Transcription
First independent framework for assessing pharmaceutical company actionAntimicrobial ResistanceBenchmark 2018METHODOLOGY 2017
Methodology for the 2018 Antimicrobial Resistance BenchmarkACCESS TO M E D I CI N E FO U N DATI O NThe Access to Medicine Foundation is an independent non-profit organisation based in the Netherlands. It aims to advance access to medicinein low- and middle-income countries by stimulating and guiding thepharmaceutical industry to play a greater role in improving access tomedicine.For ten years, the Foundation has been building consensus on the rolefor the pharmaceutical industry in improving access to medicine andvaccines. The sixth iteration of its Access to Medicine Index will bepublished in 2018. In 2017, the Foundation published the first Access toVaccines Index.AD D R ESSNaritaweg 227 ANL-1043 CB AmsterdamThe NetherlandsCO NTAC TFor more information about this publication, please contactGowri Gopalakrishna, Research Programme ManagerE gkrishna@accesstomedicinefoundation.orgT 31 (0)20 21 53 535W www.accesstomedicinefoundation.orgFU N D E RSThe Antimicrobial Resistance Benchmark research programme is madepossible with financial support from UK AID and the Dutch Ministry ofHealth, Welfare and Sports.
Access to Medicine FoundationAntimicrobial ResistanceBenchmark 2018Methodology ReportACCESS TO M E D I CI N E FOU N DATI O NAugust 2017
Methodology for the 2018 Antimicrobial Resistance BenchmarkACKNOWLE DG E M E NTSThe Access to Medicine Foundation would liketo thank all of the representatives of the manydifferent stakeholders working to curb antimicrobial resistance who contributed their views tothe development of this methodology.Expert CommitteeHans Hogerzeil (Chair)Greg FrankNina GrundmannMagdalena KettisJeremy KnoxJoakim LarssonMarc MendelsonKatarina NedogEvelina TacconelliEvelyn WesangulaResearch teamGowri GopalakrishnaJosefien KnoeffMarijn VerhoefTara PrasadEditorial teamAnna MasseyEmma RossThis acknowledgement is not intended to imply that theindividuals and institutions referred to above endorse theAntimicrobial Resistance Benchmark methodology, analyses or results. Decisions regarding inclusion of all feedback were ultimately made by the Access to MedicineFoundation.4
Access to Medicine FoundationA framework foraction on AMRThe global healthcare system depends onThe Benchmark is intended to complement andappropriate and timely access to antimicrobi-maximise the impact of these important initiativesals. Without antibiotics, there is no direct treat-on AMR.ment for infections, no safe surgery, no emergencymedicine. The unchecked rise of AntimicrobialIn the coming months, we will apply this frame-Resistance (AMR) puts this at risk for us all. Whilework to a cross-section of the pharmaceuticalAMR results from natural selection, the waysindustry, in order to report publicly on individualwe make, use and dispose of antimicrobials arecompanies’ actions along with their collaborativeundoubtedly accelerating its spread. To addressefforts. We will examine the evidence, compare dif-AMR, a fine balance must be struck – betweenferent approaches, recognise good practice, andappropriate access to antimicrobials and efforts toshine a light on where more action or coordinationcurb overuse and misuse. Novel antimicrobials andis vital. Our aim is to incentivise and guide positivevaccines are also urgently needed.change, spur deeper company engagement andchallenge the barriers to progress.These past years have seen growing attentionbeing paid to public health, paving the way towardNow is the time to tackle AMR. When antimicro-a global strategy on AMR. AMR has topped agen-bial resistance becomes widespread, it compro-das at G7 and G20 Summits, the UN Generalmises the very foundation of healthcare. No singleAssembly, the World Health Assembly and Worldstakeholder can bring AMR under control. GlobalEconomic Forum. Governments and the pharma-solidarity and collaboration between govern-ceutical industry have come forward to addressments, industry, NGOs and others is critical. Thisthe AMR threat. A group of companies has pub-Benchmark methodology can be seen as a frame-lished a roadmap for how they plan to play theirwork for action for companies seeking to join thepart. This commitment, action and willingness toglobal coalition of forces curbing AMR.share and collaborate is unique from the pharmaceutical industry.At the Access to Medicine Foundation, we have 10years of experience in publicly mapping how pharmaceutical companies are responding to globalhealth priorities. The idea of benchmarking company action to combat AMR came from discussions with the UK and Dutch governments. Theproposal of a benchmark was also endorsed by theJayasree K. IyerAMR Review Team. In this report, we publish theExecutive Directorfirst independent analytical framework dedicatedAccess to Medicine Foundationto assessing the industry’s engagement in curbingAMR. It has been developed with close referenceto the detailed research and initiatives underwayon AMR, and in consultation with many expertsand stakeholders working in the AMR field.5
Methodology for the 2018 Antimicrobial Resistance BenchmarkTable of contentsExecutive Summary7I NTRO D U C TI O NThe rise of AMR and the role of the10pharmaceutical industryPathogens and resistance12A benchmark to guide deeper pharmaceutical industry13engagement in AMRB U I LD I N G TH E M E TH O D O LO GYHow experts’ views were distilled into14a new benchmarking toolStakeholder dialogue14Stakeholders by group15Key discussions and decisions15Key discussions per Research Area16W H AT W E M E A SU R EWhat the Benchmark measures18Company scope18Disease scope20Product scope20Geographic scope20H OW W E M E A SU R EOverview of the analytical framework22R ES E ARCH AR E A SAResearch & Development24Indicators in Research & Development25B26Manufacturing & ProductionIndicators in Manufacturing & Production27C28Appropriate Access & StewardshipIndicators in Appropriate Access & Stewardship29APPE N D I CESI. Priority Pathogens included for analysis in R&D32II. Countries in scope for indicators A.4, C.1, C.2, C.333III. Products in scope for indicators C.2, C.334Definitions40Abbreviations40References416
Access to Medicine FoundationExecutive SummaryAntimicrobial resistance (AMR) is a widely recognised andmicrobial R&D, not least because of the major technical chal-growing problem. Without effective antimicrobials, infec-lenges involved in discovering and developing new antimi-tions become more difficult to treat, while medical and surgi-crobial classes. There is also little promise of a swift returncal procedures can become high-risk interventions, leading toon investment. New antibiotics are particularly highly soughtprolonged sickness, disability and death. AMR already causesafter, yet must be used conservatively to limit the risk ofmore than 700,000 deaths each year worldwide. The push toresistance emerging. This makes high-volume, high-returnlimit AMR requires a consolidated, concerted effort by multi-markets less likely to develop. Nevertheless, a core group ofple stakeholders, including governments, public health author-companies remain committed and have dedicated antimi-ities, international health organisations, academic institutionscrobial R&D divisions. To stimulate pharmaceutical companyand pharmaceutical companies.investment in R&D for new antimicrobials, the global AMRcommunity has established a range of both “push” and “pull”Although AMR is a natural phenomenon, its developmentincentives; these either lower the cost of developing a newis accelerated by the misuse and overuse of antimicrobials.antimicrobial medicine or reward its successful development.More rational use of antimicrobials is a cornerstone of strategies aimed at ensuring existing drugs remain useful forNumerous pharmaceutical companies have publicly commit-longer by decelerating the pace at which pathogens developted to tackling AMR, with many signing the “Declaration byresistance. Successful stewardship involves a ‘One Health’the Pharmaceutical, Biotechnology and Diagnostics Industriesapproach – an integrated approach addressing how antimicro-on Combating Antimicrobial Resistance” (The Davosbials are used in humans and in animals, as well as the antimi-Declaration), which was made in 2016. This was followedcrobial load in the environment.by the publication by a core group of manufacturers of an“Industry Roadmap for Progress on Combating AntimicrobialAt the same time, millions of people do not have access to theResistance” (Industry Roadmap). Both documents signal thatantibiotics and other antimicrobials they need, despite havingseveral pharmaceutical and biotechnology companies arecurable infections. Many of the global initiatives to addresspoised to play their part in addressing AMR.AMR aim to balance the need for better stewardship with theneed to enhance access where necessary. The need for newThe Antimicrobial Resistance Benchmarkstrategies and programmes to appropriately increase accessThere is growing recognition of the need for consensus onto antimicrobials remains particularly acute in low- and mid-the responsibilities of each stakeholder engaged in address-dle-income countries, where weaknesses in healthcare deliv-ing AMR, as well as the need for new, independent tools forery systems are often present. Such weaknesses can limittracking progress. The Access to Medicine Foundation hasaccess to antimicrobials while also promoting their inappro-responded to this need, drawing on its expertise in developingpriate overuse. These two issues are closely interlinked andindustry metrics related to public health. The Foundation hasmust be addressed in tandem.developed the Antimicrobial Resistance Benchmark, the firstindependent and public tool for measuring how pharmaceuti-In addition to stewardship and access, many global strategiescal companies are responding to AMR.for addressing AMR focus on pharmaceutical innovation andthe pipeline of antimicrobial products, to counter resistanceThe goal of the Benchmark is to incentivise pharmaceuti-to existing medicines.cal companies to implement effective actions for tackling theproblem of AMR. It will map the responses of a cross-sectionThe role of the pharmaceutical industryof the pharmaceutical industry to AMR, benchmarked againstAs AMR grows, there is a pressing need for novel products tothe consensus view on where they can and should be makingbe developed to treat life-threatening infections. Yet there isprogress. It will show where action is being taken in R&D,little incentive for pharmaceutical companies to invest in anti-access and stewardship, as well as where deeper engagement7
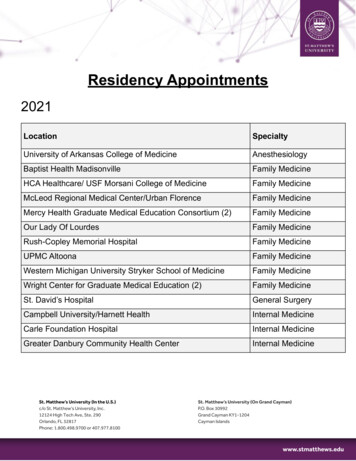
Methodology for the 2018 Antimicrobial Resistance Benchmarkby the industry needs further incentivisation. The Benchmarkaction have been distilled into the Benchmark’s analyticalwill be a tool for companies, governments, investors, NGOsframework. Methodology development began with the draft-and others seeking to deepen industry engagement in effortsing of a concept methodology after a review of reports andto curb AMR. Its analyses will identify innovative approachespublications analysing the scope, scale and potential solu-and best practices, and highlight where progress is beingtions to AMR. The review included policy reports by the AMRmade and where companies and other stakeholders can takeReview Team, Center for Disease Dynamics, Economics &action together, while pointing toward where new ideas arePolicy (CDDEP), Chatham House, DRIVE-AB, German Globalneeded.Union for Antibiotics Research and Development (GUARD),Pew Charitable Trust, ReAct and WHO. The Foundation teamHow the Benchmark was developedalso reviewed companies’ public commitments to addressingTo develop the Benchmark’s methodology, the Foundation’sAMR, as stated in the Davos Declaration and the subsequentresearch team sought input and gathered feedback fromIndustry Roadmap. The review was guided by the principlereports and a variety of stakeholders, such as governments,that the Antimicrobial Resistance Benchmark complementsnon-governmental organisations (NGOs), pharmaceuticalexisting processes for tackling AMR and builds on where con-companies and industry associations, investors, academia,sensus already exists between companies and stakeholders.public-private partnerships and relevant international organisations. The aim was to identify where stakeholders agreeThe review was followed by targeted engagement with keythat pharmaceutical companies can and should be takingstakeholders working on AMR, who were invited to challengeaction to curb AMR (see Figure 1). These opportunities forthe concept methodology. Their views were then balanced toFigure 1. How pharmaceutical companies can curb AMRThe Antimicrobial Resistance Benchmark maps pharmaceutical companies’ actions against priorities forlimiting AMR. A company’s opportunities to act are linked to its R&D pipeline and portfolio.If a company has:Its priorities for action are:Antimicrobial Investing in R&DR&D Developing priority antimicrobials Seeking open collaboration partnerships Planning ahead for appropriate access and stewardshipAntimicrobials Ensuring affordabilityon the market Limiting stock-outs and shortagesAntibiotics Registering products where access is neededon the market Ensuring manufacturing quality Minimising environmenal impact of antibiotic discharge Engaging in education on antibiotic stewardship Engaging in antibiotic surveillance systems Adapting packaging to enable rational use Supporting efforts to limit uncontrolled use Employing ethical sales and marketing practices8
Access to Medicine Foundationidentify the areas in which pharmaceutical companies can beThe Benchmark’s analysis will be presented around the fol-expected to take action. Industry views on the concept meth-lowing three Research Areas:odology were gathered in parallel. Strategic guidance wasprovided by an Expert Committee of specialists in AMR. TheA. Research & Development: This will assess company effortsresulting methodology distributes the performance indica-to develop new medicines and vaccines for infectious dis-tors across three areas where companies can be expected toeases. It will map their R&D pipelines, highlighting wherecontribute to the effort against AMR, described below as theefforts are being concentrated and whether gaps remain. ItBenchmark’s Research Areas.will also identify the proportion of company revenue investedin antimicrobial R&D and recognise efforts to target patho-What the Benchmark coversgens whose distribution and drug resistance makes them aThe Benchmark will evaluate pharmaceutical companiespriority target for R&D. This Research Area will also examinewith antimicrobial products and the ability and a commit-whether companies seek collaborative R&D partnerships toment to address AMR. A total of 30 companies are in scopetarget priority pathogens, and whether they put plans in place– across multinational research-based pharmaceutical com-during development for ensuring successful candidate prod-panies, generic medicine manufacturers and clinical-stageucts are made available rapidly, appropriately and affordablybiopharmaceutical companies with antimicrobial pipelines.in low- and middle-income countries.The opportunities for a company to act on AMR dependson its antimicrobial pipeline and portfolio. The AntimicrobialB. Manufacturing & Production: This includes an examinationResistance Benchmark will evaluate companies in threeResearch areas. Whether a company is measured in a spe-of how companies maintain the quality of their antibiotics, thecific Research Area depends on its antimicrobial portfolio andand environmental risk-management strategies for minimis-R&D.ing the impact of antibiotic discharge, and how transparentdegree to which they make provisions in their manufacturingthey are about these strategies, the results of audits and theTable 1. Analysis scopes for the AMR Benchmarklevels of antibiotic discharge.Company scope30 companiesC. Appropriate Access & Stewardship: This area will assess 8 large research-based pharmaceuticalcompaniescompany engagement in educating healthcare professionals 10 generic medicine manufacturersuncontrolled antibiotic purchases, practices related to eth- 12 clinical-stage biopharmaceutical companieson antibiotic stewardship, use of innovative models to reduceical marketing, the degree to which companies adapt theirbrochures and packaging to facilitate appropriate use of anti-Disease scopeInfectious diseases/pathogens Bacteria, viruses, protozoa, fungi, helminthsbiotics, and their contributions to AMR surveillance. ThisResearch Area also covers access to antimicrobial medicinesin 106 low- and middle-income countries. Indicators evaluating access plans include company efforts to register theirProduct scopeAntimicrobial medicines and vaccinesantibiotics in low- and middle-income countries, the evidence Medicines and vaccines in developmentbasis for company pricing strategies, and mechanisms for pre- Antimicrobial medicines on WHO Model List ofEssential Medicines 2017their highest-volume antimicrobial medicines. The aim is to AntibioticsGeographic scopeGlobal, with access indicators focusing on 106 lowand middle-income countriesventing stock-outs and improving demand forecasting forunderstand how companies approach these two challenges ofappropriate access and stewardship, and whether they integrate their approaches.9
Methodology for the 2018 Antimicrobial Resistance BenchmarkI NTRO DUCTI O NThe rise of AMR and the role of thepharmaceutical industryAntimicrobial resistance (AMR) is a widely recognised andance is the cause of death or it is a correlate of long antibioticgrowing problem that causes over 700,000 deaths eachtreatment, hospitalisation and underlying sickness.year worldwide.1 At the same time, millions of people cannotaccess the antimicrobial medicines they need, despite havingThe true extent of the burden of resistant pathogens is evencurable infections.2 These situations must be addressed inless well characterised for low- and middle-income coun-tandem. Steps to increase access must include measures totries. In part, this is due to an absence of local disease surveil-prevent resistance; steps to curb resistance must includelance systems, which are critical for monitoring and prevent-measures to enable appropriate access. Progress dependsing the rise and spread of diseases. The ability of differenton coordinated, disciplined efforts from many different play-stakeholders to understand and respond to the challengesers, not least in government, but also across the healthcareraised by AMR is affected by significant data limitations. Forand farming industries and the development and global healthinstance, information about antibiotic use, resistance levelscommunities.and transmission patterns is still scarce in many countries.Nevertheless, we know that mortality rates due to bacte-AMR threatens all countriesrial infections such as untreated pneumonia and sepsis con-In recent decades, AMR has become widespread, irrespectivetinue to be a public health problem in low- and middle-incomeof countries’ level of income. In Europe, it has been estimatedcountries, due to poor and/or limited access to relevant med-that 25,000 people die every year from antibiotic-resistanticines, especially in children.5 Many community-based infec-bacteria3 (see Figure 2). A recent report by the US Centerstious diseases, such as tuberculosis, remain more common infor Disease Control and Prevention (CDC) conservatively esti-low- and middle-income countries than in wealthier countries.mated that at least 2 million illnesses and 23,000 deaths ayear in the USA could be attributed to antibiotic resistance.4How does the problem vary globally?Such estimates are useful for giving an indication of the scaleAMR affects human health when infections become difficultof the problem, yet it is difficult to determine whether resist-to treat or life-threatening, and the appropriate antimicrobial mediciness do not exist, are unavailable, are of poor quality, or come at a prohibitively high cost to individuals and soci-Figure 2. Antibiotic resistance and increased risk of deathety. The exact impact of AMR on individuals and communitiesThe figure compares death rates (mortality) in patients with resistant anddepends on an interplay of factors, including the distributionsensitive strains of selected bacteria. Some pathogens are shown moreof pathogens, the prevalence of resistance to each, and thethan once, representing available data sets.availability of economic and healthcare delivery resources.Weaknesses in healthcare delivery systems can limit appropri-E. coliate access to existing antimicrobial medicines while also pro-A. baumanniimoting their overuse. These issues are closely interlinked andA. baumannii*can contribute to resistance; attempts to increase access canK. pneumoniaelead to overuse, which leads in turn to greater resistance. ThisK. pneumoniaethen increases the need for second- and third-line productsK. pneumoniaethat are more expensive, and thus harder to access. The needS. aureusfor new strategies and programmes to appropriately increaseS. aureus0Resistant strainSensitive strain1010%20%*Not fully sensitive30%40%50%60%Source: Adapted from ReAct: Action onAntibiotic Resistance, www.reactgroup.org, May 2012access to antimicrobial medicines remains particularly acutein low- and middle-income countries.2In the hospital setting, particularly in high-income countries,the public health focus and most clinical intervention is shift-
Access to Medicine Foundationresearch-based pharmaceutical companies or smaller biopharmaceutical companies. However, some larger researchbased pharmaceutical companies have generic medicine divisions, while some generic medicine manufacturers also investin R&D.Babu/Reuters/CorbisNeed for new products, low market promiseAs AMR grows, there is a pressing need for novel products tobe developed to treat life-threatening infections. Yet there islittle incentive for pharmaceutical companies to invest in antimicrobial research & development (R&D), not least becauseof the major technical challenges involved in discovering andThe need to increase appropriate access to antimicrobials is particularlydeveloping new antimicrobial classes. There is little prom-acute in many low- and middle-income countries.ise of a swift return on investment, as well as questionsaround pricing and affordability. New antibiotics in particu-ing to the increasing burden of chronic diseases including can-lar are highly sought after, yet must be used conservatively tocers, relative to infectious diseases. Where this shift has takenlimit the risk of resistance emerging. This makes high-volume,place, the infections that persist now tend to occur in sickerhigh-return markets less likely to develop. Since 2000, severalpatients and in challenging settings such as hospital intensivepharmaceutical companies have left the antibiotics market,care units. The resistant pathogens that have emerged hereare not as common as the underlying conditions and invasivestopping production and engagement in R&D. The numberof antibiotics in development also fell sharply.9 Nevertheless,procedures that set the stage for their presence. Yet, the con-a core group of companies remain committed and have ded-sequences of such infections for those with otherwise treata-icated antimicrobial R&D divisions. A growing number ofble conditions are life-threatening. Unless addressed early, thesmaller biopharmaceutical companies demonstrate a strongchance exists for a dramatic increase in high-risk infections.focus on antimicrobial R&D.Growing demandTo incentivise pharmaceutical companies to invest in R&D forInfectious disease products may broadly be broken down intonew antimicrobial medicines and vaccines, the global AMRthree categories: vaccines, diagnostics and antimicrobial med-community has established “push” incentives that reduceicines. The global market for such products reached USDthe costs of necessary inputs for developers. For instance,108.4 billion in 2015, and is forecast to reach USD 183.2 bil-the European Commission partners with the Europeanlion in 2021.6 The antibiotic market is expected to grow fromFederation of Pharmaceutical Industries and AssociationsUSD 27.1 billion in 2015 to USD 35.6 billion in 2022, in step(EFPIA) in the Innovative Medicines Initiative (IMI); Worldwith growing demand for generic antibiotics from emergingHealth Organization (WHO) and the Drugs for Neglectedmarkets.7 Human consumption of antibiotics is mainly grow-Diseases initiative (DNDi) have created the Global Antibioticing in low- and middle-income countries, where they areResearch and Development Partnership (GARDP), whichoften accessed over the counter rather than by prescription.is supported by the Federal Ministry of Health of Germany,Growing demand coupled with poor surveillance and steward-the Netherlands’ Ministry of Health, Welfare and Sports,ship is likely to drive the emergence of resistant strains.the South African Medical Research Council, and UKAID;the US government’s Biomedical Advanced Research andThe majority of antibiotics are generic; only a small numberDevelopment Authority (BARDA) and the Wellcome Trustremains on patent.8 In general, new antibiotics, antimicro-provide funding to CARB-X.bial medicines and vaccines are developed by either large11
Methodology for the 2018 Antimicrobial Resistance Benchmark“Pull” incentives are also being developed. They involve thepriced and prudently used. The challenge is to ensure afforda-promise of a reward for the development of new antimicro-ble, sufficient and appropriate access, while advancing antimi-bials targeting priority pathogens. For instance, the Unitedcrobial stewardship, within a viable business model.10States’ Generating Antibiotic Incentives Now (GAIN) Actgrants an additional five years of market exclusivity for com-Multiplayer solutionpanies developing antibiotics that target a selected group ofIn 2016, UN Member States committed to addressing thequalifying pathogens. Numerous initiatives, such as DRIVE-ABgrowing problem of antimicrobial resistance in the 2030and the German Global Union for Antibiotics Research andAgenda for Sustainable Development. Indeed, AMR isDevelopment (GUARD), have produced policy recommen-expected to affect the potential achievement of Sustainabledations on how to best to structure pull incentives. Novel asDevelopment Goal 3 (Good Health & Wellbeing), amongwell as existing antimicrobial medicines need to be affordablyothers. That AMR has risen up the global agenda is due atPATHOG E NS AN D RESISTANCEFour main groups of pathogenic microorganisms are relevant to currentefforts to curb AMR: bacteria (such asthose causing pneumonia and meningitis), viruses (such as HIV), fungi (suchas Candida) and parasites (such asPlasmodium falciparum, which causesHans R. Gelderblommalaria). There is large variation amongthese groups in how resistance emergesNIAIDand is transferred.Certain pathogens are already resistantto most antimicrobials on the market.Most infections with Methicillin-resistantThe HIV virus (above) has been identified byResistance emerges due to a variety ofStaphylococcus aureus (MRSA, above) occurr inWHO as a priority for strategies to address AMR.reasons such as the inappropriate usea hospital setting.of medicines, low-quality medicines,incorrect prescriptions and issues withinfection prevention and control.New and adapted medicines targeting different pathogens must take intoResistance mechanisms can comprise,for example, structural changes in oraround a medicine’s target molecule;reduced permeability of the cell membrane to the medicine; and the production of enzymes that inactivate themedicine.12CDC/Dr. Mae Melvin TranswikiKateryna Kon/Science Photo Librar yaccount their modes of resistance.Some strains of the Candida aurus fungusThere is a limited number of drugs available to(above) are resistant to all three major classes oftreat or prevent malaria caused by certain strainsantifungal drugs.of the parasite Plasmodium falciparum (above).
Access to Medicine Foundationleast in part to the actions of a range of advocacy and poli-have publicly committed to addressing AMR, with many sign-cy-oriented organisations and initiatives, such as the Allianceing the “Declaration by the Pharmaceutical, Biotechnologyfor the Prudent Use of Antibiotics (APUA), Doctors withoutBorders (MSF), the Global Antibiotic Resistance Partnershipand Diagnostics Industries on Combating AntimicrobialResistance” in 2016,11 followed by the publication of the(GARP), ReAct and the World Alliance Against Antibiotic“Industry Roadmap for Progress on Combating AntimicrobialResistance (WAAR).Resistance”.12 This is a clear sign that several pharmaceuticaland biotechnology companies are poised to play their part inLimiting AMR requires a consolidated, concerted effort byaddressing AMR.multiple stakeholders, including governments, pharmaceutical companies, public health authorities, international healthThere is growing recognition that we need consensus on theorganisations, and academic institutions to name a few. AMRresponsibilities for each stakeholder, as well as new, inde-is a public health issue that impacts not only human health,pendent tools for publicly tracking progress.1 The Access tobut the animal and agricultural industries as well. SuccessfullyMedicine Foundation has responded to this need, drawing onaddressing AMR requires a “One Health” approach that stim-its expertise in developing industry metrics related to publiculates increased access and affordability, stewardship thathealth. The Foundation has developed the Antimicrobiallimits overuse, innovative R&D in next generation medicinesResistanc
action have been distilled into the Benchmark's analytical framework. Methodology development began with the draft-ing of a concept methodology after a review of reports and publications analysing the scope, scale and potential solu-tions to AMR. The review included policy reports by the AMR Review Team, Center for Disease Dynamics, Economics &