Transcription
Smart approaches to top-level decision makingStrategicFi nanciaP anningClosing the Meaningful Use Gap forSnnall/Rural HospitalsINSIDE THIS ISSUEBy Lauren PhillipsReform at Half-Time: ACAVersus the Economy5Two CAHs Team Up to AchieveMeaningful Use6Hospital Consolidation Leadsto Price Increases7Did Hospital Value Improvev/ith the Economy?8Pinpointing Your Hospital's SpecificICD-10 Reimbursement Risks12Happy Endings Are Possible for SmallHospitals in Today's Credit Markets14Nonelderly Insured and UninsuredAre Skipping or Delaying Care15How Unwritten Rules CanSabotage Budgeting/ForecastingSmall and rural hospitals have the advantage of beingnimble and having to corral fewer people to consensus thaniarge hospitals, but finding IT skills and funds is often aconstant struggle. The non-traditional financing approacheshighlighted in this article may help shrink the IT disparitybetween small/rural and large/urban hospitals. - - MORE ONLINESubscribers can access back issuesof Strategic Financial Planning,as well as web exclusive content,at www.hfma.org/sfp.16
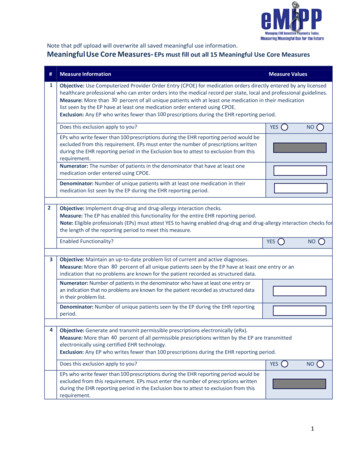
Closing the Meaningful Use Gap for Small/Rural Hospitals continued from page jGiven the high cost and complexity of electronic health record (EHR) implementation, it is not surprising that small andrural hospitals continue to lag behind: Onlyi3.9 percent of small hospitals and 12.9percent of rural hospitals were in a positionto qualify for Stage 1 meaningful use incentives at the end of ?oii, according to a May?oi3 Health Affairs study. In comparison, 9-7 percent of large hospitals and 20.3percent of urban hospitals qualified.In fact, this EHR gap grew from 2010 to2011; Small and rural hospitals that hadsome form of EHR jumped about 10 percent in that time, compared with 17.3 percent and 12.1 percent growth for large andurban hospitals, respectively.Yet, says Tracey Mayberry, partner, CSCHealthcare Group, most organizationsunderstand that, even if they can't movefast enough to meet the deadlines fora. DesRoches, CM, et al, "Small, Nonteaching, and RuralHospitals Continue to Be Slow in Adopting ElectronicHealth Record Systems," Health Affairs, April 2012,vol.31, no. 7.meaningful use incentive payments, theymust act in time to avoid the penalties fornoncompliance that go into effect in 2015.To do otherwise "is really almost anadmission that you're done as a hospital."The problem, of course, is resources—orrather, the lack of them. "Hospitals in therural market find it difficult to make thesignificant investment in EHRs due toconstraints in available financing, competing priorities for limited capital dollars, and thin operating margins," saysHFMA's Todd Nelson, technical directorfor senior financial executives/accounting.Whue bank loans and other traditionalfinancing options may be an option forsome well-positioned small/rural facilities, others may find better luck with philanthropy and nontraditional financingapproaches, such as the ones highlightedin this article.options to explore, says Aaron Fischbach,public health analyst. Federal Office ofRural Health Policy.Community Facility Direct and GuaranteedLoan Program. Under the auspices of theU.S. Department of Agriculture's (USDA's)Rural Development offices, the CommunityFacility program covers health IT and isintended to foster compliance with meaningful use in not-for-profit and publichospitals and clinics in communities ofless than 10,000 people.The Community Facility program has littlegrant money, says Fischbach. However,hospitals can use anticipated meaningfuluse incentive funds as collateral to borrowfunds from the Community Facility program . The terms on these loans givehospitals enough time to implement anEHR, attest to meaningful use, and thenuse the incentive paym.ents to repay atleast a major portion of the loan.Government Funding OpportunitiesSmall and rural hospitals have a numberof government-sponsored fundingGovernment IT Assistance: Looking for Guidance?A good place to turn is the 70 Regional Extension Centers, funded by the Office of the NationalCoordinator, which offer technical assistance, guidance, and information on best practices to support and accelerate providers' efforts to achieve meaningful use. This includes on-site technicalClinics need to take a more circuitousroute. Unlike hospitals, clinics do notqualify for direct EHR incentive payments; instead, the Centers for Medicareand Medicaid Services (CMS) programpays their clinicians, who typically reassign the payments to the clinic under theiremployment agreements.assistance to "priority primary care providers ' that have not yet adopted an electronic healthrecord (EHR) or that have certified EHR technology but need help meeting meaningful use criteria.Find the extension center that serves your region at wv/v/.regionalextensioncenters.com.Robert FrombergMaggie Van DykeSubscriptions are 165 for HFM A members and 195Editor-in-ChiefManaging Editorfor other individuals and organizations. To subscribe, callAmy D. LarsenProductionStrategic Financial Planning is published by theHealthcare Financial Management Association,Three Westbrook Corporate Center, Suite 6 0 0 ,Westchester, !L 60154. Subscribers receive a quarterlyprint newsletter and a quarterly e-newsletter.1-800-252-HFMA, ext. 2. Or visit Wma.org/sfp,Material published in Strategic Financial Planning isprovided solely for the information and education oíStrategic Financial Planning readers. HFMA does notIts accuracy. The statements and opinions in articles andcolumns in Strategic Financial Planning are those of theauthors and not those oí HFMA. References to commercialPresorted nonprofit postage paid in Rockford, IL 61109.manufacturers, vendors, products, or services that may 2012 HFMA.appear in such articles or columns do not constituteendorsements by HFMA.ISSN: 1934-7103Fall 2012 Strategic Financial Planningloans. To the extent that for-profithospitals can prove that job retentionand/or creation is involved, they can applyfor loans or loan guarantees to cover ITimprovements from the USDA RuralDevelopment's Business & IndustiyProgram or from the Small BusinessAdministration's capital loan programs.endorse the published material or warrant or guaranteeVolume 7, Number 42USDA and Small Business AdministrationUSDA Rural Development also sponsorsthree other programs where hospitals canlook for funding assistance with telecommunications software, hardware, andconnectivity:
The Rural Utilities ServiceTelecommunications InfrastructureLoan Program The RUS Broadband Initiatives Program The Distance Learning andTelemedicine Loan and Grant ProgramHUD block grants. Hospitals in counties orcities that are Entitlement Communitiesand, thus, eligible for monies under TheU.S. Department of Housing and UrbanDevelopment (HUD) CommunityDevelopment Block Grant Program, mayqualify for funds for equipment designedto provide improved community facilitiesand services—including hardware toimprove health services.CAH-specific programs. Critical accesshospitals (CAHs) and other hospitals withfewer than 4,9 beds can apply to tbeirstates for funds to help with activitiesrelated to qualify improvement and theeffective use of IT, which are availablefrom the Health Resources andAdministration's Small HospitalImprovement Program (SHIP) andMedicare Rural Hospital Flexibüify Grant(Flex) Program. Fischbacb explains thattbese programs grant money to the statesfor assistance to hospitals to provide, forexample, tecbnical or traininghelp—rather than funds to purchasehardware or software.Rural Health Care Program. One programthat Fischbach says is "very undersubscribed" is the Rural Health CareProgram, run by tbe Universal ServiceAdministrative Company under tbeoversight ofthe FCC. "Every monthly billfor pbone service includes a universalservice fee. Those fees are used to subsidize tbe costs of telecommunications forpublic and not-for-profit bealthcareproviders in rural areas, wbicb may payfour or five times as much as tbeir nearbymetro counterparts for tbe same services.Tbe subsidies can be significant—andMeaningful Use 101: Medicare Versus MedicaidMedicareMedicaidFederal government will Implemenf (will be anoption nationally).Voluntary for states to implement (may not be anFee schedule reductions begin in 2015 forproviders that are not "meaningful users" by2015.No Medicaid fee schedule reductions.Must be a "meaningful user" in year one.There is an adopt/implement/upgrade option forfirst participation year.Maximunn incentive is 44,000 for eligibleproviders.Maximum incentive is 63,750 for eligibleproviders.Meaningful use definition will be common forMedicare.States can adopt a more rigorous definition(based on common definition).Medicare Advantage eligible providers havespecial eligibility accommodations.Medicare Advantage Care providers must meetregular eligibility requirements.Last year an eligible provider may initiateprogram is 2014.Last year an eligible provider may initiateprogram is 2015.Last payment year in program is 2016; paymentadjustments begin in 2015.Last payment year in program is 2021.Only physicians, subsection (d) acute carehospitals, and critical access hospitals areeligible.Five types of eligible providers and two types ofhospitals are eligible.option in every state).Source: Mil e Alien, Winona Health Services, tailored this exhibit based on information pulled together by Cerner.there is a lot of money tbat isn't beingspent rigbt now. 'Networking Opens Other DoorsOne way small bospitals can obtain ITresources is by joining networks and consortia tbat take advantage of discountedpricing and economies of scale. Maybenybas seen a number of commimify bospitalsleverage strategic partnersbips—either byaffiliating or by joining large, mature independent deliveiy networks—to gain accessto solutions, products, and talent tbey migbtnot otbenvise be able to afford."Smaller organizations witb non-overlapping geographies can form collaborativesto work on IT initiatives, especially if tbeyhave a common vendor. For example, tbeymight start a shared service organization,essentially combining their IT operations," she says.Fischbach cites another advantage ofaffiliation. "Small, independent hospitalstend to be tbe last priorify for vendors tbatcan make more money working witb a bigbealtb system like Mayo or KaiserPermanente. So if tbe small hospitals cangroup together, they can not only save onhardware purchases but they can also probably get the attention of a vendor sooner."To encourage collaboration among ruralproviders, HHS allocated 12 million in2011 for grants to networks of ruralhealthcare organizations in support of ITadoption and and meaningful use. Tbemoney must be used for purcbasingtecbnology, installing broadband networks, and training staff.In ?oii, when 25-bed Jersey ShoreHospital in north central Pennsylvaniadecided to team up with 21-bed FultonCounfy Medical Center in McConnelsburg,2.5 bours away, the two CllAHs didn't evenknow about tbe availabilify of tbese HHSgrants. They were just looking for a meansto share IT resources needed to acbieveWnia.org/sfp Fall 20123
meaningful use, including joint installation of an EHR that would otherwise havecost each organization an estimated ?.3 million, according to CareyPlummer, Jersey Shore's CEO.Thanks to the Pennsylvania MountainsHealthcare Alliance, a 19-hospital collahorative to which both helong, they foundeach other, a partnership that has savedeach some 3oo,ooo on EHR implementation—and provided grant money, too.Both hospitals expect to attest to stage 1meaningful use criteria by Sep. 1, 3oi3.(For more details, see the case study onpage 6 of this newsletter.)Vendor RelationshipsNot all small and rural healthcare organizations are struggling to find IT dollarsand meet meaningful use deadlines; someof them were close to the finish line whenthe American Recovery and ReinvestmentAct was enacted. Winona Health Services,a Minnesota system consisting of one99-bed hospital, a nursing home, anassisted living community, and 4,5 employedphysicians, started its EHR journey morethan 10 years ago and was ready to attestin November 2011, says CFO and treasurer Michael M. Allen, FHFMA, CPA."We really just needed to go the last mile.There were a few small pieces of functionality to put in place, and there was stillwork to do with the medical staff to bringa few operational processes in line withmeaningful use criteria."Central to Winona's success, according toAllen, is something he recommends thatevery small hospital pursue: a close,strategic, integrated relationship with itsEHR provider."As a small, independent system thatwanted to accomplish big things, we knewwe'd get lost in the shuffle with any vendor if the relationship was simply based4Fall 2012 Strategic Financial PlanningLeasing Now an Option for CAHsMany critical access hospitals (CAHs) breathed a sigh of relief in July when the Centers for Medicare& Medicaid Services (CMS) changed its policy to allow CAH's nneaningful use incentive payments toinclude the cost of capital leases for certified electronic health record (EHR) technology.Previously, while a CAH could include lease costs on its cost report, only reasonable costs to whichpurchase depreciation would apply were allowable for incentive payments. But in July, CMS decided that a capital lease is essentially the same asa virtual purchase agreement and meets the intentof the statute and regulation to qualify the leased asset as a purchased asset. The cost must bebased on the fair market value of the asset at the date the lease was initiated. For more informationabout this reversal, visit www.cms.gov/EHRIncentivePrograms.on a transaction. The EHR is so critical tothe goals of the organization and of thecommunity. You need to feel comfortablewith your partner, and be able to worktogether over tbe long haul."Despite due diligence, Allen cautions thathospitals are not going to fully understandwhat they're getting from a vendor atproposal time; it's just too complex."Increasingly, however, EHR systems aregoing to cost about the same and haveabout tbe same functionality. Ifyou have astrong, give-and-take relationship, thecost and other issues will fall into line. "What does a give-and-take relationshiplook like from the provider side? Feedbackplays a prominent role. AUen himself sitson the vendor's client care council with 35or 40 other hospitals and systems."We get together at least twice a year andat other times on the phone, and work onimprovements and solutions to problemsin tbe delivery or use of software or tbebilling for software—whatever it mightbe. It's rewarding from my perspectivebecause I've got colleagues from all theseother places in the room, and we learnfrom each other."Likewise, Winona physicians sit on thevendor's physician council, which focuseson how physicians use the software toimprove patient care and workflows, andhow changes could enhance and accelerate those improvements."We also open ourselves up for site visitsby other small hospitals that want to seehow the system is working," says Allen."The vendor organizes the visits, but itstill takes a day of our time every time."In return, Allen explains, the vendorhelps Winona mature its software. "Maybethey need a beta partner for some newsoftware, which is exciting and interestingbut also very time intensive. So, typically,they will end up giving us that functionality or discounting it significantly."Sometimes there are gray areas in theagreement, things the provider and vendor don't see eye to eye on. BecauseWinona has been generous in workingwith the vendor, "they're going to be moreflexible and understanding," says Allen."If all you do is take, at some point tberelationship is just not going to be therewhen you need it most, " he continues."You need to make investments of moneyand effort both. Structure the contract in away that you can manage financially, thenroll up your sleeves and put in the time."Maximum ValueOnce a hospital has an EHR in place thatwill allow it to quality for meaningful use
A commentary by Jeffrey C. Bauerincentives, how can the hospital be sure itis getting maximum value from that sys tem? The trick, says Jim D'ltri, partner,GSG Healthcare Group, is to not stop there.Reform at Half-Time: ACA Versus the EconomyThe Supreme Court's ruling on the Affordable Care Act is not the end of thereform game. It's half-time. Here's my color commentary on what we've seen"In a small way, meaningful use is pushingthe effective application of automation tomake the hospital more efficient, but itdoesn't go far enough in terms of safetyand quality. The hospital has to engrainthe meaningful use values into its culture,into its normal workflows. For example,meaningful use requires 3o percent ofmedical orders to be done through computerized provider order entry. But itmakes no sense to stop at 3o percent."so far, and what we might expect as play continues.The Affordable Care Act (ACA) v/as enacted atoniy 60 percent—leaving the insured patientthe end of a bruising first quarter. Nothing muchwith a 4 0 percent out-of-pocket obligation.happened in the second as everyone v/aited forMany ACA fans will cry foul when they discoverjudges to decide if the game v/as being playedthis unpleasant play in the game plan. (As Chiefaccording to the rules. Assuming the same teamsJustice Roberts noted, the Supreme Court onlyreturn after half-time elections, lobbyists playingdecides whether a law is constitutionai, notfor both sides will dominate the third period. Anwhether it is viable.)underrated piayer—the economy—wiii determinethe outcome in the final quarter.capacity. Personal wealth, employment income,Why? The 2012 Roberts decision upheld a 2010Meaningful use, like the EHR, is part of amuch bigger agenda, says D'ltri. "In theend, it's about harmonizing investmentsto foster accountability, assuming responsibility for the health of a population, andmanaging consumption wisely." The second trend is ongoing decline in spendingconsumer confidence, and other key compo-iaw built on unrealistic projections that the econ-nents of purchasing power have fallen dramati-omy would recover before the mandate goes intocally since 2 0 0 8 and are unlikely to rebound byeffect in 2014. The economy has not rebounded2014. The student loan bubble will probably burstas hoped, and today's consensus forecast sug-in the meantime, the banking system is digginggests neither governments nor patients wiii beitself into a deeper hole, and the global economicable to meet their financial obligations under theoutlook is depressing (literally). Taxes are alsolaw. if lobbyists don't neutralize key provisionslikely to rise over the next two years becauseLauren Phiiiips is president, Phiiiips Medicai Writers,over the next two years, economic stagnationausterity is not re-igniting economic growth.Ltd., Beiiingham, Wash., and a frequent contributor towill likely defeat the ACA.Strategic Financial Planning (phiiwrite@att.net).Hence, as an economist unabashedly committedEconomic Forces at Playto reinventing the way we deliver health care, ITwo economic forces make it difficult forsimply cannot see how consumers will be able toPoweil, Ohio (tmayberry2@csc.com). Todd Nelson,ObamaCare to win, even though the refereeshold up their end of the reform bargain when thetechnical director for senior financial executives/decided the game can continue. First, ACAmandate goes into piay. The ACA will not gener-accounting, HFMA, Westchester, iil. (tneison@hfma.org).makes mandatory insurance "affordable" by dra-ate more money for healthcare providersAaron Fischbach is public health analyst. Federalmatically cutting the covered portion of care.because there won't be more money in govern-Office of Rural Health Poiicy, Rockville, Md. CareyToday's average health pian pays approximatelyment coffers or consumers' pocketbooks. OddsPlummer is CEO, Jersey Shore Hospital, Jersey Shore,8 0 percent of a patient's health costs, leavingare that economics will defeat ObamaCare.Pa (cplummer@jsh.org). Michael M. Allen, FHFMA,20 percent to be billed to the beneficiary.interviewed for this article (in order of appearance):Tracey Mayberry is partner, CSC Heaithcare Group,CPA, is CFO and treasurer, Winona Health Services,Winona, Minn., and a member of HFMA's MinnesotaChapter(malien@winonaheaith.org). Jim D'ltri, partner,Mandated coverage in 2014 wiii be priced on anThe Providers' Cardactuarial assumption that basic insurance paysCan providers survive under such dismal circumstances? Yes, as long as strategic financialCSC Healthcare Group, Pittsburgh (jditri@csc.com).As an economist unabashedlyleaders work relentlessly to harness the abundant waste in current operations and redirectcommitted to reinventing therecovered resources to creating an efficient andway we deliver health care,effective delivery system—doing health careI simply cannot see howconsumers will be able tohold up their end of theright all the time, as inexpensively as possible.Some innovative American health systems havealready proven that it can be done without theACA. *reform bargain when themandate goes into play.Jeffrey C. Bauer, PhD, is an independent speaker andconsultant based in Chicago, (¡effbauer@mindspring.com)hlma.org/slp Fail 20125
Copyright of Strategic Financial Planning is the property of Healthcare Financial Management Association andits content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder'sexpress written permission. However, users may print, download, or email articles for individual use.
?oi3 Health Affairs study. In comparison, 9-7 percent of large hospitals and 20.3 percent of urban hospitals qualified. In fact, this EHR gap grew from 2010 to 2011; Small and rural hospitals that had some form of EHR jumped about 10 per-cent in that time, compared with 17.3 per-cent and 12.1 percent growth for large and urban hospitals .