Transcription
Arthritis Care & ResearchVol. 70, No. 10, October 2018, pp 1431–1438DOI 10.1002/acr.23512 2018, American College of RheumatologyORIGINAL ARTICLEMedical Care Costs Associated With RheumatoidArthritis in the US: A Systematic LiteratureReview and Meta-AnalysisANDREW HRESKO,1 TZU-CHIEH LIN,2ANDDANIEL H. SOLOMON2Objective. Rheumatoid arthritis (RA) is a morbid, mortal, and costly condition without a cure. Treatments for RA haveexpanded over the last 2 decades, and direct medical costs may differ by types of treatments. There has not been a systematic literature review since the introduction of new RA treatments, including biologic disease-modifying antirheumaticdrugs (bDMARDs).Methods. We conducted a systematic literature review with meta-analysis of direct medical costs associated with RApatients cared for in the US since the marketing of the first bDMARD. Standard search strategies and sources were used,and data were extracted independently by 2 reviewers. The methods and quality of included studies were assessed. Totaldirect medical costs as well as RA-specific costs were calculated using random-effects meta-analysis. Subgroups of interestincluded Medicare patients and those using bDMARDs.Results. We found 541 potentially relevant studies, and 12 articles met the selection criteria. The quality of studies varied:one-third were poor, one-third were fair, and one-third were good. Total direct medical costs were estimated at 12,509(95% confidence interval [95% CI] 7,451–21,001) for all RA patients using any treatment regimen and 36,053 (95% CI32,138–40,445) for bDMARD users. RA-specific costs were 3,723 (95% CI 2,408–5,762) for all RA patients using any treatment regimen and 20,262 (95% CI 17,480–23,487) for bDMARD users.Conclusion. The total and disease-specific direct medical costs for patients with RA is substantial. Among bDMARD users,the cost of RA care is more than half of all direct medical costs.INTRODUCTIONRheumatoid arthritis (RA) is a chronic, progressive autoimmune systemic disease affecting approximately 0.7% of thepopulation (1). Treatment for RA was transformed in thelate 1990s with the advent of biologic disease-modifyingantirheumatic drugs (bDMARDs) targeting specific immunologic pathways. As a disease with early adoption ofbDMARDs, RA serves as a model for the use of biologicdrugs, where the treatment costs vary substantially basedon therapeutic strategy.Supported by the NIH (grant AR-K24-055989). Mr. Hresko’swork was supported by the Harold Williams Research Fellowship from Tufts University School of Medicine. Dr. Solomonhas received research support (from grants to Brigham andWomen’s Hospital) from Amgen, Pfizer, Eli Lilly, AstraZeneca,Genentech, Bristol-Myers Squibb, and Corrona.1Andrew Hresko, BA: Tufts University School of Medicine,Boston, Massachusetts; 2Tzu-Chieh Lin, PhD (current address:Amgen, Thousand Oaks, California), Daniel H. Solomon, MD,MPH: Brigham and Women’s Hospital, Boston, Massachusetts.Address correspondence to Daniel H. Solomon, MD,MPH, Division of Rheumatology, Brigham and Women’sHospital, 75 Francis Street, Boston MA, 02115. E-mail:dsolomon@bwh.harvard.edu.Submitted for publication May 18, 2017; accepted inrevised form January 2, 2018.Biologic DMARDs offer alternatives for patients unresponsive to traditional synthetic DMARDs, but the drugscarry an increased financial burden, with annual costsbetween 25,000 and 40,000. Thus, a detailed understanding of the cost of care for patients with RA since the adventof bDMARDs will be of importance to policy-makers,administrators, and physicians. The high cost of RA treatments impacts the use of limited medical resources.There is a body of primary literature examining the costof RA since the introduction of bDMARDs, but a currentcritical review of these studies is lacking. The most recentreviews on cost-of-care research for RA in the US were published before the advent of biologics (2–4). Several morerecent reviews have been published looking at costs outsideof the US (5,6), but these studies have limited relevance tothe US, given the difficulties of comparing costs acrosshealth care systems with different payment structures andsocial priorities.The question of direct medical costs for patients with RAis further complicated by the complexities and lack of standardization in the methodology of cost-of-care analyses.When conducting a cost-of-care analysis, researchers mustmake decisions about the best source of data, the case definition for RA, the financial measure, referred to as “costs,”the elements of medical costs to be included, and theassignment of costs to RA versus other concurrent morbiddiseases. Given the need for better understanding of cost of1431
1432Hresko et alSignificance & Innovations We conducted a systematic literature review withmeta-analysis of direct medical costs associatedwith rheumatoid arthritis (RA) patients cared for inthe US since the marketing of the first biologic disease-modifying antirheumatic drugs (bDMARDs).The 12 articles that met the selection criteriademonstrated that total direct medical costs were 12,509 (95% confidence interval [95% CI] 7,451–21,001) for all RA patients using any treatment regimen and 36,053 (95% CI 32,138–40,445) forbDMARD users.RA-specific costs were 3,723 (95% CI 2,408–5,762)for all RA patients using any treatment regimen and 20,262 (95% CI 17,480–23,487) for bDMARD users.Among bDMARD users, the cost of RA care ismore than half of all direct medical costs.care for RA in the US and the need for standardization incost-of-care analysis, we undertook a systematic literaturereview and meta-analysis with the following PICOS assignments: P (patients) RA patients in the US since 1999; I (interventions) any treatment regimen for RA; C(comparator) no comparison group was included; O (outcomes) direct medical costs; and S (study design) allstudy types were included. We also examined the methodology used in relevant studies.MATERIALS AND METHODSStudy selection. Studies were identified through asearch of Medline using the following medical subjectheading search terms: cost of illness; health care costs;expenditures; expenditures, direct; expenditures, health;expenditures, indirect; rheumatoid arthritis; and arthritis,rheumatoid (full search strategy available in Supplementary Appendix A, available on the Arthritis Care &Research web site at 12/abstract). Because this analysis was meantto consider only studies assessing costs after the introduction of bDMARDs in 1999, the search was limited tostudies published in or after 2000. The last search weperformed was on June 16, 2016.Citations were screened by 1 reviewer (AH) for eligibilitycriteria to select articles for full-text review. Criteria forinclusion were English language, focus on a US population,analysis of post-1999 data, and consideration of total directcosts of treatment for RA from a provider, insurer, or societalperspective. Studies were excluded if they were nonEnglish language, focused on musculoskeletal or rheumaticdisorders other than RA, did not analyze cost as an outcome, were review articles or conference abstracts, focusedon a population outside the US, focused on indirect costs,failed to analyze key elements of total direct cost, studied anongeneralizable population (e.g., only patients with aspecific comorbidity), were economic evaluations of specificdrugs or therapies, relied on pre-1999 data, or provided aninsufficient description of their cost-analysis methodology.Reference lists of studies deemed potentially relevant wereexamined for articles not identified by the Medline search.Full-text review of potentially relevant studies was performedindependently by 2 reviewers (AH and DHS) to confirmeligibility.Data abstraction and quality rating. Two independentreviewers abstracted data from included studies using astandardized form (see Supplementary Appendix B,available on the Arthritis Care & Research web site at 12/abstract). Information abstracted from each study included the characteristics of study participants, such as age, sex, comorbidities,and health insurance coverage, the study’s inclusion andexclusion criteria, cost analysis methodology, and cost-ofcare findings. Specific aspects of the cost analysis examinedwere the definition of RA, methods for comparisons withcosts of non-RA patients, the overall costing methodology,and adjustment for inflation. Regarding costing methodology,some articles used the frequency of utilization of specificservices and multiplied this frequency by a predefined dollaramount; we defined this practice as the utilization 9standardized cost. All abstracted costs were converted to2015 dollars using the consumer price index medical carecomponent.Additionally, we developed a quality rating form basedon the Newcastle-Ottawa Quality Assessment Form forCohort Studies (7), modified to facilitate assessment of RAcost-of-illness analyses (see Supplementary Appendix C,available on the Arthritis Care & Research web site at 12/abstract). Thequality rating included assessment of the representativenessof the studied cohort to assess for risk of selection bias. Thesame 2 reviewers who abstracted data also independentlyrated the quality of included studies. Disagreements regarding data abstraction or quality ratings were resolved by discussion between the 2 reviewing authors.Meta-analysis. The description of the meta-analysisfollowed the Preferred Reporting Items for SystematicReviews and Meta-Analyses checklist (see SupplementaryTable 1, available on the Arthritis Care & Research web siteat 12/abstract). The analysis of costs used a pooled estimate fromrandom-effects models. The variance of the pooled estimates was stabilized by the double arcsine transformation.This method was found to produce less bias and meansquared error than the traditional log transformation (8).We assessed heterogeneity among studies using Cochran’sQ statistic and quantified inconsistencies across studiesand their impact on the analysis by using the I2 statistic (9).All analyses were done using MetaXL software, version 1.4(http://www.epigear.com).RESULTSStudy selection. The Medline search yielded 541citations, and all abstracts were reviewed. Of these, 523
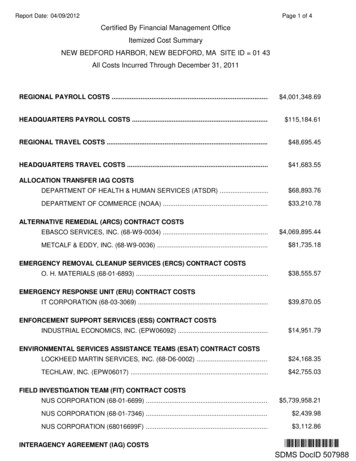
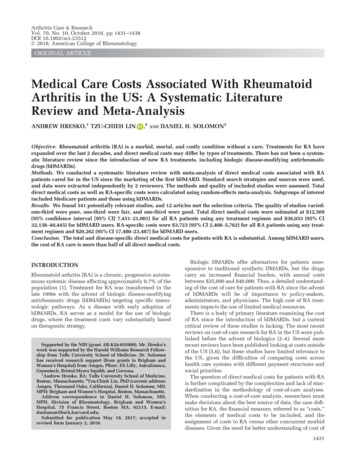
RA Medical Care Costs1433were discarded because they did not meet inclusioncriteria (Figure 1). Of those citations excluded based onabstracts, 364 were excluded because they were not cost-ofillness analyses, 68 because they examined non-US data,62 because they focused on indirect costs or only a subsetof total costs, 18 because they used data from years prior to1999, and 11 because they focused on a population thatcould not be generalized to a national sample, such as onlypatients with a specific comorbidity or using a specificdrug. After full-text review of the remaining 18 articles, 6did not meet the inclusion criteria (2 were excludedbecause they did not describe their costing methodologysufficiently for comparison to other included articles, 2because their populations could not be generalized, and 2because on further inspection their sample included datafrom years prior to 1999). A total of 12 studies wereidentified for inclusion in the review.Data sources, populations, and quality assessment.Table 1 shows the data sources and patient characteristicsof the 12 studies included in final analyses. The includedstudies used a total of 16 different sources of patient datafor their cost analyses. Only 1 database, the MedicalExpenditure Panel Survey, was used in more than 1 of theincluded studies. The included studies analyzed costswithin a number of different medical insurance settings; 6studies reported costs for privately insured patients (10–15), 3 studies reported costs for patients enrolled inMedicaid programs (12,16,17), and 1 study reported costsfor patients enrolled in Medicare (18). Additionally, 3Abstracts iden fiedthrough Medlinesearch(n 541)Abstracts screened foreligibility(n 541)Full-text ar clesassessed for eligibility(n 18)Abstracts excluded due to pre1999, non-English, non-USpopula on, non-cost-of-illnessanalysis, nondirect cost focus,or nongeneralizable popula on(n 523)Full-text ar cles excluded dueto pre-1999, nongeneralizablepopula on, failure to analyzekey elements of total directcost, or insufficient methods(n 6)Studies included inqualita ve synthesisand meta-analyses(n 12)Figure 1. Search strategy results, with the assembly of literaturefor the systematic literature review.studies used patient data from large, national databases andused weighting to generalize their findings to be representative of the entire US population (19–21). One article(12) incorporated costs from multiple insurance settings inthe same set of analyses.Identification of International Classification of Diseases,Ninth Revision, Clinical Modification (ICD-9-CM) codes inthe 714.xx series in medical claims was the most commonmethod for identifying RA patients in claims databases;only 1 study (19) did not rely on ICD-9-CM codes in somecapacity for patient identification. However, there was considerable variability in which codes were used and thenumber of instances of an RA code required for inclusion.Of the 11 studies using ICD-9-CM codes, 4 identified anarrow subset of codes to define RA (10,15–17), while the restaccepted any code within the 714.xx series (11–14,18,20,21).Eight studies (73%) required only 1 instance of an RAcode for inclusion; the remaining 3 (27%) required 1instance of an RA code, or a combination of 1 RA codewith either a claim for at least 1 DMARD or self-reportedRA diagnosis.Most studies included all patients with RA in their chosen database; however, 4 studies limited their populationto only those patients using bDMARDs. All studies, bydesign, analyzed costs incurred after 1999, but none analyzed the costs incurred after 2010. There was an even distribution in the quality of included studies according toour established quality assessment framework: 4 studieswere judged to be of poor quality, 4 were fair quality, and4 were good quality. However, in all studies the observedcohort was deemed to be adequately representative of anational sample, indicating little risk of selection bias.Cost-of-illness analysis methods. Details on the costanalysis methodologies used in the included studies areshown in Table 2. The vast majority of studies based theircost analysis on actual reimbursements paid by an insurerfor medical services or drugs as reported in a claimsdatabase. Michaud et al (19) and Weycker et al (10) insteademployed a utilization-based method in which theyapplied a consistent standardized dollar amount to eachinstance of utilization of a given medical service or drug asreported in a claims database. For a second database,Weycker et al based their cost analysis on charges billed bya health care institution for medical services and drugs, asopposed to the actual reimbursed amount. The findings ofWeycker et al yielded the highest cost estimates in ourdata set.Of the 12 included studies, 10 reported at least 1 elementof cost, such as costs of hospitalizations, ambulatory care,or prescription drugs, specific to care for RA as opposed toother comorbid diagnoses. Of those, 8 reported RA-specificcosts across 3 cost domains and were included in the metaanalysis of total RA costs.Cost-of-care findings. Among the 8 studies including allRA patients (not only those using a biologic DMARD) intheir analyses (12,14,16–21), findings for annual total costof care across all conditions ranged from 3,266 to 25,260,with the lowest estimate being in a population of Medicaidenrollees and the highest in a Medicare population
Truven Health MarketScanCommercial Claims databaseKawatkar (20),2012Simons (21),2012Baser (15), 2015* RA rheumatoid arthritis; TNF tumor necrosis factor.Medical ExpenditurePanel SurveyMedical ExpenditurePanel SurveyMcBride (13),2011Birnbaum (14),2012Harrold (18),2012Arizona HealthQuery databaseIngenix Employer database,Medicare Standard AnalyticalFiles; Florida MedicaidclaimsPrivate insurance claimsdatabasePrivate insurance claimsdatabaseMedicare Current BeneficiarySurveyJohnson (17),2008Birnbaum (12),2010West Virginia Medicaid claimsKhanna (16),2007Wu (11), 2007Private insurance claimsdatabaseNational Databank forRheumatic DiseasesConstella COMPASS database,Ingenix LabRx databaseData sourceMichaud (19),2003Weycker (10),2005Author (ref),yearTNF antagonist biologic agent userswho switched to a new TNFantagonist or a non-TNF biologicagentSample of US populationSample of US populationRA patients enrolled byrheumatologists across USTNF antagonist biologic agent users,ages 65 years in private healthplans across USMedicaid enrollees with RA in WestVirginiaTNF antagonist biologic agent usersamong employees, spouses, anddependents from 31 large employersacross USMedicaid enrollees in MaricopaCounty, ArizonaBeneficiaries from 37 large employersacross US, 5% sample of Medicareenrollees, Medicaid enrollees inFloridaEmployees of 40 large employersacross USEmployees of 40 large employersacross USMedicare enrolleesPopulationTable 1. Included studies and populations*702000: 2252002: 2602004: 2532006: 2475.8 million2004: 34,4032005: 33,6452006: 34,1453,497508372004: 572005: 582006: 59546250Private: 50Medicaid: 4556502,545Private: 14,317Medicaid: 6,4151,4929974771Constella: 166Ingenix: 1141,15762Mean age, years7,527Patients, no.80.577.061.177.831.974.7Private: 70.4Medicaid: 76.683.373.977.476.076.8Female, %1434Hresko et al
No 1 claim with primary Dx of ICD-9CM 714.00 1 claim with primary or secondaryDx of ICD-9 CM 714.xxKhanna (16),2007Wu (11), 2007Johnson (17),2008Birnbaum (12),2010McBride (13),2011YesNo 1 claim with Dx of ICD-9 CM 714.xx 2 Dx of ICD-9-CM 714.xx, OR selfreported RA Dx and 1 Dx of ICD 9CM 714.xx, OR use of biologicDMARD and self-reported RA Dx or1 Dx of ICD-9-CM 714.xxDx of ICD-9-CM 714.xx, OR MEPSclinical classification code of 202Dx of ICD-9-CM 714.xxBirnbaum (14),2012Harrold YesYesNoYesYesYesNoAnalyzedRA costsSum of costs in claims with Dx ofICD-9-CM 714.0x in any position, ordrug on list of RA-relatedmedicationsIncremental costs of RA subjects vs.comparison groupRegression analysisIncremental costs of RA patients vs.comparison groupSum of costs in claims with Dx ofICD-9-CM 714.xx in any position, ordrug on list of RA-relatedmedicationsSum of costs in claims with Dx ofICD-9-CM 714.xx in any position, ordrug on list of RA-relatedmedicationsSum of costs for list of RA-relatedmedicationsSum of costs in claims with Dx ofICD-9-CM 714.xx in any position, ordrug on list of RA-relatedmedicationsPopulation limited to patients withRASum of costs in claims with Dx ofICD-9-CM 714.xx in any position, ordrug on list of RA-relatedmedicationsNANAMethod for determining RA costs* RA rheumatoid arthritis; NA not available; Dx diagnosis; ICD-9-CM Identification of International Classification of Diseases, Ninth Revision, Clinical Modification; MEPS Medical Expenditure Panel Survey. 2 Dx of ICD-9-CM 714.0x at least 2months apartNo 2 claims with Dx of ICD 9-CM 714.xxKawatkar (20),2012Simons (21),2012Baser (15), oReimbursements, utilization 9standard costsReimbursementsConstella: utilization 9standard costs; Ingenix:chargesUtilization 9 standard costCostingmethod 1 claim with primary or secondaryDx of ICD-9 CM 714.0Dx of ICD-9-CM 714.xxNoNo 1 claim with Dx of ICD-9 CM 714.0,714.1, 714.2, or 714.81ComparisongroupNoDefinition of RADiagnosed by rheumatologistMichaud (19),2003Weycker (10),2005Author, yearTable 2. Cost analysis methods*RA Medical Care Costs1435
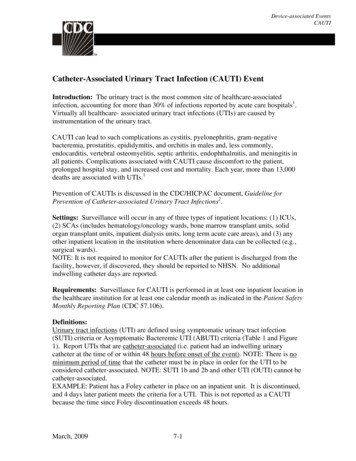
1436Hresko et alTable 3. Reported cost of care by study (in 2015 dollars)*Study type, author (ref.),yearOverall US populationMichaud (19), 2003Simmons (21), 2012Simmons (21), 2012Simmons (21), 2012Kawatkar (20), 2012Privately insured patientsBirnbaum (12), 2010Birnbaum (14), 2012MedicareHarrold (18), 2012Harrold (18), 2012Harrold (18), 2012Harrold (18), 2012MedicaidKhanna (16), 2007Johnson (17), 2008Birnbaum (12), 2010Biologic DMARD users onlyWeycker (10), 2005†Weycker (10), 2005‡Wu (11), 2007McBride (13), 2011Baser (15), 2015YearsreportedTotalcost, dollarsRA-specificcare, NRNR22,35816,71622,445* RA rheumatoid arthritis; NR not reported.† Constella COMPASS database, utilization 9 standard cost method.‡ Ingenix LabRx database, charges method.(Table 3). Notably, the low estimate of 3,266 (17) is muchlower than any other finding, being only 28% of the nextlowest estimate. Meta-analysis of studies including all RApatients found annual total cost of care to be 12,509 (95%confidence interval [95% CI] 7,451–21,001) (Figure 2A).Removing the low estimate did not substantially changethe total cost of care ( 12,458 [95% CI 7,381–21,025]).Among studies restricted to RA patients using bDMARDs,annual total cost of care ranged from 26,469 to 52,837,with the lower estimate representing privately insuredworking-age adults and the higher estimate privatelyinsured adults ages 65 years. Meta-analysis found annualtotal cost of care among patients using biologics to be 36,053 (95% CI 32,138–40,445) (Figure 2B).Estimates for annual cost for RA-specific care ranged considerably. Estimates in studies including patients using anytreatment regimen (i.e., not limited to bDMARD users only)ranged from 2,437 to 7,849 (Table 3), with the lower estimate representing a population modeling the general USpopulation and the higher representing Medicaid enrollees.Meta-analysis determined annual cost for RA-specific careto be 3,723 (95% CI 2,408–5,762) when accounting forpatients using any treatment regimen (Figure 2C), representing 30% of total costs for all care. Estimates of RA-specificcosts in studies limiting their population to patients usingbDMARDs ranged from 16,716 to 22,445, with both estimates being based on different claims databases comprisingprivately insured working-age adults. Meta-analysis foundannual RA-specific cost within this population to be 20,262 (95% CI 17,480–23,487) (Figure 2D), representing56% of total costs for all care.DISCUSSIONRA is a morbid, mortal, and costly illness. The cost oftreating RA has increased over the last 2 decades with theadvent of bDMARDs, but this increase has not been wellstudied. We conducted a systematic literature review andanalyzed prior cost-of-care studies for RA; the cost of directmedical care for a patient with RA was 12,509 and thecosts attributable to RA were 3,725, or 30% of the totalcosts. Among patients receiving bDMARDs, total directmedical costs were 36,053, and costs attributable to RAwere 20,262, or 56% of the total.These findings suggest that costs associated with RA are inline with those for other prominent chronic diseases. Recentstudies have reported the annual total direct cost of care fordiabetes mellitus patients as 14,732 (22), multiple sclerosispatients as 23,195 (23), ulcerative colitis patients between 4,032 and 13,722 (24), and patients with chronic obstructive pulmonary disease between 1,681 and 10,812 (25),using 2015 dollars. Our findings also suggest that the burdenof RA patients on the US health care system may become outsized compared to the disease’s relatively small prevalenceand compared to patients with these other chronic conditions as more patients use bDMARDs in the future.The observed costs show that patients who usebDMARDs had increased costs compared with typical
RA Medical Care CostsA1437B 12,509 ( 7,451- 21,001)C 36,053 ( 32,138- 40,445)D 3,725 ( 2,408- 5,768) 20,262 ( 17,480- 23,487)Figure 2. Meta-analysis results for the direct medical costs. A, Total cost of care, all patients. B, Total cost of care, biologic diseasemodifying antirheumatic drug users only. C, Rheumatoid arthritis (RA)–specific cost of care, all patients. D, RA-specific cost of care,biologic DMARD users only. Multiple articles included in these meta-analyses reported cost-of-care findings for several distinct patientpopulations. These distinct populations are each treated as individual contributors to the meta-analysis and are listed with the identifying characteristic of the patient population studied (e.g., individual year or specific drug-treatment regimen).RA patients. Additionally, bDMARD use had a largerincremental effect on RA-specific costs (444% increase)than on total direct medical costs (188% increase). However, in both cases the increment was below the totalcost of bDMARDs themselves. This gap suggests thateither the use of bDMARDs may be associated with lowertotal nondrug direct medical costs or that the patientswho receive bDMARDs have fewer comorbid conditions.Research comparing the characteristics of bDMARD usersversus regular DMARD users has shown differences inthe demographic and clinical characteristics of bDMARDusers compared to regular DMARD users (26,27), and thistopic is worthy of further examination.While the cost of RA is extremely important to the healthcare system, the methodologies observed and used acrossthe included prior studies varied substantially. The definition of RA differed, what were considered costs and theircalculation were not standardized, and the attempt to partition RA costs from non-RA costs differed by study. Twopredominant methods were used to identify RA-specificcosts: de-identification of claims with an RA-related ICD-9CM diagnosis code, and determination of the incrementalcosts between a population of RA patients versus a population of controls. Both methods have their limitations. Identification of claims with RA-related codes fails to addressthe possibility that claims may be misclassified as beingRA-related or not, based on a coding error. Likewise, assessment of incremental cost is subject to error in the nuance ofdefining a non-RA control population, especially in theconsideration of which comorbidities may or may not berelated to the pathophysiology of RA. In addition, the quality of reporting in the included studies was inconsistent.The methods for studying direct medical costs need further standardization. Standardized methods would facilitate comparison across studies with less concern forheterogeneity and would also allow for better temporaltrend analyses, ensuring “apples-to-apples” comparisons.Ideal methods would account for all inpatient, outpatient,prescription medication, and post–acute care costs, rely onactual reimbursement amounts reported in claims as thebasis of analysis, define RA patients by requiring multipleinstances of an RA-related diagnosis code in claims, assessboth total cost for all medical care and RA-specific care,and compare costs between RA patients and similarpatients without RA from the same database.The current meta-analysis is limited by the literature weincluded. As noted, the methods across studies were notconsistent, and this limitation increases the uncertainty ofour summarized results. Since we did not have individualpatient-level data, we could not examine the associationsbetween individual patient characteristics and cost. As well,the methods for partitioning RA costs were inconsistent,
1438Hresko et almaking the RA-specific cost analyses more difficult to interpret. Finally, we did not include studies of indirect costs ofRA, such as work lost and caregiver costs. While indirectcosts are substantial (9,28,29), the methodologic variabilityis also significant; thus, we worried about introducing evenmore heterogeneity in this meta-analysis.In light of these limitations, we conclude that the directmedical costs for patients with RA are significant. Clearly,medication costs comprise a substantial portion of thesecosts, especially for patients using bDMARDs. Without considering the health effects, benefits, and risks, the currentanalysis cannot comment on whether specific treatmentsare of value. Cost-effectiveness analyses comparing different treatment strategies for RA are ongoing and will provideuseful information. The studies included in this metaanalysis do not include assessments of RA outcomes, butour findings may be a valuable resource for future costeffectiveness analyses that will further understanding ofthe relative benefits of treatment options available to RApatients. As standards of care evolve in RA, the standardsfor studying the cost of care in RA must also mature andbecome codified. This codification will facilitate bettercomparisons across treatments and across time.AUTHOR CONTRIBUTIONSAll authors were involved in drafting the article or revising itcritically for important intellectual content, and all authorsapproved the final version to be submitted for publication. Dr.Solomon had full access to all of the data in the study and takesresponsibility for the integrity of the data and the accuracy ofthe data analysis.Study conception and design. Hresko, Solomon.Acquisition of data. Hresko, Solomon.Analysis and interpretation of data. Hresko, Lin, Solomon.ADDITIONAL DISCLOSUREDr. Lin is an employee of Amgen.REFERENCES1. Sacks JJ, Luo YH, Helmick CG. Prevalence of specific typesof arthritis and other rheumatic conditions in the ambulatory health care system in the United States, 2001–2005.Arthritis Care Res (Hoboken) 2010;62:460–4.2. Cooper NJ. Economic burden of rheumatoid arthritis.Rheumatology (Oxford) 2000;39:28–33.3. Lubeck DP. A revi
the cost of RA care is more than half of all direct medical costs. INTRODUCTION Rheumatoid arthritis (RA) is a chronic, progressive autoim- . California), Daniel H. Solomon, MD, MPH: Brigham and Women's Hospital, Boston, Massachusetts. Address correspondence to Daniel H. Solomon, MD, MPH, Division of Rheumatology, Brigham and Women's .