contentsE. Attains and maintains the highestpossible degree of ethical conductand avoids any conduct that mightbring the profession into disrepute orimpair the public’s confidence in thepharmacy profession, colleagues orother healthcare professionals.F. Consults with the prescriber, anddocuments the result if there arereasonable grounds to consider thata prescription contains any error or isnot legitimate or could be detrimentalto a patient’s health.
Pharmacy Council of New Zealand – Code of Ethics 201815Schedule to the Code of EthicsThe Code of Ethics is to be read in conjunction with legislation, regulations,codes and Pharmacy Council standards, protocols, statements and guidelines.This schedule provides a list of key documents – the schedule is notexhaustive and all pharmacists are expected to practise in accordance with alllegislation, regulations, codes of practice and standards which impact on thepractice of pharmacy and the delivery of health and disability services.Legislation Commerce Act 1986Consumer Guarantees Act 1993Crimes Act 1961Fair Trading Act 1986Health Act 1956Health and Disability Commissioner Act 1994 Health and Disability Services (Safety)Act 2001 Health and Safety at Work 2015 Health Practitioners Competence AssuranceAct 2003Human Rights Act 1993Accident Compensation Act 2001Medicines Act 1981Medicines Amendment Act 2016Misuse of Drugs Act 1975Misuse of Drugs AmendmentAct 2016New Zealand Bill of Rights Act 1990New Zealand Public Health & DisabilityAct 2000Official Information Act 1982Privacy Act 1993Vulnerable Children Act 2014Regulations Dietary Supplement Regulations 1985Health and Disability Commissioner (Codeof Health and Disability Consumers’ Rights)Regulations 1996Back to contents Health and Safety at Work (General Risk andWorkplace Management) Regulations 2016Health (Needles and Syringes) Regulations1998Health Practitioners Competence Assurance(Restricted Activities Order 2005)Health (Retention of Health Information)Regulations 1996Medicines (Designated PharmacistPrescribers) Regulations 2013Medicines (Designated Prescriber:Registered Nurses) Regulations 2016Medicines (Designated Prescriber:Dietitians Regulations 2015Medicines Regulations 1984Medicines (Standing Order)Regulations 2002Misuse of Drugs Regulations 1977The Medicines (Database of MedicalDevices) Regulations 2003Codes Advertising Standards Authority Inc.Therapeutic and Health AdvertisingCode 2016Health Information PrivacyCode 1994Code of Health and Disability ServicesConsumers’ RightsMinistry of Health, Code of Practice forChild Resistant Packaging of ToxicSubstances, 1998
Pharmacy Council of New Zealand – Code of Ethics 2018Standards Health and Disability Services – PharmacyStandards NZS 8134.7:2010Government Strategies New Zealand Health Strategy 2016 Implementing Medicines New Zealand2015-2020 He Korowai Oranga: Māori HealthStrategy 2014 Pharmacy Action Plan 2016-2020New Zealand Disability Strategy2016-2026Pharmacy Council and jointstatements, guidelines andprotocols1 Complementary and Alternative Medicines(CAM) Statement and Protocol forPharmacists 2017Competence Referral to the PharmacyCouncil Guide 2013Health Equity Statement 2013 (PharmacyReference Group for the Implementation ofthe Strategy for Māori Health (PRISM))Social Media and the PharmacyProfession 2012Sale of Codeine Containing Analgesics2016 (Pharmacy Council & PharmaceuticalSociety Inc.)Statement on Cultural Competence 2011Statement on Promotion and Supply ofMedicines over the Internet 2015Statement on Raising Concerns withPrescribers 2015Workplace Pressures in Pharmacy– Practical advice for New Zealandpharmacists 2012International United Nations Convention on the Rightsof Persons with Disabilities (ratified byNew Zealand in 2008).United Nations Declaration on the Rightsof Indigenous Peoples (adopted byNew Zealand in 2010)Sector Strategies Māori Health Strategy for the PharmacyProfession 2007Strategy for Māori Health – (PRISM)Protocol for the Sale and Supply ofPharmacist Only Medicines for ChronicConditions 20171 Please note that all statements, guidelines and protocols were correct at the time of printing.Please refer to the Pharmacy Council's website for the latest version.Back to contents16
The Pharmacy Council of New ZealandTemporary offices:Level 18, Plimmer Towers2-6 Gilmer TerraceWellington 6011New ZealandPO Box 25137Featherston StreetWellington 6146New ZealandPhone 64 4 495 uncil.org.nz
The Code of Ethics 2018 replaces the Code of Ethics 2011. Content has been revised, to account for changes in technology and legislation, to be more principle-based, and to align with the Pharmaceutical Society of Australia's Code of Ethics 2017. "The Code applies to all pharmacists, irrespective of whether they treat, care for or interact .