Transcription
Integrating Physical and BehavioralHealth: The View from Primary CareProviders and PayersJuly 17, 2018www.facebook.com/pcpccwww.twitter.com/pcpcc
Welcome & Announcements Welcome – Robert Dribbon, PCPCC Executive Member Liaison PCPCC Annual Conference – Key Policies to Elevate Primary Care Washington, DC, November 8, 2018 Registration: www.pcpccevents.com Members Only Workshop: Investing in Primary Care – Advancing a National Strategy Immediately following the PCPCC annual conference, Executive Members are invited toan exclusive workshop on November 9, 2018 Registration: www.pcpccevents.com Stay tuned for the release of PCPCC’s annual Evidence Report on 8/8/2018 Interested in PCPCC Executive Membership? Email Allison Gross (agross@pcpcc.org) or visit:www.pcpcc.org/executive-membership
PanelistsModerator: Robert DribbonBruce Landon, MDPCPCC Executive Member LiaisonMerckProfessor of Health Care PolicyHarvard Medical SchoolJames Schuster, MD, MBAChief Medical Officer of Medicaid,SNP, and Behavioral ServicesVP, Behavioral IntegrationUPMC Insurance ServicesDivisionReactor: James KingslandPresidentNational Association Primary CareRussell Phillips, MDDirectorHarvard Medical School Centerfor Primary Care
Strategies for Behavioral Integrationinto Primary Care: Implicationsfrom a Microsimulation ModelBruce Landon, M.D., M.B.A.Department of Health Care Policy, Harvard Medical SchoolDivision of General Medicine and Primary Care, BIDMCRussel Phillips, M.D.Director, Center for Primary Care, Harvard Medical SchoolDivision of General Medicine and Primary Care, BIDMCPCPCC Webinar on Behavioral Health IntegrationJuly 17, 2018
Mental Health Problems are .9Mod/Severe56.58585.33.826.266.659.6Source: Kessler RC et al. Prevalence, Severity, and Comorbidity of 12 Month DXM-IV Disorders in the NationalComorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627. doi:10.1001/archpsyc.62.6.617
And Most Mental Health Care Occurs withinPrimary CareMental Health Care Delivered to Younger and Older Adults by Office‐Based Physicians Nationally, Volume: 63, Issue: 7, Pages: 1364-1372, First published: 03 July 2015, DOI:(10.1111/jgs.13494)
MH Care in Primary Care Lack of reimbursement for screening and prevention Lack of (until recently) reimbursement for collaborative careand case management Inability to bill solely for mental health services (manyMedicaid programs) Limitations in the ability to bill for physical and mentalhealth services in the same visit (e.g., time based and nontime based billing) Lack of training and comfort ent of Mental Health Servicesin Primary Care Settings.pdf
Yet, Collaborative Care Improves both MentalHealth and Physical HealthCollaborative CareUsual CareGlobal Improvement4518 1% in A1C3619 10 point in SBP1025 50% in SCL score6030Satisfaction with Depressioncare9055Satisfaction with chronic care8670Quality of life6.05.2Katon WJ et al. Collaborative Care for Patients with Depression and Chronic Illness.N Engl J Med 2010; 363:2611-2620
Using Simulation Modeling to InformPolicy Practices and policy-makers lack tools to estimateimpacts of new practice and payment models onpractice finances and outcomes Current practice structures are not optimized to deliverhigh value care
Key Assumption It is not rational to expect primary care practices toimplement changes that adversely impact their costs orrevenues
Why model? Used extensively in other fields tomodel investment and financialdecisions A “safe space” to write down allpossible assumptions andscenarios before piloting A technique to determine whichdecisions have low-uncertaintyand which have high-uncertainty(identify future research needs) Broaden generalizability beyondsingle pilot projectsIOM, 2011
Our Approach A microsimulation– What it is A simulation of individuals in a population– Advantages: Simulates individual patients with complex histories and comorbidities Simulates individual clinics with complex panels, staff, costs, andrevenues “High data, low assumption” modeling Can capture complex non-linear relationships and feedback loops Very flexible: can add queues, vary clinic types, and changefundamental structures in the model– Disadvantages: Lots of computer power needed Lots of data needed
New Medicare Payment Approach:Collaborative Care Model Involves care plan development often includingpharmacotherapy from the PCP, RN/master-level behavioristfollow-up care by phone Requires periodic psychiatrist or psychiatric NP/PA review forMedicare payment Three new Medicare Part B CoCM Codes– G0502 – Initial 30 min behaviorist session w/ 70 min/month overall caremanagement/staff effort– G0503 – Each 26-min behaviorist follow-up w/ 60 min/month of caremanagement– G0504 – Each additional 13-min of provider visit time w/ 30 min/monthof care management
New Medicare Payment Approach: PrimaryCare Behaviorist Model PCBM involves in-person care by primary care behaviorist (PhDpsychologist or LCSW) in brief, time-limited behavioraltreatments PCBM can be paid via traditional billing mechanisms forpsychologist/LCSW visits Also can be paid under new Part B behavioral health servicescodes– G0507 – 15 min of behaviorist provider time w/ at least 20 min/monthcare manager time– G0507 provides higher payments per period as compared to traditionalcodes for routine psychotherapy, psychological testing, and health andbehavioral assessment
Medicare Payment Rates CoCM– 140 for 70 min/patient for 1st month, 125 for 60min/patient for subsequent months PCBM– G0507: 48 for at least 20 min/patient/month
Modeling Approach
Results: FQHC (Serving MedicarePatients Only)ModelTime for caremanager/behaviorist(hours/yrs)Cost, annual after year1, per MD FTENet revenue,subsequent years, perMD FTECoCM1205.6 16,823.10 33,756.60PCBM1810.5 21,467.30-( 3,744.50)
Results: Urban or Rural, Lower-PovertyZone (Serving Medicare Patients Only)ModelTime for caremanager/behaviorist(hours/yrs)Cost, annual after year1, per MD FTENet revenue,subsequent years, perMD FTECoCM1496.0 19,171.10 27,009.60PCBM1734.9 20,729.00-( 3,646.30)
Take Home Points MH problems are extremely common and most MH careoccurs within primary care Traditional reimbursement models are poorlysupportive of models that integrate PC and MH New Medicare billing codes (particularly COCM) mightbe an attractive method for improving MH care inprimary care settings
Thank Youlandon@hcp.med.harvard.eduRussell Phillips@hms.harvard.edu
Team Members Sanjay Basu, MD, PhD– Asaf Bitton, MD, MPH– Harvard Medical School, Department of Health Care PolicyRuss Phillips, MD– Harvard Medical School, Center for Primary Care; Ariadne Labs; Center for Medicare & MedicaidInnovationBruce Landon, MD, MBA, MSc– Stanford University, Prevention Research Center; Institute for Economic Policy Research; Centers forHealth Policy, Primary Care & Outcomes ResearchHarvard Medical School, Center for Primary CareZirui Song, MD, PhD–Harvard Medical School; Massachusetts General Hospital, Department of Medicine
Behavioral Health Home Plusand Optimal HealthJames Schuster, MD, MBA201823
AGENDAOverview of UPMCThe Behavioral Health Home Plus (BHHP) ModelImplementation StrategiesProgram OutcomesExpansion of the Behavioral Health Home ModelConfidential information of UPMC and UPMC Health Plan. Any unauthorized or improper disclosure, copying, distribution, or use of the contents of this presentation is prohibited. The informationcontained in this presentation is intended only for the personal and confidential use of the recipient(s) to which the information has been distributed. If you have received this information in error,please notify the sender immediately and destroy the original information.24
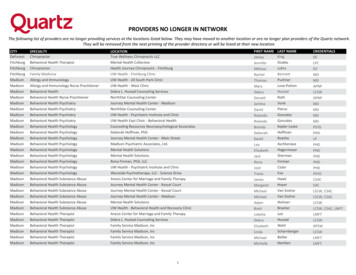
Integrated Delivery and Finance SystemIntegrated system with a world-class academic medical center,and affiliated with the University of PittsburghUPMC HEALTHSERVICES DIVISIONUPMCENTERPRISESUPMC INTERNATIONALAbout UPMCAbout UPMC Insurance Services Division More than 140 hospitals (including 38 UPMC-owned hospitals)and 24,000 providers More than 3.4 million members in CY 2017 UPMC’s community contributions were 912 million andrepresented more than 15 percent of net patient revenue Financial strength rating of A- (excellent) from A.M. Best More than 600 doctors’ offices and outpatient sites and60 UPMC Hillman Cancer Center locations 35 percent market share in western Pennsylvania Region’s largest network of rehabilitation services More than 4.7 million outpatient visits25UPMC INSURANCESERVICES DIVISION CY 2017 operating revenue was 7.5 billion (an increase of 11.2 percent) Almost 12,000 employer groups The largest behavioral health insurance provider in the nation A full product portfolio: HMO, PPO, EPO, HSA, dental, vision, COBRA,workers’ compensation, absence management, EAP, and more 41 percent medical-surgical market share in western Pennsylvania More than 97 percent of hospitals and other facilities, as well as morethan 98 percent of physicians in western PennsylvaniaData verified as of July 1, 2018 More than 60,000 network pharmacies nationwide
Innovation Drives Company GrowthLarge network anchored by UPMCUPMC Health PlanUPMC ConsumerAdvantageUPMC for LifeUPMC for LifeSpecial NeedsLife SolutionsUPMCInsuranceServicesWorkPartnersUPMC for YouWorkers’CompensationSolutionsUPMC for KidsCommunity CareBehavioral Health26UPMC VisionAdvantageUPMC DentalAdvantage
About Community Care 27Incorporated in 1996primarily to supportPennsylvaniaPart of the UPMCInsurance ServicesDivision501(c)(3) nonprofitbehavioral healthmanaged careorganizationLicensed as HMOUPMC ConsumerAdvantageUPMC Health PlanUPMC for LifeUPMC for LifeSpecial NeedsLife SolutionsWorkPartnersUPMCInsuranceServicesUPMC for YouWorkers’CompensationSolutionsCommunity CareBehavioral HealthUPMC for KidsUPMC VisionAdvantageUPMC DentalAdvantage
Community Care Behavioral Health Organization28 39 of 67 counties in 11contracts Only BHMCO in all PAHealthChoicesregions Four reprocurementsfrom competitors Experience with full-risk,shared-risk, andAdministrative ServicesOnly (ASO) contracts
What is a Behavioral Health Home?A behavioral health home (BHH)is a service delivery model that providesa cost-effective, longitudinal “homebase.”The BHH facilitates and coordinatesaccess to behavioral health care, medicalcare, and community-based socialservices and supports for people withcomplex medical, behavioral health, andsubstance use disorders.29
What is a Behavioral Health Home?The BHH is anchored in wellness guided by the triple aim:improving individual experience of care, improving population health,and reducing per capita health care costs“Wellness is not the absence of disease,illness and stress, but the presence ofpurpose in life, active involvement insatisfying work and play, joyful relationships,a healthy body and living environment, andthe presence of happiness.”— Peggy Swarbrick, PhD30
Key Behavioral Health Home Components31 Comprehensive care management Care coordination and health promotion Comprehensive transitional care Enhanced engagement in primary care and other physical health systems of care Individual and family support Community and social support services The use of health information technology to enhance population management
Community Care’s Behavioral Health Home PlusSuccessful early collaboration withCommunity Care and behavioral healthproviders in North Central region ofPennsylvania to address wellnessthrough BHH model in 201032
Behavioral Health Home PlusBHHP enhances the traditionalBehavioral Health Home model by: Adding a wellness nurse to theexisting team Using wellness coaching to addressself-management of modifiablelifestyle factors Developing a health registry to trackhealth needs and improvements Improving health literacy andhealth navigation33
Behavioral Health Home PlusKey componentsEngaging individuals inrecovery in ongoing wellnesscoaching based on the 8domains of wellness, especiallyPHWellnessNurse/WellnessCoachAddressing gaps in clinical careand coordinating PH servicesScreening for preventive healthconditions and history ofsignificant traumatic stressexposure34Establishing a reciprocal andcollaborative relationship withprimary care and specialtymedical providers
Wellness Nurse Coordinates the BHHP team interventionincluding the “virtual team” of communitybased medical and social service providers Serves as a medical consultant to nonmedical team members and wellness coaches Guides the team in identifying andaddressing gaps in clinical care andcoordinating care Develops a health resource library for theteam35
Wellness Nurse “Manages” the monthly registry of populationfocused data that identifies and stratifiesindividuals who have high-risk behavioral andmedical indicators Reaches out to the highest risk individuals onthe registry to discuss doing a physical healthassessment which helps to raise the individual'sawareness of need36
BHHP Outcomes: Optimal Health Optimizing Behavioral Health Homes byFocusing on Outcomes that Matter Mostfor Adults with Serious Mental Illness(Optimal Health) Study A multi-stakeholder collaboration to studythe key components of the BHHP model Contract awardee: UPMC Center for High-Value HealthCare Main partners include: Community Care University of Pittsburgh Stakeholder Advisory Board BHARP, NC and Chester Counties andProviders Principal investigators: James Schuster, MD, MBA, Community Care Charles (Chip) Reynolds III, MD,University of Pittsburgh Tracy Carney, CPRP, CSP, Community Care Supported by the Patient-Centered OutcomesResearch Institute (PCORI)37
CER to Examine BHH Models’ ImpactPatient Self Directed Wellness coaches Member registry Self management toolkitsProvider Supported Wellness coaches Member registry Nurse focused on wellness and health38
Learning Collaborative Process39Create ChangePackageImplementAction PeriodsDevelopCharterHold LearningSessionsSelect TeamsBegin PreWorkMeasureProgress
Create Change Package40Create ChangePackageImplementAction PeriodsDevelopCharterHold LearningSessionsSelect TeamsBegin PreWorkMeasureProgressTopic and content; model andpractices and the details of theapproach Implementation ofBehavioral Health Home
Develop Charter41Create ChangePackageImplementAction PeriodsDevelopCharterHold LearningSessionsSelect TeamsBegin PreWorkMeasureProgressMission Primary focus of thecollaborative To facilitate and supportimplementation of the PHMstrategyAims Written statements ofexpected accomplishmentsExpectations Commitments to meetduring LC
Select Teams42Create ChangePackageImplementAction PeriodsDevelopCharterHold LearningSessionsSelect TeamsBegin PreWorkMeasureProgressStrategy Leadership and Faculty Strategy and operations design Provide expert facilitators asresources to the quality improvementteams Guide the work through monthlywebinar-style coaching calls Provide technical assistance to careteams Establish aims against which tomeasure the impact of qualityimprovements efforts, track progresstoward the stated aims, and provideaggregate and individual teamfeedback Evaluate the overall impact of thequality improvement effort both atthe organizational level, and at theaggregate level of the entirecollaborative
Study Methods and Design43 Cluster-randomized design withmixed methods approach Models implemented in 11community mental health centers(CMHCs) over two years starting in2013 Research participant inclusion criteria: Medicaid-enrolled 21 years of age Diagnosed with a serious mental illness Receives services at community mentalhealth center within Community Care’snetwork Institute for Healthcare Improvement’sLearning Collaborative Model used tosupport implementation Institute for Healthcare ImprovementBreakthrough Series: http://www.ihi.org
Patient-Centered Outcomes and DataPrimary Data SourcesSecondary Data SourcesSelf-Report Measures(Patient activation,** healthstatus,** hope, quality of life,functional status, satisfactionwith care, social support)HealthChoices Eligibility Data(Medicaid eligibility)Qualitative Data(Service user and providerinterviews)Learning Collaborative(LC) Data(Implementation information)**Primary outcome44Administrative Data(Demographic info)PCORIOptimalHealthParticipantsBehavioral Health Claims(BH diagnosis, utilization)Physical Health Claims(Engagement in primary/specialty care**)Pharmacy Claims(Medication utilization)
Primary Outcomes FindingsPatient Activation More rapid increase in provider-supported sites (with wellness nurse)than self-directed sites Greater increase in activation for women in provider-supported;greater increase for men in self-directedEngagement in Primary/Specialty Care 36% increase in frequency of visits in both study armsHealth Status Small improvement in perceived mental health status Small decline in perceived physical health status45
Qualitative Findings: Patient View Shift in definition of health and wellness,away from vague to more personalized Increased awareness of interconnectednessof mental and physical health Overall favorable intervention experiences No major distinctions between arms – noevident differences in engagement in orsatisfaction with interventions Most important factor leading tointervention participation was relationshipwith wellness coach46
Qualitative Findings: Provider View47 High degree of agency support for wellnesscoaching Culture of wellness that benefitted both serviceusers and providers Models integrated into routine practice Providers simplified/casualized wellness coachingto increase service user engagement Nurses often mentioned as most beneficialcomponent of the model Robustly positive impact on service users’health/wellness Acute needs sometimes trumped wellness coaching Results published f.2017.1115
Trial Data Only: Outcomes Total spending lower with nursepractices in longer term Nurse practices engaging patientsmore with PH services whiledecreasing PH IP BH service use lower with nursepractices, including IP, psychotropicsand TCMNursevs.NavigatorTotalYear 2: PMPM 9%lower Years 1 and 2: PHuse 5% higher Year 2: BH 16%PMPM lower 48 Statistically significant ( 0.05) Suggestive; not quitestatistically significant ( 0.2)*Controlled for baselinedemographics and PMPM
Trial Data Only: OutcomesNursevs.NavigatorIPRx*Controlled for baselinedemographics and PMPMTCMERYear 2:Overall use 23%lower Year 1:PMPM 24% higher Year 1:PMPM 19% lower Year 1:Use 17% lower Years 1 and 2 :PH use and PMPM25% lowerYear 2:Year 2:PMPM 33% lower Years 1 and 2:PMPM lower(19%, 33%) Year 1: BH use 43%lower 49 Statistically significant ( 0.05) Suggestive; not quitestatistically significant ( 0.2)Psychotropic use andPMPM 15% higher
Subsequent Financial Evaluation*Comparison of utilization and otropicsBHBHPMPM(spending per SMI patients enrolled inthe study per month)ERUse(measured by monthlypenetration rate)*These analyses were conducted independent of PCORI-funded contract50
Post-Trial Comparison Group: Outcomes 51Nurse sites have lower long-termspending driven largely by decreasesin behavioral healthNurse Navvs.ComparisonTotalNurse sites have increased PH usebut similar PH cost and less PH IP useNurse sites have less prescription usebut higher prescription costsNurse sites have long-term decreasesin TCM costsYear 2: PMPM15% lower Years 1 and 2: PHuse (40-50%)higher Year 2: BH PMPM20-30% lower Statistically significant ( 0.05) Suggestive; not quitestatistically significant ( 0.2)
Trial Data Only: OutcomesNursevs.ComparisonIPYear 2:Use 30-40% lower and cost 20-25%lower Year 2:PH Use 30-35%lower 52 Statistically significant ( 0.05) Suggestive; not quitestatistically significant ( 0.2)RxYears 1 and 2:Use 25-30% lower Year 1:PMPM 15-20%higher TCMYear 2:PMPM 17% lower ERMatched cohortnot comparablefor ER analysis
BHHP Model arion ColumbiaLuzerne MonroeCentreUnion MontourCarbonSnyder donBerksChesterAdams York53Additional populationsserved: adolescents,opioid treatmentprogramsPopulation Health LCfor mature providersfocused onhypertension andsmoking cessation
PCORI Dissemination AwardContract AwardeeUPMC Center for High-Value Health Care in collaboration with Community CarePurposeDisseminate findings from our recently completed PCORI-funded study to improve the overallhealth and wellness of other priority and high-risk populations Residential Treatment Facilities (n 5) Opioid Treatment Programs (n 7)Contract DurationTwo years (March 1, 2018 – February 2020)Principal InvestigatorJames Schuster, MD, MBA Co-Investigators: Tracy Carney, CPRP, CSP; David Dan, MSW, LCSW; David Loveland, PhD, MA54
GoalsGoal 1Build provider capacity for theconsistent and sustaineddelivery of BHHP Implement and assess thefeasibility of using a LearningCollaborative approach tosupport RTF and OTP teamsto deliver BHHP Assess barriers andfacilitators to LearningCollaborative participationand success55Goal 2Increase service userinvolvement and confidence inmanaging their physical healthand wellnessGoal 3Examine change/trendsover time with BHHPimplementation onengagement inprimary/specialty careand unplanned healthcare utilization
Methods and OutcomesN 20Use a Learning Collaborative 56Model adoptionSustained implementationFidelity to the modelCulture of wellnessImproved staffknowledge/skills/attitudesrelated to wellnessconceptsGather Qualitative DataInterviews (n 20) with providersat the completion of the LearningCollaborativeUse Data to Explore theImpacts and Outcomes Engagement withprimary/specialty care Utilization of unplannedcare (emergencydepartment)
CONTACT INFORMATIONJames Schuster, MD, MBAChief Medical Officer of Medicaid, SNP, and Behavioral ServicesVP, Behavioral IntegrationUPMC Insurance Services Divisionschusterjm@upmc.edu57
Thank You58
pcc
60 UPMC Hillman Cancer Center locations Region's largest network of rehabilitation services More than 4.7 million outpatient visits 41 percent medical-surgical market share in western Pennsylvania Data verified as of July 1, 2018 UPMC HEALTH SERVICES DIVISION UPMC ENTERPRISES UPMC INSURANCE SERVICES DIVISION UPMC INTERNATIONAL