Transcription
Better Lives,Better EndingsA suite of resources forstaff in extra care housingMarch 2022The results of a project co-run by Octavia and St Christopher’s CARE and funded by Women in Fellowship
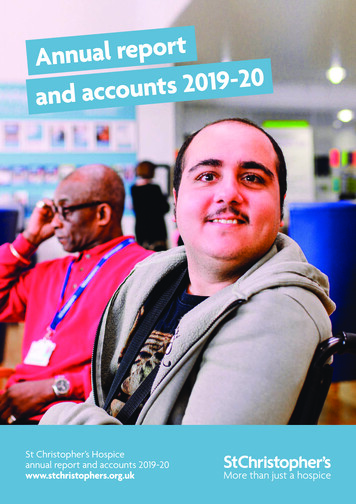
About the organisationsSt Christopher’s Hospice is a charity providing health and social care for peopleapproaching the end of their lives. The organisation was established by Dame CicelySaunders who is credited with establishing the modern hospice movement over50 years ago.Octavia is a not-for-profit organisation that provides homes, support and careto thousands of people in central and west London. Founded by the Victorianphilanthropist Octavia Hill in the 1860s, they support Londoners of all ages, givingthem opportunities that will help them lead a better life. Octavia operates sevenextra care housing schemes across west London.Authors: Antonia Bunnin, Abalone Consulting and Liz Bryan, St Christopher’s CARE.Better Lives, Better Endings project team: the project co-leads are Neil McCarthy,Assistant Director (Care, Support and Communities), Octavia and Liz Bryan, SeniorAssociate, St Christopher’s CARE. Antonia Bunnin is Project Facilitator, and LianneJoy, Head of Care Quality at Octavia is a key member of the team.The authors give particular thanks and appreciation to Neil and Lianne for all theyhave given to the project, and their hard work and continued commitment tomaking it a reality despite the demands of the pandemic. We are also grateful to allthe Octavia residents and staff who engaged in this work, and especially the extraOctaviaEmily House, 202-208 Kensal Road,London W10 5BNSt Christopher’s CARE51-59 Lawrie Park Road,Sydenham, London SE26 6DZT 020 8354 5500E info@octavia.org.ukwww.octaviasupport.org.ukT 020 8768 4656E org.uk/about-carecare staff who took part in co-designing and testing the online programme. Octaviamade a significant commitment of time and funding to this work.We would like to thank our funders, Women in Fellowship, whose financialsupport made this project possible. Our thanks too to the Housing Learning andImprovement Network (LIN) for their support with the launch of this publicationand our earlier case study about the Better Lives, Better Endings project.We thank the Better Lives, Better Endings advisory group, for their advice andencouragement over the course of the project: Karina Catley, London AmbulanceService NHS Trust; Lena Coupland, North West London CCGs; Linda Dhillon,Westminster City Council; Rachel Dickinson, Westminster City Council; Anne Lang,St John’s Hospice, London; Caroline Phillips, London Ambulance Service NHS Trust/St Christopher’s; Jeremy Porteus, Housing Learning and Improvement Network;Louise Whitley, Skills for Care.Our thanks also to all the guest speakers who helped us deliver and test thenine-week Better Lives, Better Endings programme in May, June and July 2021: AnneLang, St John’s Hospice, London; Karina Catley and Di Laverty, London AmbulanceService Macmillan team; Steph Turner, creative facilitator; Christine Lawlor,Portland Road GP surgery, London; and Aly Dickinson and Emma Clare, End of LifeDoula UK. St Christopher’s and Octavia March 2022. This publication is free to download, replicate and use. We ask thatyou acknowledge St Christopher’s and Octavia when you use the publication. Disclaimer: this publication containslinks to various materials and resources produced by others. We have credited those organisations in all cases.St Christopher’s and Octavia do not take responsibility for the content of external sources.Better Lives, Better Endings A suite of resources for staff in extra care housing 2
ContentsIntroduction4Theme 1: Recognising the need for cultural change8Theme 2: Understanding dying and what happens at theend of life11Theme 3: Relationship-based care in practice14Theme 4: Understanding what is important20Theme 5: Acknowledging grief and loss24Theme 6: Building relationships with external services27The nine-week Better Lives, Better Endings programmefor extra care staff31Guidelines and templates for using the Circles of Supporttool in extra care housing40Mapping our themes to the Care Certificate standards44Better Lives, Better Endings A suite of resources for staff in extra care housing 3
IntroductionBetter Lives, Better Endings A suite of resources for staff in extra care housing 4
IntroductionThis publication is part of Better Lives, Better Endings,a collaboration between St Christopher’s and Octavia.We initiated the Better Lives, Better Endings project toexplore how staff and residents in extra care housingmight be empowered to improve residents’ quality oflife and experiences at the end of life.Why we created this publicationThe purpose of this publication is to share resourcesthat help extra care staff think and talk about the natureof death, dying loss and grief for residents, as well asfactors that can improve their quality of life. We haveshared the story of our approach, and how we haveused some of these resources, in the hope that they willact as an inspiration (not a prescription!) to others.be particularly useful when used by a whole team ororganisation to learn, discuss and explore together,and consider what changes to introduce in their ownworkplace.The publication is also for hospices and other expertproviders of palliative and end of life care. We hopethey may use it to inform their own relationships withextra care and housing associations. It could be usedto support educational work, or it might stimulatehospices and housing providers to initiate new localcollaborations.What is extra care housing?Through our joint work, we recognised the need for acollation of resources that are meaningful to busy staffwho care deeply about improving residents’ quality oflife and experience of death, but who don’t have thetime or desire to study academic articles or lengthyreports. Our emphasis is on resources that are ‘bitesized’ and easy to use. We have included resources in avariety of formats: short films, case studies, tools andtemplates.‘Extra care’ means housing made up of self-containedhomes (usually flats) with design features and supportservices available to enable self-care and independentliving. Extra care comes in different forms, and issometimes described as: ‘housing with care’, ‘verysheltered housing’, ‘retirement villages’ or ‘retirementcommunities’. People living in extra care may betenants, owners or part-owners. Extra care housing isused by older people, people with learning disabilities,people with physical disabilities and people withdementia1.Who is it for?A co-designed approachOur publication is for anyone working in extra careor other supported housing settings where careis provided. Individuals can use it to deepen theirunderstanding of death, dying, grief and end of lifecare and ways of supporting residents throughouttheir time living in extra care housing. We think it willFrom the outset we took a co-designed approach tocreating the Better Lives, Better Endings programme.Extra care staff undertake significant amountsof mandatory training, often focused on factualknowledge that they are expected to memorisethen apply in specified circumstances. We tooka fundamentally different approach: one thatemphasises reflection, open discussion, practicebased learning and real-life application. We began byasking extra care staff about their experiences andconcerns, as well as talking to Octavia’s residents. Aswe were designing the staff development programme,we involved Octavia staff throughout in shapingthe programme to address their needs. Our aim wasnot to impart a set of facts, but for staff to gainconfidence, skills, knowledge and a greater sense ofagency in supporting residents to have better livesand better endings. We say more about our co-designapproach in Theme 1: Recognising the need forcultural change.How to use this publicationThe publication is organised into several themes. Foreach theme, we talk about: Why it is important What we did in the Better Lives, Better Endingsprogramme Putting change into practice – what Octavia is doing Useful resources.We also share insights from Octavia extra care staff– sometimes about issues and challenges they haveexperienced, and sometimes about the impact of theBetter Lives, Better Endings programme and resultingchanges in practice.There is no single way to use this publication. You canread it all the way through, or dip in theme by theme.1 The Housing LIN gives more information about extra care: gExtraCare/Better Lives, Better Endings A suite of resources for staff in extra care housing 5
We have shared the outline of our pilot nine-weekstaff development programme, not to be prescriptive,but in the hope that it may stimulate others interestedto design their own learning programmes with extracare staff. We suggest you view the resources usingthe hyperlinks; you may want to use these in your ownworkplace or seek out additional resources of yourown.Some of the ways that we envisage the publicationbeing used are: To stimulate thinking for people designing structuredlearning programmes with extra care staff, or otherstaff in care and support roles To support use of the Care Certificate2 duringinductions and with existing staff To offer groups of staff a starting point and ‘way in’for discussing and doing some work on a particulartheme or topic Through sharing ideas about what changes can bemade, to inspire action and change elsewhere For work-based discussion groups/learning groups, toconsider together For hospices and extra care providers to considercreating new collaborative relationships.About the Better Lives, BetterEndings projectOctavia and St Christopher’s began Better Lives, BetterEndings in autumn 2019, following other joint workbetween our organisations. Our project’s focus wason facilitating conversations, decisions and plans forhow people in extra care housing want to live in thelast years of life, then making sure people’s wishesare understood, documented and acted on. Doingthis effectively meant drawing on the voices andexperiences of people living in extra care housing,and of the staff who support them. A key elementwas to develop and test a programme for extra carestaff to build skills and confidence around difficultconversations, advance care planning and engagementwith the health system and others, to enable residentsto achieve their wishes.Our underpinning premise is that if individuals comingto the end of their lives have identified their ambitionsand goals for the last years of life and articulated themclearly, then people around them (staff, volunteers,family members, friends and the people they live with)can help them achieve these. They will have greaterchoice and feel greater control; all involved will feelempowered in their efforts to help individuals live well.Better Lives, Better Endings was originally intendedas a one-year project, with significant co-design byresidents as well as staff. Five months in, the arrival ofCovid-19 threw our plans into upheaval. We pausedthe project whilst Octavia staff focused on the hugeimmediate challenges of running services during thefirst wave. After exploring various possibilities, wereluctantly recognised that ongoing engagementwith residents was no longer realistic given Covid-19restrictions. We decided to use the findings from ourinitial work with residents, but focus the remainingproject on co-design with staff. In July 2020, Liz, theSt Christopher’s co-lead, ran three online hour-longevening sessions for staff at two of Octavia’s extra careschemes, including reflection, guidance and discussionbased on real people that staff had cared for. This wasa response to Covid-19 and not formally part of theproject, but was valuable in informing our subsequentnine-week programme.In May, June and July 2021, we tested the nine-weekBetter Lives, Better Endings programme with 26staff. From the outset we stressed that this was not atraditional training programme. Participants came fromall seven Octavia extra care schemes: managers, deputymanagers, team leaders, and care staff as well as thenewly-formed central quality team. The continuingpandemic meant we ran it online using zoom, in twohour sessions over eight consecutive weeks, with a ninthweek for reflections and feedback. In between sessions,participants were given short activities to complete.We held a further session six months later, in November2021, to discuss what difference the programme wasmaking for individual staff, at workplace level in differentextra care schemes and most importantly, for residents.Better Lives, Better Endings is situated as part ofOctavia’s wider agenda of transformation and culturechange. It is part of embedding a shift from task-basedto relationship-based care and support. It is not justabout end of life, but about exploring how staff canbetter support residents throughout their whole timeat Octavia. The aim is to ensure that care and supportfor each resident reflects an understanding of what isimportant to that person and their individual needs,preferences and wishes as they age, experience changeand prepare for their end of life. As our work evolves,it is ever clearer how this cultural change is essential tocreating the conditions for staff to feel confident totalk openly with residents about death, dying and lossand empowered to respond to those conversations inmeaningful ways.Our Housing LIN case study gives more informationabout the collaboration: are-housing-and-ahospice/2 T he Care Certificate was developed jointly by Skills for Care, Health Education England and Skills for Health. It sets out 15 standards that are expected of health and care staff in certain roles, and that should beaddressed in induction programmes. We have mapped our themes to the Care Certificate Standards in the section Mapping our themes to the Care Certificate standards.Better Lives, Better Endings A suite of resources for staff in extra care housing 6
Context and needThe UK has an ageing population. Increasing numbersof people are living with a long-term health condition,and often with several conditions at the same time(multimorbidity). This includes people living with frailty,and those in the last 12 months of life who may havenon-reversable conditions such as dementia, advancedheart disease or progressive neurodegenerative disease.Organisations that provide extra care housing – alongwith the rest of the health and care system – areresponding to the increasing complexity and higherlevels of need in the people they support. Whereasin the past extra care providers might have requiredsomeone to move out to a nursing home if their healthdeteriorated and their needs rose, now increasinglyextra care providers are offering a home for life. Formany residents of extra care, their home is the placewhere they would prefer to die.Extra care is adapting to society’s demographic changesby increasing the skills and capabilities of staff, toequip them to provide care and support for people astheir needs change, right up to the end of life and asthey die. As the Housing LIN3 says:“Dying is not just a physical reality, but a social eventtoo and it is important to address the emotional,social, cultural and spiritual needs of people andtheir families. Providing effective, high-quality carefor someone during the end of their life is a highlyskilled role and a challenging one. While it’s a teameffort and does not all fall upon the shoulders ofone individual, without support and information,staff and informal carers can find the experienceoverwhelming.”3 The Housing LIN gives more information about extra care: gExtraCare/Better Lives, Better Endings A suite of resources for staff in extra care housing 7
Theme 1:Recognising theneed for culturalchangeBetter Lives, Better Endings A suite of resources for staff in extra care housing 8
Theme 1: Recognising the need for cultural changeWhy it is importantThe Better Lives, Better Endings project grewfrom an existing relationship between Octaviaand St Christopher’s. It was soon apparent thatour organisations had similar values, but differingexperience and skills. Both also recognised the need toevaluate effectiveness and, if necessary, to change. Thisopenness to change on both parts played a key role inthe approach to creating Better Lives, Better Endings.Octavia was increasingly aware of the importance ofproviding supported housing for people right up to theend of their lives, and ensuring a good quality of life tothe end. However, in practice Octavia was finding bestefforts were being frustrated by blocks and obstacles,without really understanding the root causes. Frontlinestaff often felt powerless, with little confidence oragency when supporting people at the end of life.Staff wanted to act as advocates for residents, but feltignored or over-ridden by external health and careservices. St Christopher’s was increasingly aware of theneed to share its expertise with partner organisations,in ways that empower others and enable them tosignificantly improve the experience of people in theircare at the end of life.Better Lives, Better Endings offered both organisationsan opportunity to experiment. We knew we had a lotto learn from each other. We also recognised that togain lasting benefit from the project, both organisationsmust be open to adapting and working in new ways.St Christopher’s CARE: approachto learningSt Christopher’s approach to supporting learningis based on four principles: learning must becollaborative, current, challenging and contextspecific. It should also be underpinned by positiveongoing relationships. Learning that results in real andsustainable change is transformative: the ‘meaningperspectives’ of both individuals and teams have beenchanged or transformed so they are more likely to beable to change behaviours.To facilitate learning that would be transformative aspart of Better Lives, Better Endings we endeavouredto:1 establish a safe environment for staff to share theirperspectives2 provide engaging and varied ways of presenting thecontent so that staff could make their own sense ofwhat they were hearing and seeing3 encourage staff to discuss and critically evaluatethe material that was presented. We invited staffto relate the material and discussions to their ownexperiences, care settings and extra care schemes4 provide opportunities for reflection, includingspace to explore any changes to their originalperspectives5 challenge staff to identify actions that they couldtake to put their learning into practiceWhat we did in the Better Lives,Better Endings programmeWe began our project by speaking with staff andresidents. Two residents took part in sessions with aCreative Facilitator, using collage to share somethingof their lives, families and friendships, prioritiesand wishes for the future. Both residents found thesessions rewarding and we would have held more, hadCovid-19 not intervened. Some residents were keento talk about their hopes and wishes for the end oflife, and have these documented so they could beacted on. Many residents spoke about their currentquality of life, citing loneliness, isolation, boredom,and limited mobility. This reinforced the importanceof focusing on both ‘better lives’ and ‘better endings’.We spoke with 28 extra care staff in a range of roles.Some were eager for more open conversations withresidents about death, dying and future wishes.Others were reluctant, because it made them feeluncomfortable or they feared upsetting residentsand families. We heard about the long-standingrelationships with residents, often formed over years.When residents are seriously ill or dying, staff are oftenanxious and lack confidence in caring or advocating forthem. When residents die, staff grief can be strong andlasting, sometimes heightened by lack of systematicsupport. These conversations with staff provided thebasis for deciding together the key themes for thestaff development programme.In July 2020, our Project Co-Lead ran a mini-programmeof three one-hour sessions: Ensuring Dignified andCompassionate Care at the End of Life at Octavia.These were for staff at two extra care schemes wantingexpert support in light of experiences during thepandemic. These were interactive and discussionbased. Drawing on recent situations, we consideredwhat aspects had gone well, what might have beendone better, and what needs to change to supportmore person-centred care at the end of life. Thesediscussions and the ideas they generated informed thenine-week programme.Better Lives, Better Endings A suite of resources for staff in extra care housing 9
Drawing on everything we had learnt from the earlierstages, we worked with Octavia staff in designing thenine-week programme. We sought staff involvementin deciding what would be most valuable and what toinclude, at the first session and iteratively throughoutthe eight weeks and afterwards. We held a ninthsession for staff reflection and feedback at the endof the programme, and a further follow-up sessionsix months later. We invited staff to feel free to sharecomments by email, phone or text. We spoke openlythroughout about testing the programme and wantingto learn from participants about whether it wasmeeting their needs and how it could be improved.Putting change into practice:what Octavia is doingWider organisational change Octavia realised that tohave lasting effect, Better Lives, Better Endings must bepart of a wider shift across the organisation, away fromtask-based care, and towards relationship-based care.In early 2021, Octavia established a Quality Team ofthree people, working across all the extra care schemesto support and embed these changes in culture andways of working.Staff ideas for change Near the end of the nine-weekprogramme, staff identified ideas for change to try outindividually and in teams. In keeping with the ethosof co-design, it was important that these ideas camefrom staff themselves, and that they be supportedand encouraged – not told – to try putting them intopractice. Each extra care scheme came up with at leastone idea for change. Ideas varied across schemes, andincluded: creating a memorial garden; introducingmusic sessions with residents; setting up a residents’knitting group; introducing a Namaste programme forresidents with dementia; strengthening relationshipswith GPs, local hospices and other parts of the healthand care system; and creating a ‘traffic light system’ toincorporate into assessments and Care and SupportPlans to more systematically identify residents withincreasing levels of need.Turning staff ideas into action Now the OctaviaQuality Team is supporting teams in each scheme toput the changes into practice. Some are more complexthan others, and some will take longer than others.Some ideas will be initiated by one scheme with theintention of piloting and rolling out if successful, acrossall schemes. But there is a desire and commitmentto build on the enthusiasm of staff and to createmeaningful change that will improve the lives ofresidents. The next themes contain more informationabout some of these changes.“We had a good time, discussion, conversation,we were free to talk about what we feel, whatconcerns us, I think we were a good team together.And you [the facilitators] were good, we reallyappreciated it and enjoyed it. The difference is itwas on zoom, not face to face, I think for myself Iprefer face to face, you can discuss more, you candemonstrate things. But because of the situationwe did appreciate that.”Reflections on the Better Lives, Better Endingsprogramme, six months laterUseful resourcesWebsite The Point of Care FoundationThe Point of Care Foundation has information aboutthe principles and practice of co-design in health andcare: https://www.pointofcarefoundation.org.uk/Website and video (four minutes)St Christopher’s CARESt Christopher’s CARE webpage includes a videodescribing St Christopher’s vision for uk/about-care/Better Lives, Better Endings A suite of resources for staff in extra care housing 10
Theme 2:Understanding dyingand what happensat the end of lifeBetter Lives, Better Endings A suite of resources for staff in extra care housing 11
Theme 2: Understanding dying and what happens at the end of lifeWhy it is importantStaff wanted to learn about what happens at the endof life and when someone is dying. Many did not feelconfident to identify that someone might be nearthe end of life, or understand what dying looks likeand what to expect. Some were fearful of being withor providing care for dying residents. Even those whohad cared for people as they were dying wanted tounderstand more, and contextualise their experiences.Staff recognised that demystifying death wouldhelp them feel able to talk more openly about thesethings with residents. It will also help them be moreconfident and knowledgeable when communicatingwith GPs, hospices and the ambulance service aboutsick residents.What we did in the Better Lives,Better Endings programmeOur work with staff included reflecting togetheron the experience of death and dying from botha personal and a caregiver perspective. We invitedstaff to consider recent cases of residents who haddied, as well as fictional case studies and scenarios.We discussed in small groups what staff would needin order to provide the best possible experience forresidents as they approach the end of life. One was:an understanding of how to identify someone mightbe coming to the end of life, and what dying lookslike. We talked about changes, signs and symptomsthat might indicate that someone is coming to theend of their life, and what they mean. Staff reportedoften feeling ‘helpless’ when a resident is dying due tolack of knowledge and their perception that externalmedical professionals have control in these situations.As part of the nine-week programme we shared thefilm by Dr Kathryn Mannix, In my humble opinion –dying is not as bad as you think. Guest speakers fromthe local hospice and from End of Life Doula UK talkedto participants and answered questions. All of thishelped to create reassurance and understanding thatdeath can be gentle and peaceful, and that staff cangain confidence as they learn what to expect and howto best support dying residents.Putting change into practice:what Octavia is doingConfidence to talk about death and dying Staff whohave been through the nine-week programme told usthey feel more confident to talk about death and dyingwith residents, and to care for people who are dying.End of life awareness as part of induction Octavianow believes that all extra care staff should have abasic level of understanding about dying, death, griefand end of life care. Octavia is developing contentbased on the themes of this publication which willbecome part of induction mapped to the standards ofthe Care Certificate for all extra care staff, to providethis foundation-level awareness.“When we started [working in extra care], we werenot aware of how advanced it would get, that wewill be required to deal with end of life. We neverhad the education, the training, any workshops todeal with end of life. It was more about maintainingindependence, they would set targets. All theseyears you don’t come across a conversation aboutend of life. Now it is changed. There is more end oflife now. Then, seven, eight years ago, it was thatonce someone deteriorated, then they would moveto a care home. Their care package would change andthey would move to a nursing home. Through theyears that has changed, now it is their home to theend of their life.”“We used to have a tenant, and I used it [what Ilearnt on Better Lives, Better Endings] for thatspecial time, at the end of his life. I was workingat night and he was a very private person, but thatnight when I went to check on him, he wasn’t likehimself. I looked after him really well. He always said:‘how are you?’ ‘nice to see a smiling face’ and thisand that. That night he wasn’t himself, all his clotheswere on the floor, he was getting moody. I gave himwater to drink, he said thank you. I didn’t see himafter that night, he had a fall and went to hospitaland we didn’t see him. He died after that night. Afterabout three days. We knew he was going to die You think about the tenants, whether their life isending, to give them good service, better service,you give the best care you can.”Useful resourcesVideo (four minutes) In my humble opinion – dying isnot as bad as you think. BBC Ideas film (2019)Palliative care doctor and author Dr Kathryn Mannixexplains that in our society, death is no longer partof daily life. Many people do not know what thenormal dying process looks like. We have becomedetached from death and scared to talk aboutit. She describes the gentle process of a normaldeath in clear, straightforward language and givesreassurance that death is probably not as bad as wehave imagined.https://www.youtube.com/watch?v CruBRZh8qucBetter Lives, Better Endings A suite of resources for staff in extra care housing 12
Video (11 minutes) Holding Space. mote of dustfilms (2018)This short documentary is made by Rebecca Kenyon,an end of life doula and film-maker. It shows threepeople preparing for death, and the support theyreceive through their intimate and tender relationshipswith end of life doulas.https://www.youtube.com/watch?v l7nvTzDEwDQBetter Lives, Better Endings A suite of resources for staff in extra care housing 13
Theme 3:Relationship-basedcare in practiceBetter Lives, Better Endings A suite of resources for staff in extra care housing 14
Theme 3: Relationship-based care in practiceWhy
Better Lives, Better Endings A suite of resources for staff in extra care housing 2 Octavia St Christopher's CARE Emily House, 202-208 Kensal Road, 51-59 Lawrie Park Road, London W10 5BN Sydenham, London SE26 6DZ