Transcription
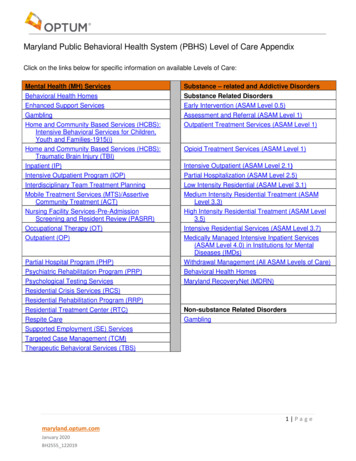
Maryland Public Behavioral Health System (PBHS) Level of Care AppendixClick on the links below for specific information on available Levels of Care:Mental Health (MH) ServicesBehavioral Health HomesEnhanced Support ServicesGamblingHome and Community Based Services (HCBS):Intensive Behavioral Services for Children,Youth and Families-1915(i)Home and Community Based Services (HCBS):Traumatic Brain Injury (TBI)Inpatient (IP)Intensive Outpatient Program (IOP)Interdisciplinary Team Treatment PlanningMobile Treatment Services (MTS)/AssertiveCommunity Treatment (ACT)Nursing Facility Services-Pre-AdmissionScreening and Resident Review (PASRR)Occupational Therapy (OT)Outpatient (OP)Partial Hospital Program (PHP)Psychiatric Rehabilitation Program (PRP)Psychological Testing ServicesResidential Crisis Services (RCS)Residential Rehabilitation Program (RRP)Residential Treatment Center (RTC)Respite CareSupported Employment (SE) ServicesTargeted Case Management (TCM)Therapeutic Behavioral Services (TBS)Substance – related and Addictive DisordersSubstance Related DisordersEarly Intervention (ASAM Level 0.5)Assessment and Referral (ASAM Level 1)Outpatient Treatment Services (ASAM Level 1)Opioid Treatment Services (ASAM Level 1)Intensive Outpatient (ASAM Level 2.1)Partial Hospitalization (ASAM Level 2.5)Low Intensity Residential (ASAM Level 3.1)Medium Intensity Residential Treatment (ASAMLevel 3.3)High Intensity Residential Treatment (ASAM Level3.5)Intensive Residential Services (ASAM Level 3.7)Medically Managed Intensive Inpatient Services(ASAM Level 4.0) in Institutions for MentalDiseases (IMDs)Withdrawal Management (All ASAM Levels of Care)Behavioral Health HomesMaryland RecoveryNet (MDRN)Non-substance Related DisordersGambling1 Pagemaryland.optum.comJanuary 2020BH2555 122019
Public Behavioral Health System (PBHS) Levels of CareThe following information is provided as an overview of the levels of care offered by theMaryland Public Behavioral Health System (PBHS). Complete Medical Necessity Criteria,Guidelines and Policies and Best Practice Guidelines, can be found athttps://optum.maryland.comReturn to Top2 Pagemaryland.optum.comJanuary 2020BH2555 122019
Behavioral Health HomesFor more information on Behavioral Health Homes see .aspx.Who is eligible to receive this service? Who is eligible to provide this service?To enroll as a Health Home, providers must be: enrolled as a Medicaid provider with the State of Maryland licensed as a PRP, Mobile Treatment, or OTP provider accredited, or in the process of seeking Health Homeaccreditation able to meet minimum Health Home staffing requirements able to provide Health Home services and meet specifiedreporting requirementsHealth Homes is available to Medicaid beneficiaries whohave been diagnosed with:- SMI and are currently receiving PRP or MT services- SED and are currently receiving PRP or MT services- an Opioid SUD and are at risk for additional chronicconditions due to the following risk factors:o Current alcohol, tobacco, or other non-opioidsubstance useo History of alcohol, tobacco, or other non-opioidsubstance dependenceEligibility Reminders Individuals receiving the following services are excluded from Health Home eligibility:- Services via 1915i SPA- Targeted Mental Health Case ManagementAuthorization RemindersFor current information on authorizations please see Requirement-Information.aspxDischarge Reminders Discharge from the Health Home primarily results from incidents such as relocation or loss of MedicaideligibilityIf a participant is discharging from Health Homes due to stabilization, the participant may remain in theprogram for six months. During the six month period, the provider is responsible for constructing adischarge plan designed to support the participant’s transition into the appropriate level of care.Return to Top3 Pagemaryland.optum.comJanuary 2020BH2555 122019
Mental Health – Enhanced Support ServicesWho is eligible to receive this service? Who is eligible to provide this service? Medicaid ParticipantsMaryland Public Behavioral Health System (PBHS) eligibleMedicare recipientsUninsured Eligible Participants with eligibility span for PRP,RRP, MTS (includes Medicare and State Funded Medicaidparticipants)Enhanced support services can only be provided byapproved Psychiatric Rehabilitation Programs (PRP),Residential Rehabilitation Programs (RRP), and MobileTreatment Services (MTS)Authorization Reminders Prior authorization is requiredProviders must submit a prior authorization request via Provider ConnectThe Core Service Agency (CSA) or Local Behavioral Health Authority (LBHA) reviews requests andmakes determinationsIf a CSA or LBHA Care Manager is unable to authorize the service as medically necessary, the requestfor services will be referred to a CSA or LBHA Physician Advisor for reviewDeterminations will be communicated via Provider ConnectService Remindersnhanced support services: will be provided in the participant's place of residence are not available for participants in inpatient facilities, residential treatment center (RTC) settings, orpartial hospitalization programs (PHPs) are considered short-term and will be reimbursed for a maximum of 10 days per episode/30 days percalendar year cannot be authorized in conjunction with respite services do not cover the provision of personal care services, which may be reimbursable by Medicaid undera separate funding authority are not available for individuals who meet criteria for a Medicaid Home and Community BasedWaiver (e.g., DDA Community Pathways Waiver, TBI Waiver, Community Options Waiver Community First ChoiceBilling Reminders A unit of enhanced support Services is one hour of servicesThe number of units must equal the number of hours enhanced support services were provided (e.g. oneunit one hour, six hours six units)Each day of service must be on a separate claim form line, and claims must specify an ICD-10 code, notDSM 5 codeReturn to Top4 Pagemaryland.optum.comJanuary 2020BH2555 122019
Gambling ServicesWho is eligible to receive this service? Who is eligible to provide this service? All Maryland residents, regardless of insurance coverage type.This includes: Medicaid eligible, Medicaid ineligible, uninsuredor privately insuredParticipants must be a Maryland residentParticipants may be individuals with problem gambling, and/orloved ones/ concerned othersProviders eligible for reimbursement of this service must beeither a private practitioner (individual or group) or acommunity-based providerPrivate practitioners must be in good standing with theappropriate professional board(s)Community-based providers must either be a FederallyQualified Health Center or licensed in accordance withCOMAR 10.63 as a substance use, mental health orintegrated behavioral health program at the following levels ofcare:- Ambulatory SUD programs for Level 1 and Level 2.1- Residential SUD programs for Level 3.1, 3.3, and 3.5- Outpatient Mental Health Clinics (OMHC)- Mental Health Intensive OutpatientMaryland Center of Excellence on Problem Gambling Private practitioners and community-based providers must ensure the staff is trained and competent toprovide services to individuals with problem gambling and/or loved ones/ concerned othersThe Maryland Center of Excellence on Problem Gambling is available to provide problem gamblingtraining and clinical consultation at no cost to programsProviders may contact the Center of Excellence on Problem Gambling at www.mdproblemgambling.comor at (667) 214-2120 for further informationProvider InformationMedicaid Providers Providers already enrolled in Maryland Medicaid and registered with OptumPlease register with Maryland Center of Excellence on Problem Gambling:- Apply through the Maryland Center of Excellence on Problem Gambling’s (COE) website g-treatment-reimbursement-application/- An acknowledgement of receipt of the application will be provided to the applicant- Following a review of the application information by Center clinical staff, a confirmation notice ofenrollment will be sent to the provider. The provider may then register with Optum ProviderConnect- Once approved, the provider may also complete the Provider Referral registration formhttps://is.gd/DGProviderReferral in order to be included in the Provider Referral Directory postedon the Center’s website and used for referrals from the 1-800-GAMBLER Helpline.Non-Medicaid Providers Providers do not need to be enrolled with Medicaid, and should not enroll with Medicaid if they are onlyseeking reimbursement for gambling services and do not wish to provide any other Medicaid reimbursed5 Pagemaryland.optum.comJanuary 2020BH2555 122019
servicesProviders that are not enrolled, and do not wish to become enrolled, with Maryland Medicaid shouldfollow the approval process detailed below. Please follow the approval process below before registeringwith Optum Provider Connect:- Apply through the Maryland Center of Excellence on Problem Gambling’s (COE) website g-treatment-reimbursement-application/- An acknowledgement of receipt of the application will be provided to the applicant.- Following a review of the application information by Center clinical staff, a confirmation notice ofenrollment will be sent to the provider. The provider may then register with Optum ProviderConnect.- Once approved, the provider may also complete the Provider Referral registration formhttps://is.gd/DGProviderReferral in order to be included in the Provider Referral Directory postedon the Center’s website and used for referrals from the 1-800-GAMBLER HelplineAuthorization Reminders Initial and concurrent authorization requests can be requested via Provider Connect.Only the following diagnosis are eligible for gambling services:- Mental Health: F63.0 Pathological Gambling- Substance Use (SGAM): F63.0 Pathological Gambling Z72.6 Gambling and Betting Problems related to Lifestyle Z71.9 Counseling unspecifiedElectronic authorizations are completed by the provider through submission of up to date clinicalinformation in Provider Connect for members registered with the SGAM fund and allowable covereddiagnoses. When reviewing the eligible fund sources, a provider should review the participant file for theSGAM funding source. If the provider does not see SGAM listed on the participants file, they will need toregister the participant through the Provider Connect site under Member Registration. On this screen youwill see a section marked Requested Services and should check the box marked Gambling Services.This will register the participant for this eligible funding source for up to one year.Upon discharge, the provider must discharge the participant from their service by going to ProviderConnect and entering a discharge. Providers should note that entering discharge information is animportant step and is reimbursable.Return to Top6 Pagemaryland.optum.comJanuary 2020BH2555 122019
Mental Health – Home and Community Based Services (HCBS):Intensive Behavioral Services for Children, Youth and Families – 1915(i)Who is eligible to receive this service? Who is eligible to provide this service? Medicaid Participants, under 18 years of age at time ofenrollment.Additional clinical and financial eligibility criteria also apply, perCOMAR 10.09.89.03.Termination of enrollment, for a variety of conditions, is alsodescribed in COMAR 10.09.89.04.Services may only be provided by approved 1915(i) serviceproviders whose eligibility has been verified by the MarylandDepartment of Health (MDH) according to the process outlinedin COMAR 10.09.89.08.Eligibility Reminders1. Age:a. Youth must be under 18 years of age at the time of enrollment although they may continue in1915(i) HCBS benefit up to age 22.2. Residence:a. Youth must reside in a home and community-based setting.b. Youth must reside in one of the geographic areas where the 1915(i) HCBS benefit is availablec. Excluded community programs in which a youth may not reside while receiving the HCBS 1915(i)benefit are: group home; psychiatric respite care facility located on the grounds on an IMD for thepurpose of placement; residential program for adults with serious mental illness licensed underCOMAR 10.21.22.3. Consent:a. Youth under 18 must have consent from the parent or legal guardian to participate; for youngadults who are 18 or older and already enrolled, the young adult must consent to participate.b. Youth over 18 who are in the care and custody of the State, require consent from their legalguardian.4. Behavioral Health Disorder:a. Youth must have a behavioral health disorder amenable to active clinical treatment. Theevaluation and assignment of a DSM diagnosis must result from a face-to-face psychiatricevaluation that was completed or updated within 30 days of submission of the application toOptum.b. There must be clinical evidence the child or adolescent has a serious emotional disturbance andcontinues to meet the service intensity needs and medical necessity criteria for the duration oftheir enrollment. Because of the clinical requirement that the young person have a seriousemotional disturbance, it will be required for the young person to be actively involved in ongoingmental health treatment on a regular basis in order to receive 1915(i) HCBS benefit services.5. Impaired Functioning & Service Intensity:a. A licensed mental health professional must complete a comprehensive psychosocial assessmentwithin 30 days of the submission of the application to Optum. The psychosocial assessment mustoutline how the youth’s functioning presents potential danger to self or others, across settings,including the home, school, and/or community. The serious harm does not necessarily have to beof an imminent nature.b. The psychosocial assessment must support the completion of the Early Childhood ServiceIntensity Instrument (ECSII) for youth ages 0-5 or the Child and Adolescent Service Intensity7 Pagemaryland.optum.comJanuary 2020BH2555 122019
Instrument (CASII) for youth ages 6-21.c. Early Childhood Service Intensity Instrument (ECSII)i.Youth must receive a score of 4 (High Service Intensity) or 5 (Maximal Service Intensity)ii.Youth who are younger than six years old who have a score of 4 on the ECSII must: Be referred directly from an inpatient hospital unit-or If living in the community, have two or more psychiatric inpatient hospitalizations in thepast 12 monthsd. Child and Adolescent Service Intensity Instrument (CASII)i.Youth must receive a score of 5 (Non-Secure, 24-Hour, Medically Monitored Services) or6 (Secure, 24- Hours Medially Managed Services)ii.Youth with a score of 5 on the CASII also must meet one of the following criteria to beeligible based on their impaired functioning and service intensity level: Transitioning from a residential treatment center (RTC) Living in the community and: If 13 years old or older, have:- Three or more inpatient psychiatric hospitalizations in the past 12 months-or- Resided in an RTC within the past 90 days If ages 6 through 12 years old and have:- Two or more inpatient psychiatric hospitalizations in the past 12 months-or- Resided in an RTC within the past 90 daysYouth will not be eligible for HCBS services if they meet any of the following criteria. Youth:- is hospitalized for longer than 30 days.- moves out-of-state for more than 30 days.- moves out of a geographic area within the state of Maryland where the youth cannot reasonablyaccess services and supports during the initial phase-in of the 1915(i) HCBS benefit.- is admitted to and placed in an RTC for longer than 60 days.- is admitted to and placed in a group home setting licensed under COMAR.- is placed in a psychiatric respite care program, a non-medical group residential facility located on thegrounds of an IMD primarily for the purpose of placement.- losses eligibility for Maryland Medicaid for more than 30 days.- turns 22 years old.- is detained, committed to a facility, or incarcerated for longer than 60 days.- has annual medical review that does not meet medical re-certification criteria.- has no CFT meeting held within 90 days.- is no longer actively engaged in ongoing mental health treatment with a licensed mental healthprofessional.Available ServicesIntensive behavioral health services are provided by a program approved and operated under the provisionof COMAR 10.09.89 and are provided in the participant’s home or in an approved community-basedsetting.Services are designed to support the participant remaining in their homes by providing a8 Pagemaryland.optum.comJanuary 2020BH2555 122019
wraparoundservice delivery model. Services can include:Care Coordination Organization (CCO) – provides case management services to 1915(i) participantsand families as described in COMAR 10.09.90.Child and Family Team (CFT) - a team of participants selected by the participant and family to workwith them to design and implement a plan of care.Intensive In-Home Services (IIHS) - strengths-based interventions with the youth and their family thatinclude a series of components described in COMAR 10.09.89.14.Mobile Crisis and Stabilization – services offered in response to urgent mental health needs and areavailable on a short-term basis, 24-hours per day, seven days per week. These services are coordinatedwith the CCO and CFT; and are incorporated in the participant’s plan of care.Community-Based and Out-of-Home Respite Care – services offered to provide stabilization and reliefto caregivers from the stress of care giving. These services may be provided in the home or community.In-home services offer additional temporary support, in the home and overnight. Out-of-home respiteservices provide a temporary overnight living.Peer-to-Peer Support - services are offered to ensure that family and participant opinions andperspectives are incorporated into the CFT process and plan of care. Services are provided by a familysupport organization (FSO) as described in COMAR 10.09.89.10.Expressive and Experiential Behavioral Services - use of art, dance, music, equine, horticulture ordrama to accomplish individualized goals as part of the plan of care. Services may be providedindividually or in a groupCustomized goods and services - expenditures requested COMAR 10.09.89.09.Behavioral Health Consultation – services to health care professionalsAuthorization Reminders Initial and concurrent authorization for services should be requested via Provider Connect.An initial assessment session (via mobile crisis services) is pre-approved for all participants and shouldbe completed within the first week of CCO services to develop a crisis response plan. Subsequent to acrisis, services are pre-approved for up to a three-day stabilization period. Additional services requirefurther documentation, review, and prior authorization.To obtain authorization for 1915(i) services, the CCO, working with the participant and family, mustrequest a prior authorization. The clinical information required consists of the list of applicable DSM 5diagnoses and the current need for requested service. The description of the requested services shouldbe identified in the participant’s individualized plan of care. The plan of care should be developedthrough the CFT process.Applicants shall have a face-to-face, psychiatric evaluation completed within 30 days of the submissionof the enrollment application.IIHS, community-based respite services and in-home respite services are automatically authorized for 60days. Thereafter, the services will be authorized in six-month increments.Peer-to-peer support services are automatically authorized for one year. Thereafter, the services will beauthorized in six-month increments.A prior authorization request is required for any additional mobile crisis and stabilization, expressive andexperiential behavioral services, and customized goods and services.Return to Top9 Pagemaryland.optum.comJanuary 2020BH2555 122019
Mental Health – Home and Community Based Services (HCBS):Traumatic Brain Injury (TBI)Who is eligible to receive this service? Who is eligible to provide this service? Technical, medical, and financial eligibility for the program isestablished in COMAR 10.09.46Technical eligibility is based on the type of injury, age at injury,and location where the applicant is residing.Technical eligibility is limited to an individual with a TBI that hasoccurred after the age of 21 who is in a state psychiatrichospital, an out-of-state placement funded through MarylandMedicaid, a state-owned and operated nursing facility, or achronic hospital that is CARF accredited for inpatient braininjury rehabilitation.Services may only be provided by approved 1915(i) serviceproviders whose eligibility has been verified by the MDH)according to the process outlined in COMAR 10.09.89.08.Available ServicesThe following four services are available through the TBI Waiver:1. Residential Habilitation: Residential habilitation services provide participants assistance withacquisition, retention, or improvement in skills related to activities of daily living (ADLs) and the socialand adaptive skills necessary to enable the individual to live in a non-institutional setting. The servicesprovided in a residential program are provided and reimbursed at one of the following three levels ofservice, as preauthorized in the participant’s waiver plan of care approved by the Behavioral HealthAdministration (BHA):a. Level 1 requires a staff to participant ratio of 1:3, at a minimum, during day and evening shifts andnon-awake supervision during an overnight shift or an awake staff person covering more than onesite during the overnight shift.b. Level 2 requires a staff to participant ratio of 1:3, at a minimum, during day and evening shifts andawake, onsite supervision during an overnight shift.c. Level 3 requires a staff to participant ratio of 1:1 during day and evening shifts and awake onsitesupervision during an overnight shift.2. Day Habilitation: Day habilitation services provide participants with assistance with acquisition,retention, or improvement in self-help, socialization, and adaptive skills which takes place in a nonresidential setting, separate from the home or facility in which the individual resides, normally furnishedfour or more hours per day. The services provided in a day habilitation program are provided andreimbursed at one of the following three levels of services, as pre-authorized in the participant’s waiverplan of care approved by BHA:a. Level 1 requires a staff to participant ratio of 1:6, at a minimum.b. Level 2 requires a staff to participant ratio of 1:4, at a minimum.c. Level 3 requires a staff to participant ratio of 1:1, at a minimum.3. Supported Employment: Supported employment services include activities needed to support paidwork by individuals receiving waiver services, including supervision and training. The services areprovided and reimbursed at one of the following three levels of service, as pre-authorized in theparticipant’s waiver plan of care approved by BHA:a. Level 1 requires staff members to provide daily contacts to the waiver participant.b. Level 2 requires staff members to provide a minimum of one hour of direct support per day.10 P a g emaryland.optum.comJanuary 2020BH2555 122019
c. Level 3 requires staff members to provide continuous support for a minimum of four hours ofservice per day.4. Individual Support Services: Individual support services means assistance provided to an individual toenable them to fully participant in the community. This may include, but not be limited to, supportsinvolving:- Budgeting- Medication administration- Counseling- Helping an individual to access and complete his or her education- Participation in recreational and social activities- Accessing community services- Grocery shopping- Behavioral and other services and support needed by the family of the individual- Developing relationshipsAuthorization Reminders TBI Waiver services are authorized, and must be approved by, BHA’s Office of Older Adults and LongTerm Services and Supports in accordance with COMAR 10.09.46.Return to Top11 P a g emaryland.optum.comJanuary 2020BH2555 122019
Mental Health - Inpatient (IP)Who is eligible to receive this service? Medicaid ParticipantsWho is eligible to provide this service? Hospitals licensed and regulated by the state of Maryland thatare approved Medicaid providers are eligible forreimbursement for services.Hospitals located outside the state of Maryland, who possessan active Maryland Medicaid provider number, and who aretreating psychiatric emergencies, are also eligible forreimbursement. Authorization Reminders: Providers are expected to submit the authorization request, with supporting clinical information, the dayof admission but no later than 24 hours, or one calendar day from date of admission.Crisis services, hospital diversion programs, or CSA or LBHA crisis response systems will be exploredprior to admission, when applicable, and available in the area.Concurrent authorization requests should be submitted via Provider Connect with supporting clinicalinformation on the first uncovered day. For example, after an initial authorization span of March 1st toMarch 4th, if needed, the continued stay request should be submitted on March 4th.A courtesy review can be requested for uninsured participantsDischarge/Aftercare Planning Providers are expected to initiate discharge planning at the beginning of service delivery. A dischargeplan should be included with the authorization requestProviders are responsible for entering a discharge when the participant completes treatment.The day of discharge is not a reimbursable day for the hospital. For example, if the participant is admittedon March 1st at 11:45 p.m., March 1st is a covered day. If the participant is discharged on March 4th at4:00 p.m., March 4th is not a reimbursable day. March 3rd would be considered the last day covered.Billing Reminders: During an IP stay, Maryland PBHS will cover and pay for diagnostic testing and consultations that arerelated to the psychiatric treatment of the participant.Only one psychiatric professional fee from a psychiatrist or nurse practitioner, per psychiatric IP day iscovered. An additional authorization for professional fees is not needed.Non-psychiatric physicians or nurse practitioners will be reimbursed by the Maryland PBHS for onehistory and physical per admission, and authorization is not required.Administrative days are used when a participant no longer meets medical necessity criteria for apsychiatric IP unit and requires discharge to a nursing home or residential treatment center, however, abed is not yet available. Administrative days are paid at a lower rate than a regularly authorized IP day.Return to Top12 P a g emaryland.optum.comJanuary 2020BH2555 122019
Mental Health – Intensive OutpatientWho is eligible to receive this service? Who is eligible to provide this service? Medicaid ParticipantsDual Participants (Medicare/Medicaid)Partial hospitalization programs (PHP) (Psychiatric DayTreatment Programs (PDTP)) approved under COMAR10.63.03.08 and OMHCs approved under COMAR 10.63.03.05may provide IOP services.Authorization Reminders Initial and concurrent authorization requests can be requested via Provider Connect or telephonically.Service Reminders Services for participants with co-occurring needs should be integrated and individualized to meet theneeds of the participant.Billing Reminders One day equals one unit, date spans will not be accepted.When IOP is provided by:- an OMHC, physician services are included in the rate- a hospital-based program, physician services may be billed separately.It is considered duplicative to bill two IOP units for the same participant/same day (i.e. substance useIOP and mental health IOP).The MarylandPBHS does not reimburse for non-mental health services such as 12-step programs.Return to Top13 P a g emaryland.optum.comJanuary 2020BH2555 122019
Mental Health – Interdisciplinary Team Treatment Planning ServiceWho is eligible to receive this service? Who is eligible to provide this service? Medicaid ParticipantsUninsured Eligible ParticipantsInterdisciplinary team treatment planning meetings are providedby OMHCs approved under COMAR 10.63.03.05.Authorization Reminders Authorization for this service is not required.Service Reminders This service is only available for OMHCs.A participant may receive up to two interdisciplinary team treatment planning meetings per calendar year.The participant is actively engaged in this process and must sign agreement with the plan.If the participant is unwilling to sign agreement with the plan, the participant’s treatment coordinator willverify the participant’s verbal agreement with the plan and document the rationale for the participant’srefusal to sign.If the participant is a minor, the minor’s parent or guardian, or the minor’s primary caretaker, must signagreement with the plan. With proper consent, family or others designated by the participant, includingthe participant’s caregivers, may sign the plan.The plan should include the participant’s diagnosis, presenting needs, strengths, recovery and treatmentexpectations and responsibilities. Descriptions of treatment and interventions to be provided, as well as adescription of how identified treatments will help the participant manage the psychiatric disorder andsupport recovery, should also be included. Measureable short-term and long-term treatment goals shouldbe documented, including targeted completion dates for each goal.At least two licensed mental health professionals who collaborate about the par
1 Page maryland.optum.com January 2020 BH2555_122019 . Maryland Public Behavioral Health System (PBHS) Level of Care Appendix