Transcription
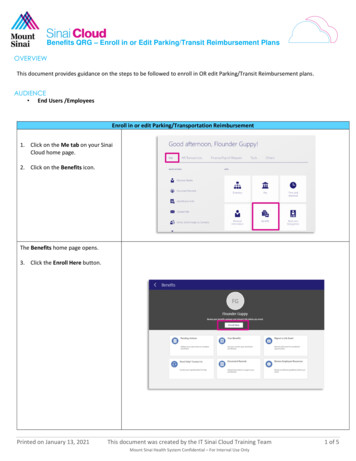
FEBRUARY 2021 VOL. 8Reimbursement andPayor Dispute UpdatePOLSINELLI REIMBURSEMENT TEAM NEWSLETTERWhy Should I Attend the 2021 Reimbursement [Virtual] Summit?R. Ross Burris, IIIShareholderAtlantaOn February 23 and 25, 2021, Polsinelli’sReimbursement Institute is hosting itsFifth Annual Reimbursement Summit as atwo‑part virtual series. Please reserve timeon your calendars to join us online for thismultiday educational and networking event!Similar to prior years, attendees can obtainCLE or CPE credits for attending.1 Unlikeprevious years, this event will be completelyonline and held over two half-days, asopposed to one long day, to allow moreflexibility to attend sessions. While we willmiss sharing a drink and snacks with friendsand colleagues, we are particularly excitedabout this virtual event because it willallow even more people to participate whopreviously may have been limited by travel orschedule restrictions.The goal of the Reimbursement Summit hasalways been to focus on key health careregulatory and reimbursement developments,including recent litigation and appeals ofimport to health care providers, and we willmaintain that focus with this year’s virtualformat. The Reimbursement Summit is a greateducation and networking opportunity forhealth care professionals ranging from thosein the executive suite and the counsel’s officeto finance, reimbursement/revenue cycle,operations, and compliance.If the pandemic has taught usanything, it’s that our clientsneed to be prepared to domore with fewer resources.Some may think that they don’t have time foranother video conference. Few have time forcontinuing education, and finding relevanteducation that will actually give them tools tohelp drive their organization’s reimbursementgoals is nearly impossible. Regardless ofwhich provider space you come from, youwill find this seminar highly relevant to yourday-to-day operations and strategic plans for2021 and beyond.Join us to hear health care reimbursementexperts from Polsinelli share their in-depthknowledge on the following topics:The Year in ReimbursementThis session will offer a high-level reviewof new laws and regulations from the lastyear — including what you may have missedwhile focusing on COVID-19 — affecting bothsmall and large health care providers acrossthe spectrum.Strategies for Complying withPrice Transparency and SurpriseBilling LawsState legislatures and the federal governmenthave been busy the past 12 months churningout laws that impose new disclosure andbilling obligations on providers, and thissession will help you get your practices upto date.Reimbursement for Innovations —Updates on Value-Based Care andother Innovation ModelsThrough actions of federal, state and theprivate sectors, “value-based” goals andmethods have become more embeddedin the nation’s health care payment anddelivery systems. These changes presentopportunities and challenges for providers,States eligible for CLE or CPE credit include the following: Arizona, California, Colorado, Georgia, Illinois, Kansas, Louisiana, Missouri, Mississippi, New Jersey,New York, North Carolina, Ohio, Pennsylvania, Tennessee, Texas, Virginia, Washington and Wisconsin.1CON TIN U ED ON PAGE 2reimbursementinstitute.polsinelli.comPOL SINELLI REIMBURSEMENT TE AM NE WSLE T TER 1
CON TIN U ED F ROM PAGE 1Table of ContentsWhy Should I Attend the 2021Reimbursement [Virtual] Summit?investors and others, and this session willexplore the movement from traditional feefor service to financial and other risk-basedpayment models.Value-Based Care in 2021:Five Emerging Trends inValue-Based CareReimbursement and COVID-19 —Updates on Provider Relief, Testing,Vaccinations, and What Waivers Maybe Here to StayThe “No Surprises” Act:Congress Enacts Legislation toEnd Surprise Medical Billing inOmnibus Year-End Spending BillThe pandemic isn’t over just becauseyou’re over it. Learn about the latest newson provider relief, reimbursement issuesfor testing and vaccinations, and mostimportantly, what waivers may be here to stay.Payors Pick Up Pacein Curbing PreventableSpending on Surgical CareWho’s Going to CoverCOVID Hospitalizations —Commercial Health Plans orWorkers’ Compensation?Physicians and Other ProvidersCan Now Sue Insurers forDouble Damages Under theMedicare Secondary Payer LawEffective Strategies for TelehealthReimbursement, Now andPost‑PandemicDuring this session, speakers will addresstelehealth initiatives that have beenaccelerated during the last year and effectivestrategies to help you through the rest of thepandemic and beyond.Trends in Commercial Payor Disputesand How to Contract Around ThemPayors are under a lot of pressure to crackdown on billing errors and fraud, whichmeans more providers and suppliers arebeing subjected to audits and inquiries fromevery angle. During this session, the panelistswill address the latest trends (and tricks) bypayors and offer tips on how you may be ableto contract around those issues in the future.We hope everyone can join us forboth days, or even just for yourfavorite session. Click here formore details and to register.If you have additional questions,please email Sinead McGuire atsmcguire@polsinelli.com.COVID-19: What YourBusiness Needs To KnowClick here to join our mailing list andreceive new blog posts, event informationand COVID-19 legal updates direct to youremail inbox.reimbursementinstitute.polsinelli.comPOL SINELLI REIMBURSEMENT TE AM NE WSLE T TER 2
Value-Based Care in 2021: Five Emerging Trends in Value-Based CareJeanna PalmerGunvilleShareholderChicagoLori A. OliverShareholderSeattleKathleen SnowSuttonAssociateDenverThe pace and pressure to embracevalue-based care are picking up. TheCOVID-19 pandemic exposed the risks andlimitations of reliance on fee-for-servicereimbursement and, combined with thegroundbreaking changes in health caredelivery models and regulatory flexibility,indicate a renewed focus on value-basedcare. This article outlines five of the toptrends to watch for in value-based carefor 2021.Top Five Trends to Watch in 2021Leaning In to Value-Based CareContinued Innovationand DisruptionCapitalizing onCOVID-19 InfrastructureNew Opportunities forProvider AlignmentEmphasis on SocialDeterminants of HealthLeaning In to Value-Based CareOne of the lessons from 2020 is that relianceon fee-for-service can leave providersvulnerable to volatility and changes indemand. As utilization plummeted duringthe COVID-19 pandemic, providers who hadinvested heavily in value-based care havebeen better able to weather the pandemicand the economic downturn by having aconsistent source of revenue despite lowutilization.1 The rapid changes in healthcare driven by the pandemic only furtheremphasized the need for providers to leaninto value-based care. Beyond the allureof steady revenue streams, new regulatoryflexibilities and care delivery innovationcreates an opportunity for providers torealize a more rapid rate of return on theirinvestment in value-based care by increasingthe portion of their business with value-basedcare reimbursement.Continued Innovation and DisruptionWhile value-based care has always beenan area ripe for innovation, 2021 presents aunique set of circumstances that point to asurge of innovation and disruption in bothpayment and care delivery models. Valuebased care had been a priority for the Centersfor Medicare and Medicaid Services (“CMS”)under the Trump administration,2 but thereis no reason to expect a change of courseaway from value-based care.3 In fact, theBiden administration’s health care goals willlikely require an increased emphasis on costsavings, which may result in an even greaterpush towards value-based care.4 Some newsoutlets are reporting that Elizabeth Fowler isa front-runner to lead the Center for Medicareand Medicaid Innovation,5 further signalingthat CMS’s momentum on value-basedcare will continue.6 Commercial payors alsocontinue to push towards innovative paymentand care models as COVID-19 has highlightedthe inequities in the health care deliverysystem and challenges for providers.Capitalizing onCOVID-19 InfrastructureThe COVID-19 pandemic promptedtransformational changes to the health caresystem that portend continued opportunitiesto manage patient care and provide qualitycare in lower cost settings. As a result ofthe pandemic, both the federal and stategovernments threw open the doors to allowproviders to furnish services via telemedicineand other digital health modalities duringSee, e.g. Jacqueline LaPointe, How COVID-19 Imperiled Physician Practices and How to Save Them, RevCycle Intelligence (May 6, 2020), eriled-physician-practices-and-how-to-save-them; How Value-Based Care Supports Doctors During the Pandemic, BlueCrossBlueShield of Illinois (Sept. 9, 2020), c.2See, e.g. Press Release, CMS, Fact Sheet: Value-based Care State Medicaid Directors Letter (Sept. 15, 2020), tate-medicaid-directors-letter; Press Release, CMS, CMS Announces Strong Participation in Value-Based Medicare Advantage Model for CY2020 and New Opportunities for 2021 (Dec. 19, 2019), -model-cy-2020-and-new; Press Release, CMS, Direct Contracting: Professional and Global (Nov. 25, 2019), g-professional-and-global.3Keith Loria, What Will CMS Do Under the Biden Administration?, Managed Healthcare Executive, cms-dounder-the-biden-administration- (last visited Feb. 10, 2021).4See, e.g. Health Care, Biden Harris Campaign, joebiden.com/healthcare/.5Shira Stein, Obamacare Architect Is Top Pick to Lead Value-Based Care Office, BloombergLaw: Health Law & Business News (Feb. 10, 2021), re-office6See, e.g. Courtney Taylor, COVID-19 May Move the Needle on Value-Based Payment, USC Shafer (Sept. 24, 2020), needle-on-value-based-payment/.1CON TIN U ED ON PAGE 4reimbursementinstitute.polsinelli.comPOL SINELLI REIMBURSEMENT TE AM NE WSLE T TER 3
CON TIN U ED F ROM PAGE 3the COVID-19 public health emergency.7Many of the telehealth waivers have beenmade permanent.8 Providers who haveembraced digital health as a way to weatherthe pandemic will also have the opportunityto capitalize on this investment as a way tomanage patient care and see a return oninvestment for services that are typicallynot reimbursable under fee-for-servicearrangements.9 CMS also created theHospital Without Walls10 and Acute HospitalCare at Home11 programs to increase hospitalcapacity during the pandemic. Commercialpayors have been eager to seize on theseopportunities to promote lower-costservices.12 Providers who have invested inthese types of programs similarly providean opportunity to provide quality care inlower cost environments, which will benefitproviders who are fully engaged in valuebased care.New Opportunities forProvider AlignmentRecent changes to federal law aim to lowerbarriers to value-based care. In particular,CMS and the Office of Inspector General(“OIG”) created new flexibility under the StarkLaw and Anti-Kickback Statute for valuebased arrangements to allow providers toenter into value-based care arrangementsthat previously may have been prohibited.13While the new exceptions and safe harborsstill require that arrangements be carefullycrafted, they provide new opportunitiesto align with providers and to incentivizeactivities that promote value-based goalsthat were previously unavailable. Additionally,the sweeping interoperability and informationblocking rules aim to ensure that patientsand providers are able to access healthinformation, further reducing structuralbarriers to value-based care.Emphasis on Social Determinantsof HealthFinally, players in the value-based carespace — particularly in Medicaid managedcare programs — are placing greateremphasis on addressing social determinantsof health.14 Providers and payors arebeginning to recognize the crucial role thatnonmedical factors play in patient health.15By solving for these issues — such astransportation, food, housing, languageservices, etc. — providers and payorsare able to realize significant benefits inimproving patient health and outcomes whilekeeping medical costs relatively low. Thefocus on social determinants of health is anemerging trend in value-based care that islikely to grow as players seek creative waysto manage patient care through valuebased arrangements.As providers and payors emerge from theupheaval of the pandemic and the resultingrevolutionary changes in health care, we canexpect renewed interest in value-based care.Opportunities abound to capitalize on thechanges wrought by the pandemic, as wellas emerging prospects, by fully investing invalue-based care.See, e.g., Telehealth, Polsinelli, www.covid19.polsinelli.com/telehealth?rq telehealth (last visited Feb. 10, 2021); General Provider Telehealth and TelemedicineToolkit, CMS, olkit.pdf (last visited Feb. 10, 2021).8See, e.g. Press Release, CMS, Trump Administration Finalizes Permanent Expansion of Medicare Telehealth Services and Improved Payment for Time DoctorsSpend with Patients (Dec. 1, 2020), health-servicesand-improved-payment9See LaPointe, supra n.1.10Pres Release, CMS, Fact Sheet – Additional Background: Sweeping Regulatory Changes to Help U.S. Healthcare System Address COVID-19 Patient Surge(Mar. 30, 2020), rge; re-home-faqs.pdf12See, e.g. Acute Hospital at Home Program, Frequently Asked Questions, %20Payer%20Telehealth%20Coverage%20Reportfinal.pdf (last visited Feb. 10, 2021); Press Release, Humana, DispatchHealth and Humana Team Up to Provide Hospital-Level Care in theHome (Feb. 1, 2021), Care-in-the-Home/default.aspx#gsc.tab 0.13Lori Oliver, Neal Shah, Jeanna Gunville, Kathleen Sutton, A New Framework: CMS and OIG Modernize the Stark Law and Anti-Kickback Statute, Polsinelli(Dec. 8, 2020), ize-stark-law-and-aks.14Addressing Social Determinants of Health & Equity Through Health-Related Services, Oregon Health Authority (Mar. 2020), ated-Services-SDOH-E-Guide.pdf; Social Determinants of Health Dashboard, Wa. State Dep’t Health, s (last visited Feb. 10, 2021); Marrying Value-Based Payment andthe Social Determinants of Health through Medicaid ACOs: Implications for Policy and Practice, Milbank Memorial Fund (May 22, 2020), tice/.15Jacqueline LaPointe, Social Determinants of Health Key to Value-Based Purchasing Success, RevCycle Intelligence (Jan. 9, 2019), ON TIN U ED ON PAGE 5reimbursementinstitute.polsinelli.comPOL SINELLI REIMBURSEMENT TE AM NE WSLE T TER 4
The “No Surprises” Act: Congress Enacts Legislation to EndSurprise Medical Billing in Omnibus Year-End Spending BillCON TIN U ED F ROM PAGE 4Key FeaturesDavid A. KingShareholderNashvilleJoshua D. ArtersAssociateNashvilleSamantha M. FlenerAssociateNashvilleProhibition on Balance Billing. The Actprohibits out-of-network providers/facilitiesfrom balance billing patients for morethan the in-network cost sharing amountfor emergency services (and ancillaryservices), and nonemergency servicesrendered by out-of-network providersat in-network facilities (when the noticeand consent criteria described below arenot met).Right to Direct and Timely Payment. TheAct requires health plans to pay providersdirectly an initial “out-of-network rate,” asspecified in the Act, thereby eliminatingany impact from anti-assignment clausesgoverned by ERISA and exempt fromstate law.Three Possible Out-of-Network Rates:Detailed Notice and ConsentRequirements for NonemergencyServices. The notice and consent criteriagenerally require nonparticipatingproviders/facilities to:The recently-enacted ConsolidatedAppropriations Act, 2021 includes the longdebated “No Surprises” Act (the “Act”),which addresses how providers are paid forcertain out-of-network health care services,and removes patients from the middle ofout-of-network reimbursement disputes.The Act comprehensively addressesall types of commercial health plansby amending the Public Health ServiceAct (“PHSA”), the Employee RetirementIncome Security Act of 1974 (“ERISA”),the Internal Revenue Code (“IRC”), andFederal Employees Health Benefits Program(“FEHBP”), each with substantially similarcompanion provisions. These provisions,summarized in brief below, will be effectiveJanuary 1, 2022. Agency rules are expectedto start rolling out in July 2021.Provide a written notice to patients.Obtain consent to be treated by anonparticipating facility/provider.Provide a signed copy of the consent tothe patient.Cost Estimate Requirement for ScheduledServices. The Act requires a provider togive a good faith estimate of charges tothe patient’s health plan, generally withinthree days of the patient scheduling aservice. The health plan is then requiredto provide an advanced EOB showing theprovider’s network status, contracted rate,good faith estimates of patient cost-sharingand the amounts the plan will pay, certaindisclaimers, and other information detailedin the Act.If there is an All-Payer Model Agreementin the State, then the amount specified inthe Model Agreement should be used asthe out-of-network rate.If there is no All-Payer Model Agreement,then a state-law-specified amount wouldbe the out-of-network rate if the statelaw governs each of:The item/service furnished.The provider/facility.The plan/coverage/issuer.If there is no All-Payer Model Agreementand no state law governing, then theamount that the parties agree on(including any agreements from themore formal negotiation proceduresdetailed later in the Act) is the out-ofnetwork rate.Patient/Provider Dispute Resolution. TheAct calls for the Secretary to establish aprocess by which uninsured individuals canchallenge bills substantially in excess ofgood faith estimates provided pursuant tothe cost estimate requirement above.ScopeThe Act applies to emergency services provided bynonparticipating facilities/providers and air ambulanceservices, and nonemergency services rendered bynonparticipating providers at participating facilities(unless a detailed notice and consent requirement ismet). The Act covers all commercial plans governedby state and/or federal law.CON TIN U ED ON PAGE 6reimbursementinstitute.polsinelli.comPOL SINELLI REIMBURSEMENT TE AM NE WSLE T TER 5
CON TIN U ED F ROM PAGE 5Provider/Health Plan Dispute Resolution.The Act sets forth a detailed disputeresolution procedure for providers andhealth plans that do not agree on the outof-network rate. The procedure begins withan open negotiation process. If the providerand plan cannot reach an agreementthrough the open negotiation process,one party may escalate the dispute toindependent dispute resolution known inthe Act as the “IDR Process.” Both partiesmust then submit their “offer”, i.e. theirargued price for the disputed item/service.The IDR Process is baseball-style, meaningthe arbitrator must select one party’s offer.Quality and outcomes.Case mix.Provider/plan market share.A hospital’s teaching status.Any other nonprohibited informationrelating to the offer submitted byeither party.Provider’s billed charges.Medicare rates.Median in-network rates.Medicaid/CHIP rates.Provider’s training and experience,patient acuity, and the complexity ofthe service.TRICARE rates.Good faith efforts (or lack thereof) tobecome an in-network provider.the IDR Process cannot initiate another IDRProcess against the same adverse party fordisputes related to the same item/servicesduring a 90-day “cooling-off” periodfollowing the arbitrator’s decision.Information the Arbitrator MayNot Consider:Information the Arbitrator May Consider:Contracted rates during the previousfour years.Effect of IDR Decision. Absent some likelyrare exceptions, like fraud, the arbitrator’sdecision in the IDR Process is not subjectto judicial review. The party who initiatedVoluntary Process. The IDR process isvoluntary and does not prohibit the use oftraditional litigation or other agreed disputeresolution processes.Timely Bills. The Act imposes a frameworkon providers and plans with the goal ofsending timely bills to patients.Provider Directories. The Act takes actionto make accurate provider informationavailable to patients, so they can determinewhich providers are in their network.All Payer Claims Databases. The Actestablishes one-time grants for states thatsubmit applications to create State AllPayer Claims Databases.Payors Pick Up Pace in Curbing Preventable Spending on Surgical CareKara M. FriedmanShareholderChicagoBrittany L. StrandellAssociateKansas CityIn 1982, the ambulatory surgery center(“ASC”) model began to proliferatewhen Medicare approved this type ofprovider as an appropriate site of care forapproximately 200 surgical procedures. Yet,despite their lower cost, nearly 40 yearslater, commercial and government payorshave not forced the migration of outpatientsurgical care to ASCs.As such, outpatient surgical proceduresremain a mainstay for many health systemsto ensuring hospitals maintain a healthyfinancial position. However, recent trends inCenters for Medicare and Medicaid Services(“CMS”) regulations as well as commercialpayor reimbursement policies demonstratenew enthusiasm from payors to guide theirenrolled providers and plan beneficiaries tolower-cost settings outside of the hospitaland relatedly to restrict health systems andphysicians from retaining elective outpatientsurgical services in the hospital setting.Illustrating this trend, some payors, such asUnitedHealthcare (“UHC”) and Anthem, havepromulgated policies that restrict the site ofcare for elective surgical procedures. UHC’spolicy took effect in November 2019 for fullyinsured groups in most states.1 Pursuantto this policy, UHC only pays for surgicalprocedures performed in an outpatienthospital setting if such setting is medicallynecessary based on the acuity of thepatient. For example, the freestanding ASCsetting can be a riskier setting for patientswho, based on their health condition, mayhave complications with anesthesia. UHCmay also permit elective surgical care inthe hospital setting if ASC services are notgeographic accessible. UHC stated its intentto reduce costs with this new requirement.UHC estimated that steering beneficiariestoward the lower-cost setting would savebeneficiaries 500 million in 2020 and wouldsave UHC over 20% in reimbursementto providers.Similarly and more recently Anthem,which has insurance products in 15 states,published a Clinical UM Guideline onAugust 20, 2020, which also limits the useof outpatient hospital surgical facilities.2The Anthem guidelines consider the useof outpatient hospital facilities medicallynecessary only if: (a) the procedure is of alevel of complexity that it cannot be safelyperformed in a less intensive setting; or(b) the individual has a clinical conditionthat may compromise the safety of alower-cost setting, such as conditions thatrequire enhanced anesthesia monitoring,UHC, Outpatient Surgical Procedures – Site of Service (eff. Nov. 1, -procedures-site-service-11012019.pdf.2Anthem, Ambulatory or Outpatient Surgery Center Procedures (CG-SURG-10) (last rev. Nov. 5, uidelines/gl pw a051150.html.CON TIN U ED ON PAGE 71reimbursementinstitute.polsinelli.comPOL SINELLI REIMBURSEMENT TE AM NE WSLE T TER 6
CON TIN U ED F ROM PAGE 6medications, or prolonged recovery orwhere the patient is at an increased risk forcomplication due to severe comorbidity. Allother uses of an outpatient hospital facilityare not medically necessary under the policy.Outside of value-based care initiatives, CMShas not yet adopted outpatient surgicalprocedure site of care policies that restrictcertain cases to a nonhospital setting. CMShas, however, developed new paymentpolicies to find ways to reduce the increasingcosts associated with health care services.More specifically, for calendar year 2021,CMS added 11 procedures to the ASCcovered procedures list, including moretotal joint replacement procedures.3 Thisis significant in multiple respects. Fromthe hospital perspective, joint replacementprocedures, which are generally consideredelective and tend to have a better payor mix,have been a profitable source of income forhospitals. From a CMS program integrityperspective, the fiscal burden of jointreplacements on the Medicare programis high and, along with other rising costs,threatens program solvency particularly aslongevity of seniors increases and somepatients begin to outlive their first jointreplacement needing a second procedurelater in life. As CMS has an urgent need toaddress the trust fund’s solvency, movingsurgical care that can be performed in anASC, rather than the hospital, may be oneof several crucial endeavors for the futureof Medicare.per patient was about 12,000 for the ASCand almost 20,000 for the same procedurein the hospital. In keeping with these findings,a report from UnitedHealth Group alsofound that migrating half of routine total jointreplacements to ASCs could yield 1 billionin savings for Medicare, and moving patientsrequiring joint replacement procedures toASCs could minimize the rate of hospitalacquired infections in this population.4 It isunsurprising, then, that certain projectionssuggest that by 2028 approximately 57%of joint replacement procedures will beperformed at ASCs.As suggested by several studies, the potentialsavings of moving total joint replacementprocedures to ASCs is substantial, with thecost of treatment being about 40% less inan ASC when compared to hospital surgicalcare for the same procedure. The estimatedaverage cost for joint replacement surgeryAs in recent years, reducing the health carespend will remain a priority for federal andstate government, other payors, employersand patients alike, and health systems willneed to focus their surgical programs ondeveloping and expanding strategies forlower cost ambulatory surgical care.See CMS, Fact Sheet: CY 2021 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Final Rule (CMS1736-FC) (Dec. 2, em-and-ambulatory-surgical-center-0.4See UnitedHealth Group, New Research Highlights the Safety and Cost Savings Associated with Ambulatory Surgery Centers (Dec. 10, ry-centers-490916.html.3Who’s Going to Cover COVID Hospitalizations —Commercial Health Plans or Workers’ Compensation?Tish R. PickettAssociateLos AngelesC. Ryan MorganShareholderDenverA trend is emerging. Commercialhealth plans are delaying and evendenying reimbursement for COVID-19hospitalizations — especially high-dollarinpatient stays. Plans are attemptingto defer these claims to workers’compensation on the health plans’ assertionthat COVID-19 is a work-related illness.Some hospitals defer to health plans, as itrelates to these types of claims, becauseit is plausible that patients could havecontracted COVID-19 at work and becauseworkers’ compensation is typically primaryfor coordination of benefits purposes.But workers’ compensation is notoriouslycomplex, and hospitals may not understandthe nuances of the program enough to knowwhen it is appropriate to challenge this typeof health plan denial. Failing to appeal thesedenials may impact hospital reimbursement,as well as a hospital’s accounts receivabledays, known as “AR days,” depending on thenumber of COVID hospitalizations and thecorresponding amount in open balances. It isdefinitely a conundrum. The goal of this articleis to provide hospitals and its business officeswith a better understanding of COVID-19 asan occupational illness to enable hospitalsto be better equipped to determine when itis appropriate to challenge health plans thatseek to delay or deny reimbursement forCOVID hospitalizations.Demystifying Workers’ CompensationWith a Brief OverviewIt is important to have a generalunderstanding of workers’ compensationcoverage. Workers’ compensation is astate-mandated insurance program thatprotects employers and employees fromfinancial loss when employees suffer jobrelated injuries and illnesses. Virtually allemployers, even small employers, mustmaintain workers’ compensation coverage.If an employee suffers an occupational injuryor illness, an employer through its workers’compensation carrier may provide missedwage replacement, temporary and permanentdisability, death benefits, and supplementalbenefits. But one of the bas
The pandemic isn't over just because you're over it. Learn about the latest news on provider relief, reimbursement issues for testing and vaccinations, and most importantly, what waivers may be here to stay. Effective Strategies for Telehealth Reimbursement, Now and Post-Pandemic During this session, speakers will address