Transcription
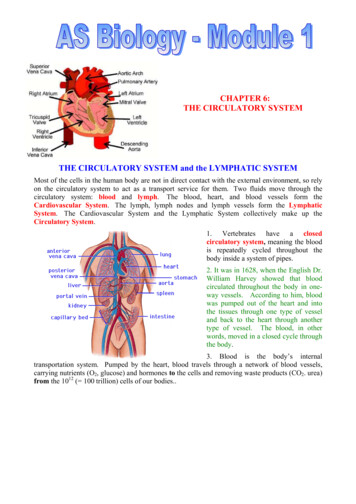
2/18/2021Cardiac Rehabilitation: IntroductionCR is comprehensive long-term servicesinvolving:Cardiac RehabilitationM. Wesley Milks, MD, FACCAssistant Professor of Internal Medicine - ClinicalMedical Director, Cardiac Rehabilitation Outpatient Care Upper ArlingtonAssociate Program Director, Cardiovascular Disease FellowshipDivision of Cardiovascular Medicine, Department of Internal MedicineThe Ohio State University Wexner Medical CenterOutline Indications for cardiac rehabilitation Scope of cardiac rehabilitation programs Exercise testing and prescription Medical evaluation Prescribed exercise Cardiac risk-factor modification Health education Counseling Behavioral interventionsWenger NK, et al. [NHLBI Clin Pract Guidel No. 17]. Clin Pract Guidel Quick Ref Guide Clin. 1995 Oct;(17):1-23.Stock photo was purchased from istock.com by the Ohio State Heart & Vascular Center.Team irector)Nurses /CaseManagersRegisteredDieticians1
2/18/2021Indications for cardiac rehabPer CMS (Medicare Part B) guidelinesIschemicHeart DiseaseValvularHeart Disease Acute MIwithin 12 mo. CABG surgery PCI/stent Stable anginapectoris Heart valverepair Heart valvereplacement(incl. TAVR)Heart FailurePhases of Cardiac RehabPhase I In-hospital Goals of education, early ambulation, andencouragement of referral to phase IIPhase II 12-week intensive outpatient program Goals Return to work, hobbies, lifestyle Improved QOL / perception Anxiety and depressionmanagement Risk factor modification Tobacco use cessationPhase III Long-term maintenance (no ins.coverage) Hearttransplantation Chronic heartfailure*SymptomaticPeripheral Artery DiseaseShifting paradigms in CR*Added 2014.LVEF 35%, NYHAClass II‐IV symptomsdespite GDMTtolerated x 6 wkwithout major CVhospitalizations orprocedures.Fitness, Activity, ExercisePhysical FitnessTraits thatallow forability to lityExerciseOLDvs.NEWPhysical ActivitySkeletalmuscleactivityEnergyexpenditure baselineE.g. chores,walksExerciseSubset ofphysical activitythat is planned,structured,repetitivePurpose is toimprove 1 component ofhealth-relatedphysical fitnessExercise Prescription Modules: Assessment, Evaluation, and Best Practices. AACVPR 2016.Stock photo was purchased from istock.com by the Ohio State Heart & Vascular Center.2
2/18/2021Exercise Testing & PrescriptionExercise: Is it Safe?Contraindications to exercise (selected)Absolute Unstable angina / ACS Acute myocarditis Uncontrolled arrhythmias Severe/decompensated valvedisease / HF Severe resting hypertension (e.g. 200/110 mmHg) Acute pulmonary embolism Acute non-cardiac illness Physical disability renderingexercise unsafe Ratio of oxygen uptake by thebody at a given activity level toresting oxygen uptake by thebody 1 MET 3.5 ml[O2]/kg/min Equivalent to 58.2 W/m2 BSA, or about100 W for a standard 1.73 m2 individual Sleep: 0.9 METs sleeping Extreme exercise: 23 METs running a4:17 mileStock photo was purchased from istock.com by the Ohio State Heart & Vascular Center.Relative Electrolyte abnormalities Arrhythmias / high gr. AVB Hypertrophic cardiomyopathywith LVOTO 25 mmHg Known significant left maincoronary artery stenosis Asymptomatic severe AS Cognitive impairment orpsychiatric diseaseAdapted from: Henzlova MJ, et al. J Nucl Cardiol 2016 Jun;23(3):606-39.Exercise TestingExercise PrescriptionParameters assessed Routine Heart rate, rhythm Blood pressure Symptoms; rating of perceived exertion(RPE)SpeedGrade Oxygen saturationOxygen consumptionVentilatory/lactate thresholdVE/VO2 slopeCO2 productionExhaustionHenzlova MJ, et al. J Nucl Cardiol 2016 Jun;23(3):606-39.Workload bytime and stageDuration OptionalExercise Prescription Modules: Assessment, Evaluation, and Best Practices. AACVPR 2016.3
2/18/2021Exercise ResponsesExercise ResponsesTime toexhaustion( /‐)VO2max,VE/VO2slope, aburdenResting EKG abnormalitieswhich reduce test accuracy LVH LBBB Ventricular pacing Resting ST-depression 0.5 mm Digitalis effectMagnitude/Henzlova MJ, et al. J Nucl Cardiol 2016 Jun;23(3):606-39.Exercise Prescription Modules: Assessment, Evaluation, and Best Practices. AACVPR 2016.Intensity of Exercise Absolute predicted maximal heart rate method HRmax 220 – [age] Entry to CR: may be approximately 50% x HRmax, dependingon level of conditioning Exercise goal and prescription: target HR of 60-85% xHRmax Karvonen (proportion of HR reserve) method Target HR 0.5 to 0.8 * (HRmax – HRrest) HRrest Oxygen consumption method Exercise at 60-80% of maximal oxygen consumptionBraverman DL et al. Am J Phys Med Rehabil 2011;90:599-611.time of ST Adapted from: Henzlova MJ, et al. J Nucl Cardiol 2016 Jun;23(3):606-39.Exercise PrescriptionKarvonen (Heart Rate Reserve) MethodExercise Prescription Modules: Assessment, Evaluation, and Best Practices. AACVPR 2016.4
2/18/2021Exercise Testing & Rx.Exercise s1.0 - 1.5Easy walking1.6 - 2.9 40% 123.0 - 5.940 – 59%12 – 136.0 – 8.860 – 90%14 – 17Above 90%18 – Rating ofRange ofHR or VO2max PerceivedreserveExertionIntensityBrisk walking(4 mph)Household choresJoggingMoving furnitureFastest running,cycling, rowingCreating an Exercise Prescription: FITT(VP) principleFIFrequencyNumber of sessions/wk.Most days of the week recommended for allIntensityLevel of exertion: most potent stimulus forimproved fitness. May be relative or objective(e.g. METs, %maxHR, %VO2max)TT(V)(P)TimeTime spent per exercise session5‐10 min warm up, cool‐downTypeType of exercise, e.g. walking, jogging, cycling,weightliftingVolumeE.g. moderate 150 mins/wk;vigorous 75 mins/wkProgressionE.g. increase duration by 5 min/session every 1‐2weeks until reaching goal (e.g. 30m)Exercise Prescription Modules: Assessment, Evaluation, and Best Practices. AACVPR 2016.Exercise Prescription Modules: Assessment, Evaluation, and Best Practices. AACVPR 2016.Exercise PrescriptionSpecial ConsiderationsOsteoarthritis Emphasis onflexibility Lightmoderateintensity 150 min/wkrecommendedbut may need tooccur in shorterboutsReturn to Sexual ActivityAHA Scientific Statement on Sexual Activity and Cardiovascular Dis.Diabetesmellitus Moderate tovigorousintensity Suggest notgoing 2 consecutivedays withoutphysical activitydue to glycemiccontrol benefits ConsiderglucosemonitoringHeart Failure Emphasis onaerobic activity metricactivity)Exercise Prescription Modules: Assessment, Evaluation, and Best Practices. AACVPR 2016. Risk of coital MIis elevated insedentaryindividuals (RR3.0) vs.physically activeindividuals (RR1.2). Sexual activityis the precipitantof 1% of allacute MIsPrior toresumption ofsexual activityLevin GN et al. Circulation 2012;125:1058-1072.Evaluate withEvaluate with H&P(IIa, C)H&P (IIa, C)PerformexercisePerform exercisestress testingstresstestingforforthoseat atelevatedriskthoseelevatedor have unknown ex.risk capor haveunknownex. cap(IIa, C)(IIa, C)Resumption ofsexual activityis reasonableLowLow riskrisk ationseval.clinicalon clinical eval(IIa, B)AbilitytotoexerciseexerciseAbility 3 3toto5 5METsMETswithoutwithoutangina, excessiveexcessiveangina,dyspnea, ST or BPdyspnea,ST drop (IIa,C) orBP drop (IIa, C)Defer mpensated,severe symptomaticsevereCVDsymptomatic(III, C)CVD (III, ipitatedbyprecipitated bysexual(III,(III,C)sexualactivityactivityC)5
2/18/2021ConclusionsBenefits of Cardiac RehabExercise capacity Expect 33% increase in tolerated METs Increased VO2max by 16%Improved symptom burden Decreased dyspnea or angina Decreased BP/HR for given workloadImproved prognosis Improved cardiovascular mortality (OR 0.74) Improve all-cause mortality (OR 0.80)Potential risks: Arrhythmias (AF, VT) Inappropriatedefibrillation (considerwaiting 6 wk post ICDimplant to avoid leaddislodgement) Death: 1/60,00080,000 hrs supervisedexercise Cardiac rehab is acomprehensivesecondary preventionprogram Safe return to physicalactivity is key in promotingrecovery & wellness Risk factor modificationcan reduce risk of recurrenteventsBraverman DL et al. Am J Phys Med Rehabil 2011;90:599-611.Stock photo was purchased from istock.com by the Ohio State Heart & Vascular Center.OutlinePulmonary Rehabilitation Definition/BackgroundPhysiologic rationaleProgram componentsOutcomesRehab in non-COPD settingsPhilip T. Diaz, MDProfessor of Internal MedicineMedical Director of Pulmonary RehabilitationThe Ohio State University Wexner Medical Center6
2/18/2021Which of the following intervention is likely toprovide the greatest improvement in her shortnessof breath?– 59 y.o. female with COPD– Long standing dyspnea with minimal exertion– No acute exacerbations in the last year– On daily umcledinium/vilanterol (Anoro); prn albuterol– FEV1 – 0.52 liters, 26% of predicted– Residual volume 199% predCombination inhalers for COPD ICS/LABA LAMA/LABA– Umeclidinium/Vilanterol Anoro– Tiotropium/Olodaterol Stiolto– Glycopyrrolate/Formoterol Bevespi– Glycopyrrolate/indacaterol Utibron– Fluticasone/Salmeterol Advair– Budesonide/Formoterol Symbicort– Mometasone/Formoterol Dulera– Fluticasone/Vilanterol Breo1. Replace Anoro with twice dailybudesonide/formoterol (Symbicort)2. Add Roflumilast (Daliresp)3. Replace Anoro with dailyUmeclidinium/Vilanterol/Fluticasone (Trelegy)4. Pulmonary rehabilitation.Dyspnea ScaleVery severeSevereModerateBronchodilatorsOxygenExercise trainingSlightVery slightLAMA/LABA/ICS- Umeclidinium/Vilanterol/Fluticasone TrelegyGlycopyrrolate/Formoterol/Budesonide BreztriEndurance Exercise TimeAdapted from Am J Respir Crit Care Med 19997
2/18/2021Pulmonary RehabilitationPR – Historical Perspective“A comprehensive intervention based on a thoroughpatient assessment followed by patient tailoredtherapies that include but are not limited to exercisetraining, education and behavioral change designedto improve the physical and psychological conditionof people with chronic respiratory diseases and topromote the long-term adherence to healthenhancing behaviors.” Originally described 1960’s by Barach Advanced by Petty in 1970’s Remained controversial as a treatmentuntil mid-1990’sAmerican Thoracic Society/European Respiratory Society, 2013Which of the following pulmonaryphysiologic parameters is consistentlyimproved following pulmonaryrehabilitation?A.B.C.D.E.FEV1FVCPO2Oxygen saturation during exerciseNone of the aboveOutline Definition/BackgroundPhysiologic rationaleProgram componentsOutcomesRehab in non-COPD settings8
2/18/2021Airflow obstruction in COPDSmall airways disease –obstructive bronchiolitisSmall airway inflammationand narrowingEmphysema – tissuedestructionHyperinflation and respiratorymuscle weaknessLoss of elastic recoil“Drivingpressure”Shorter muscle length - less actin, myosin overlapDecreased zone of appositionNormalEmphysemaDynamic hyperinflation in COPDSystemic effects of COPDPulmonary inflammationCOPDSystemic “spillover” ofinflammatory mediatorsCoronary artery diseaseNormalOsteoporosisSkeletal muscle dysfunctionAnemiaEnd expiration9
2/18/2021Impaired oxygen utilization in skeletalmuscles of patients with COPDA. Decreased capillary densityB. Decreased type I muscle fibersC. Decreased oxidative enzyme activity inmitochondria Reduction in citrate synthase – criticalenzyme in Krebs cycle and metabolismof oxygen Citrate synthaseCitrate synthase activityactivity issignificantly50decreased in thevastus lateralismuscle of COPDpatients. Maltais et al25COPD10Correlation of citrate synthase activity andfunctional status in COPDRationaleMaltais et. al. Thorax 2000Deconditioning Least functional patientshave lowest citratesynthase activitiesNL2000; ThoraxMalnutritionInflammatorycytokines DYSPNEA pCO2 Lactic acidEarlier onset anaerobic metabolismHypoxemia/hypercarbia Mitochondrial oxidative enzymes Capillary densityFunctionalClass 4FunctionalClass 1 % Type I fibers10
2/18/2021COPD vicious cycleIncreased load anddecreasedefficiency ofrespiratory musclesHyperinflation/airflow obstructionCOPDImprovement in citrate synthase with rehabPre-rehabAnxiety/DepressionIncreased lactate productionduring exerciseDyspnea on exertionSystemicinflammationDecreased oxidativecapacity of skeletalmuscle enzymesCitrateSynthase22.3 /- 3.5Post-rehab25.8 /- 3.8(Maltais et al 2000)P value 0.05DeconditioningReductions in exercise lactic acidosis andventilation as a result of exercise training inpatients with obstructive lung disease.Casaburi et al Am Rev Respir Dis 1991Lactate (mEq/L)Pre-rehab6Post-rehab4Outline Definition/BackgroundPhysiologic rationaleProgram componentsOutcomesRehab in non-COPD settings2075Workload (Watts)15011
2/18/2021Exercise PrescriptionLower extremityendurance training Treadmill (Walking)– Start 60-80% of the speed walked on the initial sixminute walk 10 or more minutes (intervals are appropriate)– Once patient is able to walk continuously for 20minutes, the speed is increased by 10%– Use Borg dyspnea scale (0-10) with target of 4-6 totitrate exercise– Once patient is able to walk 2.0 mph, then anincline is addedUpper extremity training in COPD Bicycle ergometry– Start Based on 60-80%% ofworkload extrapolated from 6minute walk speed– Once patient is able to do15 minutes then theresistance is increased in 510 Watt increments Upper extremity tasksdivert shoulder girdlemuscles that COPDpatient uses to assist inbreathing Upper extremity exercises– Unsupported weight lifting2-3 pounds– Therabands– Arm ergometry12
2/18/2021Upper extremityexercise prescription Upper Body Ergometer– Start - 6 minutes at constant– Increase Resistance based on Borg dyspnea scale Time – aiming for 15 minutes of continuoustraining'Dumb-bells foryour diaphragm' Used in patients withinspiratory muscle weakness(maximum inspiratorypressure 50% of predicted) Spring-loaded device withadjustable pressure Two 5 minute sets, adjustresistance weeklyInspiratory muscletraining in COPD Rationale – Inspiratorymuscle dysfunction– Geometric changes in the thoraxand diaphragm– Systemic factors– Possible structural changes inthe respiratory musclesBreathing retraining Pursed lip breathing– Increase pressure in themouth transmitted to smallairways– Prolonged expiratory phase– Minimize dynamichyperinflation13
2/18/2021Education topicsPsychosocial/Behavioral Component Prevalence of anxiety and depression very high inchronic lung disease Group sessions– Introduction/Stress– Physical symptoms– Cognitive issues– Emotional issues– CopingIntervention with pulmonary rehabtraining/ Upper extremitytrainingIncreased load anddecreased efficiencyof respiratory muscles*Psychosocial counseling/ educationAnxiety/DepressionDyspnea on exertion* Lower extremity “aerobic” trainingDeconditioning* Breathing retrainingIncreased lactateproduction during exerciseDecreased oxidative capacity ofskeletal muscle enzymesOrientationAnatomy and physiology of lungsBenefits of exerciseRespiratory musclesOxygen and oxygen therapyInfection controlMedication managementEnergy conservationDiet/NutritionImportance of continuing maintenance exercise* Respiratory muscleHyperinflation/airflow obstructionCOPD Outline Definition/BackgroundPhysiologic rationaleProgram componentsOutcomesRehab in non-COPD settings14
2/18/20212015 Cochrane Review: PulmonaryRehabilitation for COPD.(McCarthy et al.) Review of 65 randomized controlled studies Conclusions – Pulmonary Rehabilitation is animportant component of disease management:– Improves exercise tolerance, relieves dyspnea andfatigue and enhances sense of control– Effects are moderately large and clinicallysignificant– Additional randomized trials comparing pulmonaryrehab to usual care for COPD are not warrantedAssociation Between Initiation of PulmonaryRehabilitation After Hospitalization for COPD and1-Year Survival Among Medicare BeneficiariesLindinauer et al., JAMA 2020 Retrospective cohort study – 4446 hospitals Medicare beneficiaries hospitalized for COPD in 2014 Evaluated 1 year mortality in those receiving pulmonaryrehabilitation within 3 months of discharge compared tothose who did notCOPD and Pulmonary Rehab Consider in:– Any patient with dyspnea on exertion despitemedical management– Medicare covers patients with GOLD II disease(FEV1/FVC 0.70 and FEV1 80% ofpredicted)– Sessions at OSU are 3/week for 8 weeks.Each sessions lasts 2 hoursAssociation Between Initiation of Pulmonary RehabilitationAfter Hospitalization for COPD and 1-Year Survival AmongMedicare Beneficiaries Lindinauer et al., JAMA 2020 2721 (1.5%) patients had pulmonary rehab within 3months of discharge Mortality of those having rehab within 3 months – 7.3%vs 19.6% (p 0.001) Every 3 additional rehab sessions was significantlyassociated with a lower risk of death15
2/18/2021Outline Definition/BackgroundPhysiologic rationaleProgram componentsOutcomesRehab in non-COPD settingsPulmonary Rehabilitation for NonCOPD Patient Groups IPF Asthma PulmonaryHypertension Sarcoidosis Kyphoscoliosis Bronchiectasis Pre-post lungtransplant Pre-post lungvolume reductionsurgery Pre-post lungcancer resectionPulmonary rehab in interstitiallung disease Exercise Training in ILD– Improved 6 minute walkdistance– Improved respiratorysymptoms– Improved peripheralmuscle oxygen extraction64 y.o 2 days of N/VMild cough anddyspneaCOVID 2 days later – severehypoxemicrespiratory failurerequiring mechanicalventilation16
2/18/2021After 14 days,patient dischargedon supplemental O2Post-dischargeimaging showsevidence of postinflammatory fibrosis.PFT’s show severerestriction17
Cardiac Rehabilitation: Introduction CR is comprehensive long-term services involving: Medical evaluation Prescribed exercise Cardiac risk-factor modification Health education Counseling Behavioral interventions Wenger NK, et al. [NHLBI Clin Pract Guidel No. 17]. Clin Pract Guidel Quick Ref Guide Clin. 1995 Oct;(17):1-23.