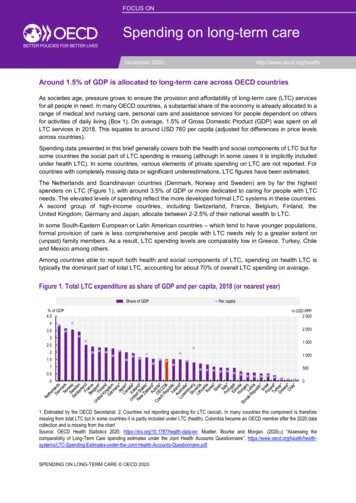
Transcription
Reducing Harm Improving Healthcare Protecting CanadiansMEDICATION RECONCILIATIONIN LONG-TERM CAREGetting Started KitMarch 2012www.saferhealthcarenow.ca
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012Safer Healthcare Now!We invite you to join Safer Healthcare Now! to help improve the safety of the Canadian healthcaresystem. Safer Healthcare Now! is a national program supporting Canadian healthcare organizations toimprove safety through the use of quality improvement methods and the integration of evidence inpractice.To learn more about this intervention, to find out how to join Safer Healthcare Now! and to gain accessto additional resources, contacts, and tools, visit our website at www.saferhealthcarenow.caThis Getting Started Kit has been written to help engage your interprofessional/interdisciplinary teams ina dynamic approach for improving quality and safety while providing a basis for getting started. TheGetting Started Kit represents the most current evidence, knowledge and practice, as of the date ofpublication and includes what has been learned since the first kits were released in 2005. We remainopen to working consultatively on updating the content, as more evidence emerges, as together we makehealthcare safer in Canada.Note:The Getting Started Kits for all interventions are available in both French and English.This document is in the public domain and may be used and reprinted without permission providedappropriate reference is made to Safer Healthcare Now!2
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012AcknowledgementThe Institute for Safe Medication Practices Canada (ISMP Canada) leads the medication reconciliationinitiative for the Safer Healthcare Now!This Medication Reconciliation in long-term care kit has been prepared by ISMP Canada and containsmaterials, documents and experiences of medication reconciliation teams across Canada customized tothe long-term care setting. The insight and contributions of the Canadian Medication ReconciliationFaculty are gratefully acknowledged.Canadian Medication Reconciliation Faculty(September 2011)ProvinceNameFacilityPositionONBell, ChaimUniversity of Toronto,St Michaels HospitalAssistant Professor of Medicineand Health Policy, Management,& Evaluation, Staff GeneralInternistONColquhoun, MargaretISMP CanadaISMP Canada Project Leader,Medication ReconciliationNational LeadNSCreighton, PaulaNova Scotia HealthGeriatric PhysicianONEtchells, Edward E.Sunnybrook HealthSciences CentreDirector, Patient Safety ServiceONFernandes, OlavoUniversity Health Network,ISMP CanadaPharmacy Practice LeaderONFlintoft, VirginiaSafer Healthcare Now!Central Measurement TeamMBHoncharik, NickWinnipeg Regional HealthAuthorityRegional Pharmacy Manager,Professional PracticeDevelopment, Clinical PharmacistABJames Fairbairn,KathyGood Samaritan SocietyConsultant PharmacistSKJohnson, JulieRegina Qu'Appelle HealthRegionDirector, Quality ImprovementONLam, JamesProvidence HealthcareDirector, Pharmacy ServicesLester, Mary LouBC Patient Safety & QualityCouncilSafer Healthcare Now!Norton, PeterUniversity of CalgaryMedical CentreBCABProject ManagerMedication Safety Leader - BCProfessor and Head of theDepartment of Family Medicine,Faculty of Medicine3
Reducing Harm Improving Healthcare Protecting CanadiansNameFacilityPositionSKParcher, MyraSaskatoon Home Care,Saskatoon Health RegionManager Operations - Home CareBCPataky, FruzsinaVCH-PHC RegionalPharmacy ServicesMedication Safety CoordinatorQURobitaille, CarolineHôpital Général JuifISMP CanadaPharmacistConsultantONStreitenberger, KimThe Hospital for SickChildrenQuality Analyst, Quality & RiskManagementProvinceThe Canadian Patient Safety Institute (CPSI) isacknowledged for their financial and in-kindsupport of the Safer Healthcare Now! GettingStarted Kits.The Institute for Safe Medication PracticesCanada (ISMP Canada) is an independentnational not-for-profit agency established forthe collection and analysis of medication errorreportsandthedevelopmentofrecommendations for the enhancement ofpatient safety.4
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012Table of ContentsSafer Healthcare Now! . 2Acknowledgement .3Canadian Medication Reconciliation Faculty . 3Table of Contents . 5Glossary of Terms . 7Introduction . 8What is meant by the term Long-Term Care in this kit? . 9Overview of Medication Reconciliation . 9The Case for Medication Reconciliation. 10The Impact of Medication Reconciliation . 11Medication reconciliation in the long-term care setting is a three-step process . 12What is the Best Possible Medication History (BPMH)? . 12Multiple Sources of Information Used to Obtain the BPMH . 12The Medication Reconciliation Process . 16Medication Reconciliation at Admission . 16Medication Reconciliation at Internal Transfer . 20Medication Reconciliation at Discharge or External Transfer . 21Implementing the Medication Reconciliation Process . 23Getting Started with Implementing Medication Reconciliation in Long-Term Care . 231. Secure Senior Leadership Commitment . 232. Form a Team . 233. Use the Model for Improvement to Accelerate Change . 244. Implement Changes . 295. Spread Changes . 30Measuring the Success of Medication Reconciliation . 31Core Measures . 31Collect Data . 32Optional Measures . 34Measurement Tips . 35Submitting Data to SHN . 36Data Submission . 37How long should you continue to measure? . 38Challenges of Medication Reconciliation in Long-Term Care . 39Summary . 42Appendix A - Glossary of Terms . 43Appendix B - Tips for Creating a Best Possible Medication History . 45Appendix C - Tips to Remember When Interviewing Residents . 47Appendix D - Resident and Family Role in the Medication Reconciliation Process . 48Appendix E - Resident Assessment Instrument . 50Appendix F - Sample Policies and Procedures . 515
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012Appendix G - Sample Tools for Admission Medication Reconciliation . 57Appendix H - Examples of Best Possible Medication Discharge Plan . 65Appendix I - Keys to Successful Implementation of Medication Reconciliation . 69Appendix J - Lessons Learned - the Canadian Experience . 70Appendix K - Examples of Change Concepts . 72Admission.73Transfer . 77General Processes . 78Appendix L - Individual Medication Reconciliation Audit Tool . 80Appendix M - Technical Descriptions and Worksheets . 821. Number of UNDOCUMENTED INTENTIONAL Discrepancies (DOCUMENTATION ACCURACY). 822. Number of UNINTENTIONAL discrepancies (Rate of Error) . 843. Percentage of residents reconciled on admission . 86Appendix N - Creating a Business Case for Medication Reconciliation . 88Appendix O- Communities of Practice . 90Appendix P - Suggested References . 92Additional Resources. 95Patient Safety Websites. 976
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012Glossary of TermsThe SHN Getting Started Kit: Medication Reconciliation in Long-Term Care uses the following terminology:(See Also Appendix A – Glossary of Terms).Undocumented Intentional discrepancy is one in which the prescriber has made an intentional choice toadd, change or discontinue a medication but this choice is not clearly documented.Unintentional discrepancy is one in which the prescriber unintentionally changed, added or omitted amedication the resident was taking prior to admission.Best Possible Medication History (BPMH): A Best Possible Medication History (BPMH) is a history createdusing 1) a systematic process of interviewing the resident/family; and 2) a review of at least one otherreliable source of information to obtain and verify all of a resident’s medication use (prescribed and nonprescribed). Complete documentation includes drug name, dosage, route and frequency. The BPMH ismore comprehensive than a routine primary medication history which is often a quick preliminarymedication history which may not include multiple sources of information.Best Possible Medication Discharge Plan (BPMDP) from acute care accounts for the medications that theresident was taking prior to admission (BPMH) to acute care, the most current medication list, and anynew medications planned to start upon discharge. The best possible medication discharge plan (BPMDP)should be communicated to the resident, community physician, community pharmacy and alternative carefacility or service.Most Current Medication List: The most recent list of medications (name of medication, dose, route andfrequency) currently taken by the resident. This list is communicated to the next care provider andprovides the starting point for the BPMH at the next facility or hospital. Examples of the most currentmedication list include: a comprehensive medication profile or a Medication Administration Record(MAR), which includes medications given weekly, monthly and every 3 months.Re-admission to long-term care refers to a resident externally transferred to an acute care hospital and isreturning (i.e. transferring back) to the same long-term care facility.7
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012IntroductionThis Safer Healthcare Now! (SHN) Getting Started Kit: Medication Reconciliation in Long-Term Care is astep-by-step guide to assist healthcare professionals working in long-term care facilities across Canadato implement medication reconciliation. Medication reconciliation is designed to reduce the number ofadverse drug events and potential resident harm associated with changes in medication information asresidents transfer from one care setting to another.Accreditation Canada has included reconciliation of the resident’s medications as one of the corepatient safety performance measures for long-term care organizations.1 The Required OrganizationalPractices related to medication reconciliation within the Patient Safety Area of Communication includerequirements to: Employ effective mechanisms for transfer of information at interface points, Reconcile the residents’ medications upon admission to the organization, and with theinvolvement of the resident, and The team reconciles the client’s medications with the involvement of the client, family orcaregiver at transition points where medication orders are changed or rewritten (i.e. internaltransfer, and/or discharge).This SHN Getting Started Kit is intended to assist long-term care facilities meet this patient safety goalby using quality improvement processes and will address the unique challenges of implementingmedication reconciliation in a long-term care facility.Although this kit is intended to be used by long-term care facility staff, its application may be extendedto rehabilitation hospitals, palliative care/hospice units, complex continuing care facilities, mentalhealth institutions and homes for children.8
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012What is meant by the term Long-Term Care in this kit?In general, long-term care facilities provide living accommodation for people who require on-sitedelivery of 24-hour, 7 days a week supervised care, including professional health services, high levels ofpersonal care and services. They accommodate varying health needs with on-site supervision forpersonal safety.2 Long-term care is governed by provincial and territorial legislation.Across the country, jurisdictions offer a different range of services and cost coverage. Consequently,there is little consistency across Canada in what facilities are called. (BC – Residential care facility, AB –Continuing Care Centre, SK – Special Care home, MB – Personal Care home, ON – Long-term Care Home,QC - Community Health Division) Centre hospitalier et d’hébergement de soins de longue durée(CHSLD), CHSLD privés, NB – Nursing Home, PEI - Government Manor home, Private Manor home, NS Nursing Home or Home for the Aged, NL - Nursing Home, YK - Residential Continuing Care Facility, NT Personal Care Facility, NU - Group Living Environment for Dependent Elderly.)3 For the purposes of thiskit, we will use ‘long-term care’.Long-term care, when compared with acute care, is characterized by higher resident to nurse orRPN/LPN ratios and on-site pharmacist/physician services that vary from daily to weekly or monthlybasis. The acuity of long-term care residents, while usually less than acute care patients has beenincreasing steadily, but long-term care residents are typically in more stable condition, except inspecialized programs. Therefore, changes to a resident’s care or medication regimen occur lessfrequently than in acute care. Residents in long-term care are often prescribed multiple medicationsand are usually serviced by a community or in-house pharmacy with multi-dose packaging.Overview of Medication ReconciliationWhat is Medication Reconciliation?Medication reconciliation is a formal process in which healthcare providers work together withresidents, families and care providers to ensure accurate and comprehensive medication information iscommunicated consistently across transitions of care.Medication reconciliation requires a systematic and comprehensive review of all the medications aresident is taking to ensure that medications being added, changed or discontinued are carefullyevaluated. It is a component of medication management and will inform and enable prescribers to makethe most appropriate prescribing decisions for the resident.Medication reconciliation is a process that can minimize potentialprescribing errors when a resident changes location.49
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012The Case for Medication ReconciliationLiterature about medication reconciliation in long-term care is building. Some studies show that asystematic approach to reconciling medications is reducing errors leading to adverse drug events andimproved efficiency in the medication system. Studies involving long-term care facilities indicate thatimprovements in access to accurate and timely information are needed. Recent articles refer to LTCspecific issues. These include: “Increased collaboration between nursing home registered nurses and licensed practical nurses staffcould improve patient care.” The March 2012 study stated that “Researchers estimate nearly800,000 preventable adverse drug events may occur in nursing homes each year. Many of theseincidents could be prevented with safety practices such as medication reconciliation, a process inwhich healthcare professionals, such as physicians, pharmacists and nurses, review medicationregimens to identify and resolve discrepancies when patients transfer between healthcare settings.In nursing homes, both registered nurses and licensed practical nurses often are responsible for thissafety practice. A recent study by a University of Missouri gerontological nursing expert found,when observed, these nurses often differed in how they identified discrepancies. Recognizing thedistinct differences between RNs and RPNs could lead to fewer medication errors and better patientcare.5 2006 survey by Lee – Studied the transfer of information from an acute care hospital to a long-termcare facility and found 22% of transfers had no formal summary of information. Legible summarieswere available only 56% of the time; secondary diagnoses were missing from 30% of transfers; only51% had allergies documented; clarification of information was difficult because identification ofhospital physician was only legible 41% of the time and phone numbers only 33% of the time. Theconclusions from this survey were that major errors of omissions and commissions occur frequentlywith potential for serious departures from intended or appropriate management resulting inunnecessary rework and inefficiencies.6 2007 survey by Earnshaw et al. - Surveyed 218 continuing care nurses and pharmacists from Albertaabout the quality of medication information received for new admissions transferred from acutecare hospitals. Only 25% reported medication information was “always” legible and complete withmedication name, dose, frequency and route. Only 10% of respondents reported that there was“always” enough information to tell if the prescribed medications were appropriate for theresident’s diagnoses. Sixty percent of respondents reported medication information arrived thesame day as the resident’s admission. Overall, their perspective of medication information receivedwas incomplete or inaccurate.7 2007 survey by Boockvar - Only 68% of responding long-term care administrators indicated that staffoften or always received all the information required to care for residents transferred from thehospital, 53% indicated they received a readable and easily understood post-hospital plan of care,and 38% indicated they received information about the purpose and diagnosis of each prescribedmedication. Fourteen percent (14%) also reported incidences of resident harm caused byinadequate communication of health information from hospital to a long-term care facility.810
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012 1997 study by Jones et al. of 709 long-term care residents transferred to the emergencydepartment, sixty-seven residents (10%) were transferred without any documentation. For thoseresidents with transfer documentation, 6 common discrepancies were identified. The authorsconcluded that many residents were transferred without appropriate documentation for theemergency physician.9 In a 2000 study by Gurwitz et al., adverse drug events occurred commonly among long-term careresidents and more than half (51%) were judged to be preventable. Serious life-threatening and fataladverse drug events were more likely to be preventable than less severe events. Most errorsassociated with preventable events occurred at the ordering and monitoring stages.10 In a 2007 Institute of Medicine Report, it was noted that components of the medication use systemoperate in silos with ineffective means of sharing important information across the continuum ofcare. The report recognized the need to improve continuity of resident care through theimplementation of medication reconciliation between hospital and community providers.11The Impact of Medication Reconciliation 2004 study by Boockvar - the incidence of adverse drug events caused by medication changes upontransfer between facilities was twenty percent (20%). Adverse events due to medication changesoccurred most often upon transfer from the hospital back to the nursing home. Incomplete orinaccurate communication between facilities was identified as a potential factor in theseoccurrences. Their recommendation was to implement an intervention, like medicationreconciliation, at the time of admission back to the long-term care facility.12 2006 study by Boockvar - The possibility of having a discrepancy-related adverse event was lesslikely in the group of residents who had medication reconciliation by a pharmacist (with physiciancommunication) upon transfer back from acute care to long-term care, compared with the groupthat did not. The pharmacist compared the medications ordered upon transfer back to the longterm care facility to the medications taken before hospitalization. The most common discrepancieswere omissions followed by additions and dosage changes. The most common adverse drug eventwas pain due to the omission of analgesics, and the most common causes of discrepancy-relatedADEs were antibiotics and analgesics.1311
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012Medication reconciliation in the long-term care setting is a three-step process:1. Create a complete and accurate Best Possible Medication History (BPMH) of the resident’smedications including name, dosage, route and frequency. This includes:o a systematic process of interviewing the resident/family, ando a review of at least one other reliable source of information;2. Reconcile Medications: Use the BPMH to create admission orders or compare the BPMH against theresident’s admission, transfer or discharge medication orders; identify and resolve all differences ordiscrepancies; and3. Document and Communicate any resulting changes in medication orders to the relevant providers ofcare and resident or family member wherever possible.Guiding PrincipleMedication reconciliation is a process that can minimize potential prescribing errorswhen a resident changes location.4What is the Best Possible Medication History (BPMH)?The BPMH forms the basis of medication reconciliation both in acute and long-term care. The BPMH isdocumentation of all medications, including drug name, dose, frequency and route that a resident iscurrently taking, even though it may be different from what was actually prescribed.At each interface in care when the resident is being transferred from one healthcare facility/service toanother, the BPMH should be compared to the resident’s medication orders. From our experience withmedication reconciliation in acute care, the BPMH is the cornerstone of the medication reconciliationprocess.Several tools created in the SHN in acute care are helpful in ensuring care providers obtain the BPMH inthe most efficient manner. These tools are available on the Medication Reconciliation Communities ofPractice website and can be accessed using the following links: Best Possible Medication History (BPMH) Interview Guide Medication History Taking Presentation – Winnipeg Regional Health AuthoritySee also Appendix B: Tips for Creating a BPMH and Appendix C: Tips to remember when InterviewingResidents and Appendix D: Resident and Family role in the Medication Reconciliation Process, AppendixG: Sample Tools for Admission Medication Reconciliation.Multiple Sources of Information Used to Obtain the BPMHThe sources of information used to obtain the BPMH differ with the specific types of admission to longterm care. (Refer to Table 1) Synthesizing the data from multiple sources of information will help ensurethe Best Possible Medication History (BPMH).12
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareMarch 2012Note: These are possible sources of information that may not always be available for use dependingon each individual transferring facility.Table 1: Sources of Information to Obtain the Best Possible Medication History (BPMH)Sources of InformationType of AdmissionFrom Acute CareHospital(New Admission)From Acute CareHospital(Readmission to LTC) Most Current Medication List (MAR or medication profile) Best Possible Medication Discharge Plan (BPMDP)* Transfer Orders/Discharge PrescriptionsPre-Acute Care Medications (if medication reconciliation was not clearlydocumented at the former facility) Review the “home medication list” Interview family/resident to confirm medications and dosages Review medication vials, blister pack medications Review community pharmacy profile or the provincial electronic healthrecord Review family physician records, home care records Most Current Medication List (MAR or medication profile)Best Possible Medication Discharge Plan (BPMDP)*Transfer orders, discharge prescriptionsPre-Acute Care Medications Resident’s most current long-term care MAR prior to hospital transferFrom Another LongTerm Care facility Most Current Medication List (MAR or medication profile)Resident Assessment Instrument (RAI)** – Section U - standard screeningand assessment tool used in long-term care (where completed)Pre-long-term care medications (if medication reconciliation was notclearly documented at the former facility) Review the “home medication list” Interview family/resident to confirm medications and dosages Review medication vials, blister pack medications Review community pharmacy profile, provincial electronic healthrecords or drug information systems (e.g. PIP, Drug Profile Viewer,PharmNet) Review family physician records, home care recordsFrom Community orAssisted Living Review the “home medication list” Interview family/resident, check medication vials, blister packmedication lists, home care health record Review community pharmacy profile, provincial electronic healthrecords or drug information systems (e.g. PIP, Drug Profile Viewer,PharmNet) Review family physician records, home care records13
Safer Healthcare Now! How-to Guide: Adverse Drug Events (Medication Reconciliation) in Long-Term CareSources of InformationType of AdmissionRehabilitation/Complex ContinuingCare facility(Rehab/CCC)March 2012 Most Current Medication List (MAR or medication profile)Discharge Prescription from the facility‘Dear Doctor/Community Pharmacy’ letterPre-Rehab/CCC medications (if medication reconciliation was not clearlydocumented at the former facility) Review the “home medication list” Interview family/resident to confirm medications and dosages Review medication vials, blister pack medications Review community pharmacy profile, provincial electronic healthrecords or drug information systems (e.g. PIP, Drug Profile Viewer,PharmNet) Review family physician records, home care recordsThe term Best Possible Medication Discharge Plan (BPMDP), introduced in the acute care SHN GettingStarted Kit is intended to be the product of medication reconciliation at acute care discharge. It shouldbe communicated to the long-term care facility upon admission but, may not be available as many acutecare organizations are focusing on admission prior to implementing discharge medication reconciliationprocesses. (See Appendix H for Examples of BPMDPs used in Acute Care)* Using the Best Pos
University of Toronto, St Michaels Hospital Assistant Professor of Medicine and Health Policy, Management, & Evaluation, Staff General Internist ON Colquhoun, Margaret ISMP Canada ISMP Canada Project Leader, Medication Reconciliation National Lead NS Creighton, Paula Nova Scotia Health Geriatric Physician ON Etchells, Edward E.