Transcription
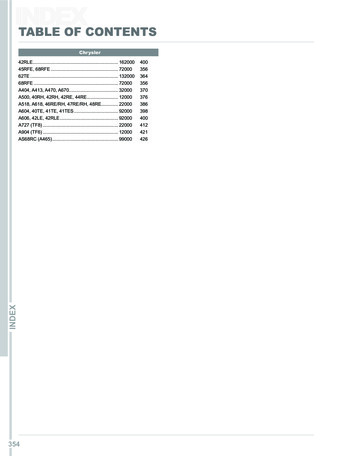
Table of ContentsUpdates to PALS in 2015. 3PALS Systematic Approach . 4First Impression . 4Evaluate-Identify-Intervene . 5Primary Assessment. 6Airway . 6Breathing. 7Circulation . 8Disability . 9Exposure . 9Secondary Assessment and Diagnostic Tests . 10Respiratory Distress/Failure . 11Causes of Respiratory Distress . 12Cardiac Arrest . 14Ventricular Fibrillation and Pulseless Ventricular Tachycardia . 14PEA and Asystole . 15Rapid Differential Diagnosis of Cardiac Arrest . 16Shock . 17Fluid Resuscitation . 18Return of Spontaneous Consciousness (ROSC) and Post Arrest Care . 19Postresuscitation Management . 20Transport to Tertiary Care Center . 21Bradycardia. 22Tachycardia . 23Tachycardia with Pulse and Poor Perfusion . 24Tachycardia with Pulse and Good Perfusion . 25PALS Tools . 26Broselow Pediatric Emergency Tape System . 26PALS Airways . 26Intraosseus Access . 27Team Dynamics/Systems of Care . 28
ECG Rhythms . 29Atrioventricular (Heart) Block . 29Pulseless Electrical Activity and Asystole . 30Ventricular Fibrillation and Pulseless Ventricular Tachycardia . 31Tachyarrhythmias . 32Resuscitation and Life Support Medications . 33
Updates to PALS in 2015As we learn more about resuscitation science and medicine, physicians and researchersrealize what works best and what works fastest in a critical, life-saving situation.Therefore, it is necessary to periodically update life-support techniques and algorithms.If you have previously certified in pediatric advanced life support, then you will probablybe most interested in what has changed since the latest update in 2015. The table belowalso includes changes proposed since the last AHA manual was published.InterventionVolume for children withfebrile illnessAtropine for emergencytracheal intubationArterial blood pressuremonitoringAmiodarone and LidocaineTherapeutic hypothermiaBlood PressureCompressionsUpdates to the 2015 Guidelines2015 GuidelineRestrictive volumes of isotonic crystalloids2010 GuidelineAggressive volume resuscitationControversial for neonates; no minimum doseRoutine premedication prior to intubationIf in place, may be useful to adjust CPRNo guidelineAcceptable for shock-refractory VFib or PulselessVTachFever should be avoided after ROSC but use oftherapeutic hypothermia is controversialFluids and vasoactive agents to maintain systolicblood pressure above the 5th percentile for age100 to 120 per minuteNo guidelineTherapeutic hypothermia should be usedNo guidelineAt least 100 per minute
PALS Systematic ApproachThe PALS systematic approach is an algorithm that can be applied to every injured orcritically ill child.The first step is to determine if the child is in imminent danger of death, specificallycardiac arrest or respiratory failure. The PALS systematic assessment starts with aquick, first impression. The provider or rescuer makes it very quick assessment aboutthe child's condition.Is the child in imminent danger of death? Is there time to evaluate the child to identifyand treat possible causes for the current illness? Is the child conscious? Is shebreathing? What is her color? A conscious child who is breathing effectively can bemanaged in the next steps of PALS, Evaluate-IdentifyIntervene. A unconscious child who is breathing effectively can bemanaged in the next steps of PALS, Evaluate-IdentifyIntervene. A child who is not breathing adequately but who has apulse 60 BPM should be treated with rescuebreathing. A child who has a pulse 60 BPM should be treatedwith CPR and according to the cardiac arrestalgorithm. A child who has a pulse 60 BPM should be treatedwith CPR and according to the cardiac arrestalgorithm.
ify Assuming that the childdoes not need CPR,rescue breathing, ordefibrillation, the nextstep in this systematicapproach in PALS is acircular construct thatincludes evaluation,identification, andintervention. The provider willevaluate, identify, andintervene as many timesas necessary until thechild either stabilizes orher condition worsens,requiring CPR and otherlifesaving measures. “Evaluate” pertains toevaluation of the child'sillness, but also to thesuccess or failure of theintervention. If the child’s condition worsens at any point, revert to CPR and emergencyinterventions as needed. After Spontaneous Return of Circulation (ROSC), use the evaluate–identify–intervenesequence. The evaluate phase of the sequence includes Primary Assessment, SecondaryAssessment, and Diagnostic Tests that are helpful in pediatric life support situations.
Primary Assessment follows ABCDE: Airway, Breathing, Circulation, Disability, Exposure. While CPR currently uses theC-A-B approach orcompressions, airway,breathing, the PrimaryAssessment in PALS still beginswith Airway. If the child airway is open, youmay move onto the next step. However, if the airway is likely to becomecompromised, you may consider a basic or advanced airway. Often, in unresponsive patient or in someone who has a decreased level ofconsciousness, the airway will be partially obstructed. This instruction does not comefrom a foreign object, but rather from the tissues in the upper airway. You canimprove a partially obstructed airway by performing a head tilt and chin lift. If thereis suspected trauma to the cervical spine, use a jaw thrust instead. A blocked airway would usually requires a basic or advanced airway.
The evaluation of breathing include several signs including breathing rate, breathing effort,motion of the chest and abdomen, breath sounds, and blood oxygenation levels. Normalbreathing rates vary by age and are shown in the table. The breathing rate higher or lower thanthe normal range indicates the need for intervention.Normal Respiratory Rate by AgeAgeRangeRate (BPM)0-12 months30-60Toddler1-3 years24-40Preschooler4-5 years22-34School Age6-12 years18-30Adolescent13-18 years12-16InfantNasal flaring, head bobbing, seesawing, and chest retractions are all signs of increased effort ofbreathing. The chest may show labored movement (e.g., using the chest accessory muscles),asymmetrical movement, or no movement at all.Stridor is a high-pitched breath sounds, usually heard on inspiration, that usually indicates ablockage in the upper airway. Rales or crackles often indicate fluid in the lower airway. Rhonchiare coarse rattling sounds usually caused by fluid in the bronchi.Blood oxygen saturation below 90% indicate that an advanced airway, such as an endotrachealtube, is needed. Blood oxygenation can be 100% during cardiopulmonary arrest but should betitrated to between 94 and 99% after ROSC or in non-acute situations.
A heart rate that is either too fast or too slow can be problematic. In children, heart rateless than 60 bpm is equivalent to cardiac arrest. Diminished central pulses, such as inthe carotid, brachial, or femoral arteries, indicate shock. The same is true for capillaryrefill the takes longer than 2 seconds to return, cyanosis, and blood pressure that islower than normal for the child's age. Bradycardia and tachycardia that are interferingwith circulation and causing a loss of consciousness should be treated as cardiac arrestor shock, rather than as a bradycardia or tachycardia.Normal Heart Rate by AgeRangeRate (BPM)0-3 months80-2054 months - 2 years75-1902-10 years60-140Over 10 years50-100Normal Blood Pressure by AgeSystolic RangeDiastolic RangeLow SystolicBlood Pressureby Age1 Day60-7630-45 604 Days67-8435-53 601 month73-9436-56 701-3 months78-10344-65 704-6 months82-10546-68 707-12 months67-10420-60 722-6 years70-10625-65 70 (2 X age)7-14 years79-11538-78 70 (2 X age)15-18 years93-13145-85 90Age
Rapidly assess disability using the AVPU paradigm: Alert, Verbal, Pain, Unresponsive.AVPU , normal activity for the child’s age and usual statusResponds only to voiceResponds only to painDoes not respond to stimuli, even painA more thorough assessment would be the Pediatric Glasgow Coma Scale.Pediatric Glasgow Coma ScaleResponseScoreVerbal ChildPre-verbal ChildEye Opening4SpontaneouslySpontaneously3To verbal commandTo speech2To painTo pain1NoneNone5Oriented and talkingCooing and babbling4Confused but talkingCrying and irritable3Inappropriate wordsCrying with pain only2Sounds onlyMoaning with pain only1NoneNone6Obeys commandsSpontaneous movement5Localizes with painWithdraws when touched4Flexion and withdrawalWithdraws with pain3Abnormal flexionAbnormal flexion2Abnormal extensionAbnormal extension1NoneNoneVerbal ResponseMotor ResponseMild: 13-15Moderate: 9-12Severe: 3-8Exposure is included in the primary assessment to remind the provider to look forcauses of injury or illness that may not be readily apparent. To do this, the child'sclothes need to be removed in a ordered and systematic fashion. During the removal,the provider should look for signs of discomfort or distress that may point to an injury inthat region.The provider should look for and treat, at a minimum, hypothermia, hemorrhage, localand/or systemic infection, fractures, petechiae, bruising or hematoma.
When a child is experiencing an acutelylife-threatening event, such ascardiopulmonary failure, it is appropriateto treat the child with CPR and theappropriate arrest algorithm.When a child has a condition that maysoon become life-threatening or ifsomething does “not feel right”, continueusing the Primary Assessment sequenceof Evaluate-Identify-Intervene. If at anytime the child’s condition worsens, treatthe child with CPR and the appropriatearrest algorithm.Use SAMPLE in Secondary nsPPast HistoryLLast MealDecreased intakeVomiting/DiarrheaBleedingShortness of breathAltered mental statusFussiness/AgitationMedication allergyEnvironmental allergyFood allergyPrescribedOver-the-counterNew meds?Last dose?Birth historyChronic health issuesImmunization statusSurgical historyBreast/bottle/solid?When? What? How much?New foods?History of present illnessOnset/time courseWhen a child is ill but does not likely haveEvents/ExposuresEa life-threatening condition, you mayproceed to the Secondary Assessment. The Secondary Assessment includes a focushistory and focused physical examination looking for things that might cause respiratoryor cardiovascular compromise.The focused physical examination may be quite similar to the Exposure phase of thePrimary Assessment, but will be guided by the data that the provider collects during thefocused history. The focused history will also help determine which diagnostic testsshould be ordered.Key Diagnostic Tests Used in PALSTest/StudyIdentifiesPossible InterventionArterial Blood Gas (ABG)HypoxemiaIncrease OxygenationHypercarbiaIncrease VentilationAcidosisIncrease VentilationAlkalosisReduce VentilationArterial LactateMetabolic acidosis, Tissue hypoxiaShock AlgorithmCentral Venous Oxygen SaturationPoor O2 delivery (SVO2 70%)Shock AlgorithmCentral Venous PressureHeart contractility, othersVasopressors, Shock AlgorithmChest X-rayRespiratory co
The PALS systematic approach is an algorithm that can be applied to every injured or critically ill child. The first step is to determine if the child is in imminent danger of death, specifically cardiac arrest or respiratory failure. The PALS systematic assessment starts with a quick, first impression. The provider or rescuer makes it very .File Size: 2MBPage Count: 35