Transcription
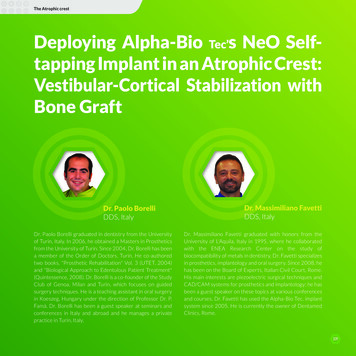
The Atrophic crestDeploying Alpha-Bio Tec’s NeO Selftapping Implant in an Atrophic Crest:Vestibular-Cortical Stabilization withBone GraftDr. Paolo BorelliDDS, ItalyDr. Paolo Borelli graduated in dentistry from the Universityof Turin, Italy. In 2006, he obtained a Masters in Prostheticsfrom the University of Turin. Since 2004, Dr. Borelli has beena member of the Order of Doctors, Turin. He co-authoredtwo books, "Prosthetic Rehabilitation" Vol. 3 (UTET, 2004)and "Biological Approach to Edentulous Patient Treatment"(Quintessence, 2008). Dr. Borelli is a co-founder of the StudyClub of Genoa, Milan and Turin, which focuses on guidedsurgery techniques. He is a teaching assistant in oral surgeryin Koeszeg, Hungary under the direction of Professor Dr. P.Famà. Dr. Borelli has been a guest speaker at seminars andconferences in Italy and abroad and he manages a privatepractice in Turin, Italy.Dr. Massimiliano FavettiDDS, ItalyDr. Massimiliano Favetti graduated with honors from theUniversity of L'Aquila, Italy in 1995, where he collaboratedwith the ENEA Research Center on the study ofbiocompatibility of metals in dentistry. Dr. Favetti specializesin prosthetics, implantology and oral surgery. Since 2008, hehas been on the Board of Experts, Italian Civil Court, Rome.His main interests are piezoelectric surgical techniques andCAD/CAM systems for prosthetics and implantology; he hasbeen a guest speaker on these topics at various conferencesand courses. Dr. Favetti has used the Alpha-Bio Tec. implantsystem since 2005. He is currently the owner of DentamedClinics, Rome.109
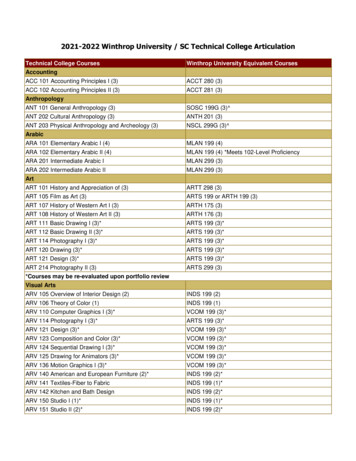
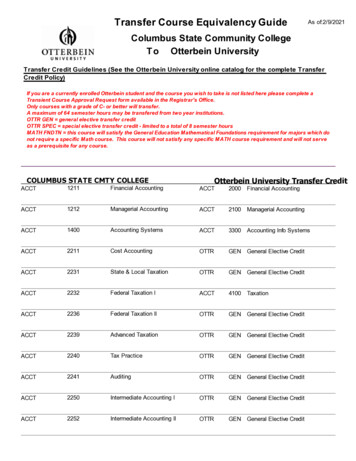
Deploying Alpha-Bio Tec’s NeO Self-tapping Implantin an Atrophic Crest: Vestibular-Cortical Stabilizationwith Bone GraftAbstractCase OverviewIn daily clinical practice, it is often necessary to re-treat patientswho have previously undergone prosthetic rehabilitations.It is not uncommon, in fact, to have to prosthetically re-treatpatients who have a prosthetic abutment (due to decay,root fracture etc), and a rehabilitation with implant supportoften becomes necessary. In cases in which extractionstook place several years earlier, we may find ourselvesfaced with atrophic crests, into which the insertion of animplant can be difficult and often requires an increase inbone volume. An example is presented below in which, byusing self-tapping implants, the vestibular-cortical boneloss is minimized, increasing the odds of implant success.Patient, female, 45-years old, non-smoker, without any particularproblems in his medical history, presented complainingabout a problem in the mandibular left quadrant. Thephysical examination reveals bridge decementation fromelements 35, 36 and 37. Simply redoing this bridge isimpossible, due to the absence of an adequate ferrule aswell as uncertainty regarding the long-term prognosis fortooth 37. It was decided, therefore, to replace tooth 36with an implant and GBR with a resorbable membrane andheterologous graft.IntroductionThe patient is normotrophic as regards to soft tissues andthe perioral musculature without significant asymmetriesof the face.The insertion of implants in atrophic bone crests can easilycreate fenestrations in the coronal part of the implant site.For this reason, many authors advocate using GBR (guidedbone regeneration) to prevent possible dehiscence in thepost-surgical phase and to guarantee the survival ofimplants, which is attributed to adequate bone thicknessesin the cortico-vestibular portion of the crest. [1-2] Vestibularbone loss is frequently caused by the technique used toprepare the implant site, that, for insertion of an implant ofØ3.75 mm diameter, usually anticipates an osteotomy witha drill of at least Ø3.2 mm diameter [3] . In such cases, the useof self-tapping implants and auto-condensers enables us toreduce the osteotomy to a Ø2.8 mm diameter drill, makingit possible to save at least 0.4 mm of vestibular corticalbone, fundamental in obtaining an optimal aesthetic andfunctional result that is long-lasting [4] .110Extraoral ExaminationIntraoral ExaminationGood level of oral hygiene, some signs and facets of dentalwear, absence of mobility problems (Fig. 1).1Frontal view of the patient
The Atrophic crestMaterials UsedX-ray ExaminationThe preoperative oral X-ray (Fig. 2) suggests that tooth 37has an uncertain long-term prognosis as bridge abutment.NeO implant Ø3.75 x 11.5 mm (Alpha-Bio Tec., Israel) inzone 36Resorable collagen membrance2Ortho-panoramic X-rayXenograftPTFE 4-0 suture (Omnia, Italy)Treatment Objectives and Work PlanThe CBCT (Figs. 3a and 3b) shows the crestal bone to bevery thin, but of adequate height for the insertion of animplant of 13 mm in length.3aCBCT with implant planningThe treatment plan includes a pre-implant hygiene session.Proper positioning of the implant will require an increasein volume from the vestibular side for the restoration ofcorrect tissue harmony and a correct emergence profile ofthe prosthetic crown. Several post-surgical follow-up visitsare planned at 2, 4, 7 and 14 days to disinfect the incisionwith chlorhexidine and to check for possible dehiscenceof the flap. The prosthetic phase will be carried outapproximately 4 months after the positioning of the implantand consists of a zirconia and ceramic crown on a titaniumabutment.Surgical PhaseAfter plexus anesthesia, performed with mepivacaine1:100.000 both in the vestibular and lingual fornix, a crestalincision was made without releasing cuts, so as not toreduce the vascularization of the flap, As predicted by theCBCT (Figs. 3a, 3b, 4),3bCBCT with implant planning4Flap incision111
the bone crest appears very thin, but of adequate height forthe insertion of an implant of 13 mm (Fig. 5).58Subcrestal insertion ofimplantOcclusal view of the gapIn order to minimize possible vestibular fenestration in thesub-crestal positioning of the implant of Ø3.75 x 11.5 mm,we decided upon a 13 mm preparation of the site, beginningthe drilling sequence with a 2 mm stop drill. The osteotomywas stopped at the 2.8 mm diameter drill (Fig. 6).9Subcrestal insertion ofimplant6Preparation of implanttunnelThe implant was inserted using a manual ratchet andstabilized in a subcrestal position with approximately 50Ncm of torque (Figs. 7, 8, 9).7Manual insertion of theimplant112Although no vestibular fenestration was observed at thetime of surgery, it was decided to increase the vestibularcortical bone thickness, since some portion of this boneis usually resorbed after implant placement. First, theresorbable membrane was stabilized lingually and, afterfilling the relevant zone with heterologous bone, themembrane was folded down on the vestibular side toprotect the graft (Figs. 10, 11).10Regeneration withresorbable membrane andheterologous bone
The Atrophic crest1114Regeneration withresorbable membrane andheterologous boneSutureThe surface of the membrane was then disinfected witha 0.2% chlorhexidine solution, and the flap was closedpassively in order to obtain a first degree closure withouttraction on the suture (Figs. 12, 13).The patient was discharged with the following drugregimen: rinses with 0.12% chlorhexidine diclugonate for60 seconds twice a day, antibiotic therapy with amoxicillinand clavulanic acid - 1 tablet of 875 mg twice a day, ice onthe first day and a semiliquid diet for the first week. At 15days after surgery, follow-up was performed to verify thehealing of the tissues (Fig. 15).12Release of the flap andprimary intention closure15Suture follow-up at 15days13Release of the flap andprimary intention closureAfter removal of the suture the site does not show signs ofdehiscence of the wound (Fig. 16).16Suture removal at 15 daysTwo lines of sutures are executed, the first with horizontalexternal mattresses, later stabilized with a second line ofseparate points more coronal to the first (Fig. 14).113
The successful osseointegration of the implant is visible onthe 4 month follow-up X–ray and all tissues appear to bewell healed (Fig. 17,18)References1.Christoph H. F. Hämmerle, Ronald E. Jung, AndreasFeloutzis. A systematic review of the survival of implantsin bone sites augmented with barrier membranes (guidedbone regeneration) in partially edentulous patients. J ClinPeriodontol. 2002; 29 Suppl. 3:226-31.2.Proussaefs, P., Lozada, J. The use of resorbable collagenmembrane in conjunction with autogenous bone graft andinorganic bovine mineral for buccal/labial alveolar ridgeaugmentation: a pilot study. J Prosthet Dent. 2003 Dec;90(6):530-8.3.Giro, G., Tovar, N., Marin, C. et al. The effect of simplifyingdental implant drilling sequence on osseointegration:an experimental study in dogs. Int J Biomater. 2013;2013:230310.4.Steier, L., Steier, G. Successful dental implant placementsurgeries with buccal bone fenestrations. J Oral Implantol.2015 Feb; 41(1):112-8.17Rx after 4 months18Tissue healing after 4monthsA healing abutment was then inserted (Fig. 19).19Healing abutmentThe case will be finalized and updated in the next fewmonths with the delivery of the final prosthetics to thepatient.114
CBCT with implant planning 3b CBCT with implant planning 4 Flap incision The CBCT (Figs. 3a and 3b) shows the crestal bone to be very thin, but of adequate height for the insertion of an implant of 13 mm in length. Materials Used Tec., Israel) in zone 36 Resorable collagen membrance Xenograft PTFE 4-0 suture (Omnia, Italy) Treatment Objectives .