Transcription
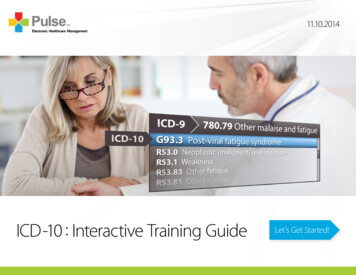
11.10.2014ICD-10 : Interactive Training GuideLet’s Get Started!
MENUBACK NEXTOur Objective.2DBACK g this document3.4.1. Menu - The menu allows the user to jump toany section of the book.2. Back / Next - These buttons allow for page-topage navigation.3. Medical Specialty Selection - This takes youto the medical specialty selection screen.4. ICD-10 Conversion Charts - Opens a browserwindow with ICD-10 reference materialproviding a comparison of ICD-9 codes to theirICD-10 counterparts.
MENUBACK NEXTICD-10: Interactive GuideMenuIntroduction3ImplementationGuideClinical DocumentationCoding ogyAuthorizationsDiagnostic RadiologyEndocrinologyENTCodingSpecific InformationFamily PracticeGastroenterologyGeneral SurgeryBillingNumber of CodesGynecologyHematologyInternal MedicineAppealsLength of CodesMental HealthNephrologyNeurologyContract NegotiationsCombination Use of AlphabetPediatricsPulmonaryRadiologyClinical DocumentationModern TechnologySubstance AbuseUrologyAre you Ready?
MENUBACK NEXTIntroduction4
MENUBACK NEXTIntroductionThe History of InternationalClassification of Diseases5The World Health Organization (WHO) firstThis translates into codified data detailing theestablished diagnosis coding with the 6thdiseases and other health problems recorded onedition of a published classification of index ofmany types of health and vital records includingdiseases, reformatted to become the Internationaldeath certificates and health records. In additionClassification of Diseases (ICD). WHO defines theto enabling the storage and retrieval of diagnosticclassification as “The standard diagnostic tool forinformation for clinical, epidemiological, andepidemiology, health management and clinicalquality purposes, these records provide the basispurposes. This includes the analysis of the generalfor the compilation of national mortality andhealth situation of population groups. It is used tomorbidity statistics by WHO member states. Itmonitor the incidence and prevalence of diseasesis also used for reimbursement and resourceand other health problems.” (1)allocation decision-making by countries.
MENUBACK NEXTIntroductionICD-9: TodayThe current method of diagnosis coding in the U.S. is ICD, 9th Edition, Clinical Modification (ICD-9). Ithas become obsolete, contains outdated terminology and does not allow for updates in healthcare,medicine and technology that have occurred in the 21st century. Due to these limitations, it has beenmandated that all healthcare providers in the United States comply with the International Classificationof Diseases, 10th Edition, Clinical Modification / Procedure Coding System (ICD-10). ICD-10 will fullyreplace ICD-9.On March 31, 2014, the US Senate voted to approve H.R. 4302, Protecting Access to Medicare Act of2014. This included language delaying the implementation of ICD-10 to October 1, 2015.ICD-10: FutureICD-10 is not a simple update to ICD-9. The structural changes throughout the coding system aresubstantial, and the increased level of complexity requires not only training for your coders but alsorequires significant involvement from the physicians, billing staff, and any areas in your practice thatcurrently utilize ICD-9. The objective of this ebook is to serve as a resource tool to understand, train,and successfully implement ICD-10.6
MENUBACK NEXTCoding Set Differences7
MENUBACK NEXTCoding Set DifferencesThe SpecificsICD-9 has long lacked necessary specifics, suchas similar injuries on opposite limbs having thesame ICD-9 code. This reduces documentationeffectiveness and has caused confusion on manydifferent levels. ICD-10 offers a greater degreeof specific information in areas such as rightversus left, initial or subsequent encounter,and other relevant clinical information. Thisgreater degree of specificity is utilized with anumber of different methods, many of whichare covered in this ebook.8
MENUBACK NEXTCoding Set DifferencesNumber of CodesAs part of the effort to provide more information,ICD-10 currently has roughly 68,000 availablecodes, with flexibility for adding new ones, incomparison to ICD-9’s 14,000 codes and limitedspace for additions. ICD-10 codes are different thanbefore, so education is crucial in understandingnew coding rules, guidelines, and documentationrequirements, as well as understanding theindexing for the many new codes.9
MENUBACK NEXTCoding Set DifferencesLength of CodesThe expanded number of characters of the ICD-10The following example shows the more detailedIn this example, S52 is the category. The fourth anddiagnosis codes provides greater specificity to identifyinformation gained through the added characters.fifth characters of “5” and “2” provide additionaldisease etiology, anatomic site, and severity.clinical detail and anatomic site. The sixth characterin this example indicates laterality, i.e., right radius.ICD-10 Code Structure:S52.5 Fracture of lower end of radiusThe seventh character, “A”, is an extension that: Characters 1-3 – CategoryS52.52 Torus fracture of lower end of radiusprovides additional information, which means: Characters 4-6 – Etiology, anatomic site, severity,S52.521 Torus fracture of lower end of right radiusor other clinical detail: Character 7 – Extension10S52 Fracture of forearmS52.521A Torus fracture of lower end of rightradius, initial encounter for closed fracture“initial encounter”.
MENUBACK NEXTCoding Set DifferencesCombination CodesICD-10 provides further use of combination codesthat can be used to classify such things as multiplediagnoses or a diagnosis with a complication.These are expressed as single codes, reducing thenumber of codes that need to be made while stillproviding information that is as specific as possible.Example: ICD-10 requires only one code, E08.42“Diabetes mellitus due to underlying conditionwith diabetic polyneuropathy”, while ICD-9 wouldrequire a minimum of two codes, 357.2 and a codefrom the code range 249.6-250.6.Use of AlphabetICD-10E11.22 - Type 2 diabetes mellitus with diabetic chronic kidney diseaseICD-10I50.21 - Acute systolic (congestive) heart failureICD-10I13.1 - Hypertensive heart and chronic kidney disease without heart failureICD-9 only utilized numeric codes. In contrast,ICD-10 utilizes alpha-numeric codes as part of itseffort for more specificity. The characters will notbe case sensitive, and both alphabetic and numericcodes are intended to retain identical meaningsas much as possible throughout code sets andprocedure sections.11
MENUBACK NEXTCoding Set DifferencesModern TechnologyICD-9 is currently considered to be based onoutdated technology, with codes unable to reflectthe use of new equipment and technology.ICD-10 offers far more integration with moderntechnology, with an emphasis on devices that arecurrently being used for various procedures. Theadditional reserved coding spaces available arepartly designed to allow for new technologyto be seamlessly integrated into codes, whichmeans fewer concerns about the ability toaccurately report information as medicaltechnology progresses.12
MENUBACK NEXTClinical Documentation13
MENUBACK NEXTClinical DocumentationImprovement areas to considerDocumentation will be significantly impactedby ICD-10 implementation. The changes in theTake a sampling of current records anddocumentation requirements to allow for theanalyze the documentation as to whether itgranular level of coding required by the newmeets the requirements for the ICD-10 code.code set must be properly documented in orderIf the documentation states only “fracture offor the coder to assign the correct code set tothe right patella” it would be missing five otherthe record. Repeated inquiries to the physiciandocumentation requirements required for ato clarify documentation will slow down theproper code assignment.revenue cycle. Educating the clinicians on thenew documentation requirements is essentialto a successful ICD-10 implementation. Considerthese suggestions to evaluate and monitor yourdocumentation improvement initiative:14: Assess documentation for ICD-10 readiness.: Implement early clinician education. If theclinician begins documenting the record withthe new requirements now, impact willbe greatly reduced.Post Implementation AssessmentEstablish a concurrent documentation reviewprogram. Closely monitor claims being denieddue to incomplete documentation andimplement a process for an audit and feedbackto the providers.
MENUBACK NEXTClinical DocumentationAre you ready?Accuracy of diagnosisThe best way to prepare for ICD-10 is to startGood clinical documentation starts with aIn ICD-9, the fifth digit of diabetes codes notutilizing workflows now that will need to happengood grasp of understanding documentationonly indicate the type of diabetes but alsowith ICD-10. There is not a grace period oncerequirements and the associated rationale.whether the diabetes is uncontrolled or out ofICD-10 is put into effect. Take advantage of thisWhile some unspecified codes are stillcontrol. In ICD-10, the physician must documenttime and start transitioning, so that on Octoberacceptable to payers, the increased specificitythat the diabetes is inadequately controlled,1, 2015 your processes are established andin ICD-10 codes means that simply saying aout of control, or poorly controlled. You haveunderstood.patient has uncontrolled diabetes is no longerto code the diabetes by type and add ‘withsufficient. ICD-10 codes will ask for the type,hyperglycemia’.If you would like assistance in performingan assessment of your current practiceand establishing ICD-10 processes, contactPulse RCM. Our RCM Managers and certifiedprofessional coders are ICD-10 certified, withthe knowledge and expertise to help ensure asuccessful transition for your practice.15complication, and manifestation, requiringproviders to understand and document thedifference between diabetes mellitus due toan underlying condition and diabetes inducedby drugs or chemicals.This is a documentation challenge just asmuch as a coding challenge. After all, if it isn’twritten down, then it might as well never havehappened. A coder can’t code what doesn’t exist.
MENUBACK NEXTClinical DocumentationCompleteness of documentationQueries and clarificationsPhysicians must be as specific as possible whenICD-10 will require coordination andUnderstanding the new documentationcharting notes. Since ICD-10 takes into accountcommunication.requirements and documenting them timely willmore variables than ICD-9 documentation, itis better for physicians to provide more ratherthan less.A busy physician with twenty or thirty patientsper day may not remember every detail of hisencounter with each patient. As a result theThis information is likely already being sharedprovider is at risk of supplying inaccurate orby the patient during your visit—it’s just aincomplete information in the event that theymatter of recording it for your coding staff.need to supplement their documentation afterGood documentation will also help reducethe fact. If physicians don’t understand whatthe need to follow-up on submitted claims—they need to provide to the coders, the coderssaving you time and money.will have no choice but to come back to themfor specificity.16reduce the amount of “after the fact” queries, whichcould possibly result in timely filing issues andimpact the revenue cycle.Continue to see ClinicalDocumentation Requirements& Examples by Medical Specialty
MENUBACK NEXTClinical DocumentationView by Medical SpecialtyPlease select a medical specialty below to jump to that yContactPulse ary
-9-10DDICICAnesthesiologyClinical Documentation18MENUBACK NEXT
-9-10DDICICClinical DocumentationAnesthesiology RequirementsThe following items should be documented as appropriate to allow complete coding under ICD-10Laterality : Left, right, bilateral, multiple locationsStatus of : AcuteDisease : Chronic: Intermittent: RecurrentGeneral : Detailed locations (Head, Shaft, Proximal, Distal, etc.)Injuries: Type of tendon (Flexor or Extensor): Episode of care (Initial, Subsequent, Sequela)Cause of : Mechanism – How it happened (struck by basketball)Injuries : Place of occurrence – Where it happened (high school): Activity – What patient was doing (playing basketball): External cause status – Military, Civilian, Work-related, Leisure19MENUBACK NEXT
-9-10DICDICMENUBACK NEXTClinical DocumentationAnesthesiology Clinical ScenarioPreop Diagnosisview and the lumbar spine was examined. TheRadiofrequency lesion was then created at 80Intractable back pain which is due to diskogenicsuperior medial aspect of the transverse processesdegrees for 90 seconds at each of the above levelspain, L4-L5, L5-S1 as well as facet arthrosis andof bilateral L4 and L5 at the junction of superiorbilaterally. At the end of lesioning, an injectionlumbar spondylosis, status post injury.articular processes were denoted on the skin. Thethat contained 40 mg of Depo-Medrol andbilateral sciatic notch as well as the superior medial0.5% bupivacaine was instilled, 1 mL into eachPostop Diagnosisaspect of the posterior foramen of S1 was equallylevel, to prevent post radiofrequency neuritis.Intractable back pain which is due to diskogenicdelineated. These areas were infiltrated with 1%The radiofrequency probe was removed andpain, L4-L5, L5-S1 as well as facet arthrosis andlidocaine using 1-1/2-inch 27-gauge needle. Next,the cannula was dilated and removed. Pressurelumbar spondylosis, status post injury.the radiofrequency pulse generator was primeddressing was applied over all the injection sites.ready and the safe test was completed. A Smith &The patient was taken to the recovery area inNephew device was utilized.stable condition.Procedure PerformedBilateral L3-L4 medial branches, L5 distal primaryramus, and S1 accessory branch radiofrequencyneurotomy.Findings and ProcedureFollowing informed consent, the patient was takento the operating room and placed prone on thefluoroscopy stretcher. The entire back was preppedand draped in sterile surgical fashion. Using asterile technique, a fluoroscope was brought into20A 22-gauge, 10-mm tip radiofrequency cannulawith a bent tip was gently advanced through theanesthetized skin and guided into the respectivetargets as noted above. Next, the radiofrequencysensory and motor stimulation parameters werethen utilized to guide and locate the appropriatetargets. The patient demonstrated paresthesia onmultifidus muscle stimulation at bilateral S1-L4 aswell as L3. She had no significant stimulation orparesthesia on the level of L5 dorsal primary ramus.
-9-10DDICICCardiovascularClinical Documentation21MENUBACK NEXT
-10ICDICD-9MENUBACK NEXTClinical DocumentationCardiovascular RequirementsThe following items should be documented as appropriate to allow complete coding under ICD-10Laterality : Left, right, bilateral, multiplelocationsStatus of : AcuteDisease : Chronic: Intermittent: Recurrent: Transient: Primary: SecondaryDiabetes : Type I, Type II or due to otherdisease / drug: Link Diabetes tocomplicationsNervous : Primary versus secondarySystemdisease and cause: Presence of Intractabledisease22Nervous : Level and type of paralysisSystemCirculatory : Acute Myocardial InfarctionSystemtime period is 4 weeks: Link complications toHypertension: Systolic versus diastolicheart failure: Left versus right heart failureRheumatic versus nonrheumatic disease: Traumatic versus nontraumatic cerebralhemorrhage and cause ofhemorrhage or infarction: Artery blockedor ruptured
-9-10DDICICClinical DocumentationCardiovascular RequirementsThe following items should be documented as appropriate to allow complete coding under ICD-10Respiratory : Exacerbation of chronic diseaseSystem : Effects of tobacco use/exposure on respiratory systemGenitourinary : Primary versus secondary disease: Stage of chronic kidney disease: Link infectious agent or cause to disease23MENUBACK NEXT
-9-10DICDICMENUBACK NEXTClinical DocumentationCardiovascular Clinical ScenarioProcedures Performed1. Left and Right heart catheterizationmedical therapy and presents today for potential2. Left ventriculography and coronaryangiographyocclude device. Risks/benefits ratio of procedure3. Intracardiac echocardiographyIndication1. Secundum-type atrioseptal defect.2. Congestive heart failure, chronic, systolic.Brief History of Present Illnessclosure of this defect with a percutaneous septalwere explained and informed consent wasobtained.ComplicationsNone immediateHemodynamic Findings1. AC 120/78 (94mm Hg mean)2. LV 120/17mm Hg)Procedure3. RA 16 (12mm Hg mean)On arrival to the lab, the patient was in stable4. RV 45/11 mm Hg meancondition. Initially a 5-French sheath was placed5. PA 45/17 (32mm Hg mean)in the right common, femoral vein. A 5-Frenchsheath was placed in the left common femoralThis is a 63 year old who has chronic dyspneaartery. Hemodynamics was measured using sheathon exertion consistent with CHF NYHA class III,side arms, as well as using a 7-French pulmonarywith most recent echocardiogram on 3/3/2014artery Swan-Ganz catheter (after upgrading sheathejection fraction rate of 45%. Outpatient evaluationto 1-French). Intracardiac echocardiography wasrevealed pulmonary hypertension and dilatedperformed using an AcuNav 10-French intracardiacpulmonary artery. Subsequent noninvasive testing,echocardiography catheter with standardan echocardiogram, as well as a coronary CTtechnique.angiography, revealed a large Secundum-type24atrial septal defect. He has been managed with6. PCWP 19 mm Hg mean7. Oximetry Run- SVC 71%, RA 84%, PA 88 4%, FA91%8. System blood flow 6.14 liters per minute.Pulmonary blood flow 47 liters per minute withQp/Qs ration 7 69 (assumed hemoglobin of 15.7gm/dL, assumed oxygen consumption of 258mL per minute).
-9-10DICDICMENUBACK NEXTClinical DocumentationCardiovascular Clinical ScenarioAngiographic FindingsLeft Main: Normal. Has a very short left main.Left Anterior Descending: NormalLeft Circumflex: Left circumflex artery terminates25pulmonary vein. Subsequently, an intracardiacechocardiogram catheter was advanced andparked in the right atrium and detailed interrogationof the interatrial septum was performed usingstandard technique. There was a large secunduminto 3 large CM branches without any significanttype atrial septal defect. There was no posteriordisease.rim detected in the midsegment. The anterior rimRight Coronary Artery: Arising from a slightlywas adequate. In light of the above we electedanterior position in the right coronary cusp. Thisto assess the accurate sizing and flow cessationvessel has a very large conus branch arisingwith a sizing balloon. An Amplatz Super-Stiff wirealmost in an anomalous fashion right at its origin,and subsequently a J-wire were parked in the leftand supplies the right ventricle. This has multipleatrium, over which a 30mm NMT sizing balloonlarge branches. The main RCA and posteriorwas advanced and inflated across the interatrialdescending arteries are free of significant disease. Aseptal. This balloon at 30mm still had somemultipurpose 5-French catheter was advanced andresidual minimal shunting on the posterior rim andinitially this wire went to an area outside the rightthere was some give with motion. After detailedatrial free border. In light of the above, anomalousdiscussion with Dr. Benway, an interventionalpulmonary venous drainage was suspected.cardiologist, we elected not to proceed with anyThis multipurpose catheter was advanced andattempts at percutaneous device closure becausepulmonary vein angiography was performed.of the above findings. All equipment was removed,This was the right upper pulmonary vein, drainingand access site hemostasis was to be achievednormally into the left atrium and was not anomalouswhen ACT was less than 160 seconds.Impression1. A large secundum-type atrial septal defect, andnot suitable for percutaneous closure.2. Elevated right heart filling pressure with mildpulmonary hypertension and significant left toright shunt at the atrial level (Qp/Qs ration morethan 7).3. No significant epicardial coronary artery stenosis.Plan and RecommendationsThis patient’s detailed intracardiacechocardiography and the right and left heartcatheterization confirm hemodynamicallysignificant secundum-type atrial septal defect.Based on the technical factors delineated above,this will be best served with surgical closure. I willdiscuss the case with a cardiothoracic surgerycolleague, and then proceed further as appropriate.Patient will require close follow up, and I havetaken the liberty of adding low-dose ACE inhibitortherapy to optimize his perioperative outcomesfrom a remodeling standpoint.
-9-10DDICICDermatologyClinical Documentation26MENUBACK NEXT
-9-10DICDICMENUBACK NEXTClinical DocumentationDermatology RequirementsThe following items should be documented as appropriate to allow complete coding under ICD-10Laterality : Left, right, bilateral, multiplelocationsStatus of : AcuteDisease : Chronic: Intermittent: Recurrent: Transient: Primary: SecondaryInfections : Link infective organism anddisease processNeoplasms : Malignant versus benign,primary, secondary, In Situ: Detailed locations: Overlapping sites versus different, distinct locations27Diabetes : Type I, Type II or due to otherdisease / drug: Link Diabetes tocomplicationsSkin : Link infectious agent or causeto disease: Pressure ulcer – Detailed site,laterality and stage I – IV: Non-pressure chronic ulcer –Site, laterality and:: Skin breakdown: Fat layer exposed: Necrosis of muscle: Necrosis of bone: Contact dermatitis –document reason
-9-10DICDICMENUBACK NEXTClinical DocumentationDermatology RequirementsThe following items should be documented as appropriate to allow complete coding under ICD-10Musculoskeletal : Past infection, past trauma, other disease processes: Link infectious agent or case to disease: Arthritis – Rheumatoid versus Osteoarthritis: Primary, post-traumatic, or secondary disease: Pathological Fracture due to osteoporosis, neoplastic disease or other causeGeneral Injuries : Detailed locations (Head, Shaft, Proximal, Distal, individual body part, etc): Episode of care (Initial, Subsequent, Sequela)Cause of Injury : Mechanism – How it happened (struck by basketball): Place of occurrence - Where it happened (high school): Activity – What patient was doing (playing basketball): External cause status – Military, Civilian, Work-related, Leisure28
-9-10DICDICMENUBACK NEXTClinical DocumentationDermatology Clinical ScenarioSubjectiveObjectiveReturning 81 year old caucasian female patientVital signs are found in the back of the chart. Bloodor bone was observed.seen today after request by Dr. Reynolds atpressure ideal at 120/80 and temperature 98.9.EXT: No edema. No bruising.Lakeside nursing home. Patient has beenPatient’s BMI was 20.1.recovering after a fall in her home when sheAssessmentbecame unbalanced vacuuming her kitchen floor.FACE: Lesion was observed on patient’snose just to the right of the nasal bridge andPatient had complaint of pain on lower back justPatient has stage 2 pressure ulcer on sacrum. Skinabove supratip break across the nose to theabove buttock. Following up on ulcer last weeklesion on nose confirmed malignant melanoma.tear trough of the patient’s right side [detailednurse also requested Dr. Reynolds to examine aExamlesion that is multicolored with unusual borderson patient’s nose that is normally covered up bymakeup. Patient had stated she has always had a“beauty mark” there, but had noted it has grown inpast few months, as well as changed in color. Lastweek we had taken a biopsy and now returningGEN: Patient alert and appears slightlyuncomfortable.CV: No murmur.RESP: No crackles, rales, or wheezing.to patient with results. I did not take entire lesionABD: Patient’s abdomen was not tender tolast week due to its size. All other systems werepalpitation. However, there was pressure ulcernegative.center on sacrum [detailed location]. Fat layerwas exposed [detailed stage information]as patient’s skin was quite thin and prone to29breakdown. No exposure or necrosis of musclelocation]. It is approx. 2.8 cm across with reddishappearance without clear borders.Plan1. Malignant melanoma on nasal bridgeextending to right tear trough of patientperformed removal of lesion with complexclosure total of 3.2 cm excised.2. Sacral pressure ulcer stage 2.3. Will follow up with patient next week tocheck if healing.
-9-10DDICICDiagnostic RadiologyClinical Documentation30MENUBACK NEXT
-9-10DICDICMENUBACK NEXTClinical DocumentationDiagnostic Radiology RequirementsThe following items should be documented as appropriate to allow complete coding under ICD-10Findings : The report should use appropriate anatomic, pathologic,and radiologic terminology todescribe the findingsPotential : The report should, whenlimitationsappropriate, identify factorsthat may compromise thesensitivity and specificity ofthe examinationClinical : The report should address orissuesanswer any specific clinicalquestions. If there are factorsthat prevent answering theclinical question, this shouldbe stated explicitly31Comparison : Comparison with relevantstudies andexaminations and reportsreportsshould be part of the radiologic consultation andreport when appropriateand availableImpression : Unless the report is brief eachreport should contain an“impression” or “conclusion”: A specific diagnosis shouldbe given when possible: A differential diagnosisshould be rendered whenappropriate
-9-10DICDICMENUBACK NEXTClinical DocumentationDiagnostic Radiology RequirementsThe following items should be documented as appropriate to allow complete coding under ICD-10Impression : Follow-up or additional diagnostic studies to clarify or confirm the impressioncont.should be suggested when appropriate: Any significant patient reaction should be reportedStandardized : Standardized computer-generated template reports should be designed tocomputersatisfy the above criteriageneratedtemplatereports32
-9-10DICDICMENUBACK NEXTClinical DocumentationDiagnostic Radiology Clinical ScenarioReferring PhysicianJohn Doe, MDIndications for Study1. Spinal stenosis.curvature. Marrow signal within the bonystructures is unremarkable.At C7-T1, there is no focal disk disease.ImpressionSome mild multilevel disk disease, as describedabove, with some disk bulges and posteriorosteophytes. There is no frank disk herniationAt C6-7, there is a disk bulge which causes mildMRI of the Lumbar Spineflattening of the anterior CSF space and some3. Bilateral leg numbness.Sagittal and axial images were obtained. The upperneural foraminal narrowing, left greater than right.lumbar spine is not well visualized due to body4. Weakness in hands.At C5-6, there is a combination of disk bulge andCervical and Lumbar Spine MRIposterior osteophytes, which narrows the neural2. Low back pain.Due to the patient’s body habitus and size, thepatient could not be moved further into the coilforamina and flattens the anterior CSF space, moreso than at the C6-7 level.habitus and positioning within the coil. The conusappears grossly within normal limits, normal inlocation and signal intensity. The marrow signalappears within normal limits. There is markednarrowing at L5-S1 with some apparent fusionand visualization of the upper lumbar spine is veryAt C4-5, there is a disk bulge, which flattens theat this level to the left of midline. There is somelimited. The patient’s head was also squeezed intoanterior CSF space and causes some bilateralminimal scoliosis. Marrow signal within the bonythe cervical spine coil and was very uncomfortableneural foraminal narrowing, left greater than right.structures is unremarkable.during the study.MRI of the Cervical SpineSagittal and axial images were obtained. Thecraniocervical junction is within normal limits.Spinal cord is normal in location and signal33intensity. There is straightening of the normalAt C3-4, there is a combination of bone and disk,which slightly flattens the anterior CSF space andnarrows the neural foramina bilaterally.
-9-10DDICICClinical DocumentationDiagnostic Radiology Clinical ScenarioMRI of the Lumbar SpineImpressionAt L5-S1, the nerve roots exit normally. There is some1. There is some slight trilateral narrowing at L3-4.The nerve roots exit more normally on the nextimage.slight right neural foraminal narrowing on one imagedue to a combination of bone and disk; however, theneural foramina are patent on the next image.At L4-5, there is a mild disk bulge and posteriorfacet degenerative changes. Nerve roots arepatent.At L3-4, there are some mild posterior facetdegenerative changes, thickening of theligamentum flavum, and neural foraminalnarrowing. On the next image, the nerve roots exitnormally.342. At L4-5, there is a disk bulge and some posteriorfacet degenerative changes.3. At L5-S1, there is a bulging disk and narrowingon the right with slight right neural foraminalnarrowing on one image. On the next, the neuralforaminal are more patent. There is no focal diskherniation.MENUBACK NEXT
-9-10DDICICEndocrinologyClinical Documentation35MENUBACK NEXT
-10DICD-9MENUICBACK NEXTClinical DocumentationEndocrinology RequirementsThe following items should be documented as appropriate to allow complete coding under ICD-10Laterality : Left, right, bilateral, multiplelocationsStatus of : AcuteDisease : Chronic: Intermittent: Recurrent: TransientInfections : Link infective organism anddisease processNeoplasms : Malignant
ICD-10 will fully replace ICD-9. On March 31, 2014, the US Senate voted to approve H.R. 4302, Protecting Access to Medicare Act of 2014. This included language delaying the implementation of ICD-10 to October 1, 2015. ICD-10: Future ICD-10 is not a simple update to ICD-9. The structural changes throughout the coding system are