Transcription
The LaryngoscopeC 2017 The American Laryngological,VRhinological and Otological Society, Inc.A Paradigm for Evaluation and Management of the Maxillary SinusBefore Dental ImplantationYi-Wei Chen, MD ; Fu-Ying Lee, MD; Po-Hung Chang, MD; Chi-Che Huang, MD;Chia-Hsiang Fu, MD ; Chien-Chia Huang, MD ; Ta-Jen Lee, MDObjectives: To determine a paradigm for evaluating and managing maxillary sinus conditions before dental implantationvia preoperative sinonasal assessment.Study Design: Prospective cohort study.Methods: Eighty-four patients who underwent dental implantation with or without sinus augmentation were included.Maxillary sinus conditions were classified into groups 1 to 6 according to cone-beam computed tomography (CT) findings: 1)nonspecific findings, 2) solitary polyp or cyst, 3) mucosal thickening, 4) air–fluid level or fluid accumulation, 5) near-totalopacification of the maxillary or other paranasal sinus, and 6) calcification spots in the maxillary sinus. Dental implantationwith or without sinus augmentation was suggested with postoperative sinus observation (groups 1–3), after medication foracute sinusitis (group 4), and after comprehensive treatment of chronic or fungal sinusitis (groups 5–6). Intraoperative andpostoperative sinus-related complications were recorded.Results: Two patients (groups 1 and 3) developed acute rhinosinusitis after sinus augmentation; both recoveredcompletely with medical treatment. Schneiderian membrane perforation occurred during sinus lift surgery in six patients(group 1): five recovered after conservative medical therapy and close observation, whereas one required endoscopic sinussurgery and recovered well. No chronic rhinosinusitis developed after dental implantation.Conclusion: Craniofacial CT is crucial for pre-dental implantation sinonasal evaluation. The risk of dental implantrelated chronic rhinosinusitis is low for patients with cysts, polyps, or mucosal thickening in the maxillary sinus. However,preventive endoscopic sinus surgery is recommended for patients with incurable chronic rhinosinusitis, fungal sinusitis, andlarge polyps or cysts.Key Words: Dental implant, maxillary sinusitis, sinus augmentation, cone beam computed tomography.Level of Evidence: 4.Laryngoscope, 00:000–000, 2017INTRODUCTIONDr. Leonard Linkow performed the first moderndental endosseous implant in 1952. However, dentalimplant placement in the maxilla has not been widelyimplemented due to close proximity of the maxillarysinus and complications arising from surgery. The sinuslift technique introduced by Tatum1 and Boyle andJames2 resolved this problem. After introduction of thesinus lift procedure, Tatum described the lateral windowapproach and Summers introduced a new crestalapproach using an osteotome. The search for safer andsimpler sinus elevation procedures is ongoing.From the Department of Otolaryngology (Y-W.C., P-H.C., CHI-C.H., Cthe Department of Periodontics, Division of Dentistry (F-Y.L.), Chang Gung Memorial Hospital, Taipei; the Chang GungUniversity (Y-W.C., F-Y.L., P-H.C., CHI-C.H., C-H.F., CHIEN-C.H., T-J.L.), Taoyuan,Republic of China; and the Xiamen Chang Gung Hospital (T-J.L.), Xiamen, Peoples Republic of ChinaEditor’s Note: This Manuscript was accepted for publication onJuly 21, 2017.The authors have no funding, financial relationships, or conflictsof interest to disclose.Send correspondence to Ta-Jen Lee, MD, Department of Otolaryngology, Chang Gung Memorial Hospital, 5 Fu-Shin Street, Kueishan,Taoyuan, 333, Republic of China. E-mail: yiwei0819@gmail.comH.F., CHIEN-C.H., T-J.L.);DOI: 10.1002/lary.26856Laryngoscope 00: Month 2017Although the lateral window approach and crestalosteotome technique have been shown to be safe andpredictable procedures for increasing alveolar boneheight for appropriate positioning of dental implants inregions close to the maxillary sinus, complications associated with these procedures are not rare. Kim et al.reported that the incidence of sinusitis after sinus liftsurgery was 9.8%, and it was higher with the lateralapproach (12.1%) than with the crestal approach(4.1%).3 In most cases, this can be resolved with antibiotic therapy. Chronic maxillary sinusitis requiring surgical intervention occurs in 1.3% of all patients,4 and oftenleads to medical disputes.According to a review of the literature and the findings of our previous study, the possible causes of chronicmaxillary sinusitis after dental implantation includesinus penetration by the implant,5 formation of anoroantral fistula,6 uncontrolled graft infection,5 dislodged bone grafts or dental implants with a foreignbody reaction,7 perforation of the Schneiderian membrane,8 postoperative obliteration of the ostium,9 andpreoperative chronic rhinosinusitis.4 Endoscopic sinussurgery is the first choice of surgery because of its lowmorbidity and good prognosis.10The risk of rhinosinusitis after dental implant surgery is higher in patients with preoperative chronicChen et al.: Pre-Dental Implantation Sinus Evaluation1
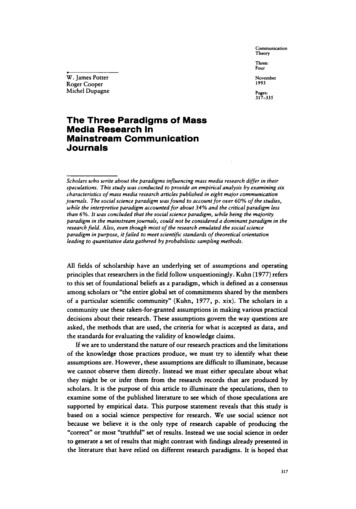
Fig. 1. Cone beam computedtomography findings in the maxillarysinus before dental implantation.(A) Nonspecific finding, (B) solitarypolyp or cyst, (C) mucosal thickening, (D) air–fluid level or fluid accumulation (most often indicatingacute infection or inflammation), (E)near-total opacification of the maxillary sinus or other paranasal sinuses(most often indicating chronic rhinosinusitis), and (F) calcification spotsin the maxillary sinus (most oftenindicating fungal sinusitis).sinusitis, which is a major concern for dentists. Beforeplacing dental implants, dentists usually acquire conebeam computed tomography (CBCT) images or panoramic radiographs to confirm the height of the alveolarbone and to determine the necessity for the sinus liftprocedure. Maxillary sinus lesions in various stages ofseverity often are revealed in imaging findings, andthese patients are first advised to consult ear, nose, andthroat (ENT) specialists. However, there is no specificprotocol for maxillary sinus evaluation and managementbefore dental implant surgery. Therefore, we designedthis prospective clinical study to determine a paradigmfor evaluating and managing maxillary sinus conditionsbefore dental implantation by assessing preoperativesinonasal characteristics using CBCT and determiningtheir association with implant-related rhinosinusitis.MATERIALS AND METHODSThe institutional review board of Chang Gung MemorialHospital (Taoyuan, Republic of China) approved this study, andall the patients provided written informed consent. All patientswho underwent endosseous maxillary implant surgery performed by Dr. F-Y Lee in the Department of Periodontics atChang Gung Memorial Hospital between January 2013 andDecember 2015 were included in this study.When the need for dental implants was determined, adetailed medical and dental history was obtained and thoroughoral examinations were performed for all patients in this dentaldepartment. Craniofacial CBCT also was performed to evaluatethe height of the alveolar bone and determine the necessity forsinus lift procedures. The patients were subsequently referredto the ENT department for further evaluations.In the ENT department, all patients underwent completesinonasal evaluations, including careful history-taking and localLaryngoscope 00: Month 20172examinations. They also were asked to complete the Sino-NasalOutcome Test 22 (SNOT-22). In addition, all patients wereassessed for possible general and specific risk factors for sinonasal diseases after sinus lift or dental implant procedures,including smoking, allergic rhinitis, previous nasal surgery ortrauma, history of chronic and/or recurrent rhinosinusitis, andother systemic diseases that may affect the physiology of thenose or sinuses. Nasal fiberoptic endoscopy was performed toevaluate the condition of the nasal mucosa, septum, turbinate,meatal grooves, and osteomeatal complex.Craniofacial CBCT images were carefully assessed to evaluate the sinonasal condition, including anatomical alterationssuch as septal deviation and concha bullosa; patency of themaxillary sinus ostium; the presence of oroantral fistulae; andthe presence of any sinonasal abnormality, particularly in themaxillary sinus. On the basis of these findings, patients werecategorized into six groups (groups 1–6) (Fig. 1): those with 1)nonspecific findings, 2) a solitary polyp or cyst, 3) mucosalthickening, 4) air–fluid level or fluid accumulation (most oftenindicating acute infection or inflammation), 5) near-total opacification of the maxillary sinus or other paranasal sinuses (mostoften indicating chronic rhinosinusitis), and 6) calcificationspots in the maxillary sinus (most often indicating fungalsinusitis).After these assessments, the ENT risk for each patientwas established. For patients with normal maxillary sinuses(group 1), we considered that the risk of postoperative chronicrhinosinusitis was very low. For patients with small polyps,cysts, or mucosal thickening (groups 2 and 3), we suggestedclose observation after dental implant surgery with or withoutsinus augmentation. These patients were instructed to returnfor follow-up if they experienced any nasal discomfort after surgery. However, if a large cyst or polyp was present (height ofcyst or polyp more than half the height of the maxillary sinus),we discussed the outcomes of preventive surgery with thepatients to aid in deciding on their treatment plan. For patientsChen et al.: Pre-Dental Implantation Sinus Evaluation
TABLE I.Characteristics, Systemic Diseases and SNOT-22 Scores rs40152816816Without systemic disease382260Systemic diseaseAsthma17372245Hypertension527Diabetes mellitusHeart disease320133Hepatitis314GoutThyroid disease200121Ectopic dermatitisSNOT-22 Score (Average)513.35116.83614.55SNOT-22 5 Sino-Nasal Outcome Test 22.with acute rhinosinusitis (group 4), medical therapy was prescribed and follow-up examinations conducted until recovery,following which further implant treatment was planned withDr. F-Y Lee Patients with chronic or fungal sinusitis (groups 5and 6) were informed of a high risk of implant failure and wereadvised not to undergo implant surgery until complete resolution of the sinusitis. Endoscopic sinus surgery was suggestedfor patients with chronic rhinosinusitis to increase the survivalrate of dental implants and decrease the possibility of complications after implant surgery. All the patients followed oursuggestions.The outcomes of sinus lift and dental implant surgerieswere assessed during follow-up visits in the dental departmentwhere the surgeries were performed, and all intraoperative andpostoperative complications were recorded. If patients presentedwith any symptom or sign related to rhinosinusitis, they werereferred to the ENT department for further evaluation andtreatment. Patients who did not present with any signs orsymptoms underwent ENT assessments, including nasal fiberoptic endoscopy, SNOT-22 evaluation, and sinus radiography (ifpanoramic radiography was not available), at 3 months aftersurgery.sinuses, which is a characteristic of chronic rhinosinusitis. Finally, 2.4% patients exhibited few calcificationspots with mucosal thickening in the maxillary sinus,which sometimes were accompanied with scleroticchanges in the sinus wall. These are similar to classicalfindings of fungal sinusitis. The findings from craniofacial CBCT before sinus augmentation are summarized inTable II.Postoperative ComplicationsTwo patients, belonging to groups 1 and 3, respectively, developed acute rhinosinusitis after sinus augmentation, and both recovered completely after medicaltreatment. Schneiderian membrane perforation occurredduring sinus lift surgery in six patients belonging togroup 1, five of whom recovered after conservative medical therapy and close observation. The remaining patientunderwent endoscopic sinus surgery because of diseaseprogression and demonstrated good recovery (Fig. 2). Nocase developed chronic rhinosinusitis after dentalimplantation. One patient, who complained of nasal discomfort after dental implantation, showed normal findings on follow-up sinus computed tomography (CT).DISCUSSIONIn the present study, we determined a paradigm forevaluating and managing maxillary sinus conditionsbefore dental implantation by assessing preoperativesinonasal characteristics using CBCT and determiningtheir association with implant-related rhinosinusitis.Our findings revealed a normal maxillary sinuswithout definite abnormal findings in almost half of thepatients (46.4%); this rate was similar to rates (43.7–53.2%) found in several other studies.11 Such patientscan safely undergo dental implant procedures, withaccompanying explanations regarding possible sinusrelated complications. The most common abnormal CTfindings were solitary cysts or polyps and mucosal thickening, and we suggested implant surgery with closesinus observation to these patients, considering thatmost of them were asymptomatic according to theirSNOT-22 results. Fan et al. reported that all 18 implantsRESULTSIn total, 84 patients were included in this study.The average age of patients was 48.8 years, and the male:female ratio was approximately 2:1. The averageSNOT-22 score was 14.55, which was similar to the scoreof a healthy population. The patient characteristics arelisted in Table I.Preoperative CBCT FindingsPreoperative CBCT findings revealed nonspecificfindings in 46.4% patients. Solitary polyps or cysts wereobserved in 22.6% patients; mucosal thickening in 20.2%patients; and fluid accumulation in the maxillary sinus,which could represent acute infection or inflammation,in 7.2% patients. Only 1.2% patients showed near-totalopacification of the maxillary sinus or other paranasalLaryngoscope 00: Month 2017TABLE II.CT Finding of Maxillary Sinus Before Sinus Augmentation.CT FindingNo. of Patients (%)Group 1: Nonspecific findingGroup 2: Solitary polyp or cyst39 (46.4%)19 (22.6%)Group 3: Mucosal thickening17 (20.2%)Group 4: Air–fluid level or fluidaccumulation6 (7.2%)Group 5: Nearly total opacificationof maxillary or other sinusGroup 6: Calcification spots inmaxillary sinus1 (1.2%)Total2 (2.4%)84 (100%)CT 5 computed tomography.Chen et al.: Pre-Dental Implantation Sinus Evaluation3
Fig. 2. A representative case ofSchneiderian membrane perforationduring sinus augmentation, withgraft material leakage into the sinus.(A) Cone-beam computed tomography findings before sinus augmentation. There was no specific findingin the maxillary sinus. (B) Schneiderian membrane perforation wasnoted during sinus augmentation.Some graft materials leaked into themaxillary sinus. (C) Image taken 2weeks after the leakage observed in(B). Left maxillary sinusitis with sinusmucosal thickening had developed.(D) Endoscopic findings during surgery. Graft materials were notedwithin the maxillary sinus. (E) Threemonths after surgery. The maxillarysinus shows complete recovery. (F)Eighteen months after surgery. Dental implantation was performed, withgood prognosis. [Color figure canbe viewed in the online issue, whichis available at www.laryngoscope.com.]placed in 16 patients with sinus membrane thickening ofmore than 2 mm were successful.12 Similar results wereobserved in the present study, with no case of postoperative chronic rhinosinusitis or implant failure.Air–fluid level or fluid collection in the maxillarysinus, which mostly represents acute rhinosinusitis, wasnoted on preoperative CBCT scans in approximately7.2% of patients in the present study. This condition easily is cured by medication. The only concern is chronicrhinosinusitis that fails to respond to medical treatment,particularly fungal sinusitis. In most cases of fungalsinusitis in the present study, the disease was in theearly stage, with mild symptoms. Preoperative CBCTonly showed mucosal thickening, with few calcificationspots (Fig. 3). Careful evaluation of preoperative CTscans is essential to rule out chronic rhinosinusitis, particularly fungal sinusitis, to prevent possible implantfailure in the future.In the present study, two patients with a normalsinus or mild mucosal thickening on preoperative CBCTand endoscopy developed acute sinusitis after sinus augmentation. These patients showed complete recoveryafter 2 weeks of antibiotic therapy. We believe that theacute sinusitis in these patients was not associated withthe preoperative severity of mucosal thickening, butrather with the recovery capacity of the maxillarysinus.13 The incidence of postoperative acute sinusitis inthe present study was lower than 5%, similar to that ina previous study.14 Sinusitis without chronic changescan be cured by medical treatment alone.The membrane perforation rate in patients treatedwith sinus augmentation is reported to be between 9%and 44%.15,16 Most studies did not consider smallLaryngoscope 00: Month 20174perforations be of major concern.4,17–19 If the perforationexceeds 5 mm, repair is required to prevent the laterincidence of sinusitis and to increase the survival of dental implants.17,20 In the present study, six patients developed obvious Schneiderian membrane perforation duringsinus augmentation. The image in Figure 2 showsmarked leakage. We observed a normal sinus conditionFig. 3. A representative case of fungal sinusitis in the early stagesbefore sinus augmentationPreoperative cone beam computed tomography only showsmucosal thickening with a few calcification spots (arrow). A fungalball with pus is noted in the maxillary sinus during surgery (upperright). [Color figure can be viewed in the online issue, which isavailable at www.laryngoscope.com.]Chen et al.: Pre-Dental Implantation Sinus Evaluation
Fig. 4. Paradigm for evaluation andmanagement of maxillary sinus conditions before dental implantationwith or without sinus augmentation.CT 5 computed tomography; F/u 5follow-up.before sinus augmentation, with a series of changes inthe sinus mucosa after leakage. The patient underwentendoscopic sinus surgery and received dental implants,and was in good condition thereafter. Because the otherfive patients exhibited less leakage, we treated themwith medical therapy only, which led to complete recovery. These findings give rise to an important question:should patients with graft material leakage from sinusmembrane perforation receive aggressive or conservativetherapy? We suggest that if the maxillary sinus ostiumLaryngoscope 00: Month 2017is patent on CT or endoscopy, observation followed byconservative therapy will be beneficial because themovements of the sinus membrane cilia may transfermost leaked material to the nasal cavity, from where itwill be eliminated. Surgery only should be consideredwhen conservative therapy fails.The requirement of preventive functional endoscopic sinus surgery remains controversial. Torrettaet al. suggested that patients with presumably reversibleENT contraindications to sinus floor elevation, such asChen et al.: Pre-Dental Implantation Sinus Evaluation5
chronic sinusitis, endo-antral foreign bodies, and nosedeformity, should resolve these issues before dentalimplant surgery to prevent sinusitis resulting from sinusaugmentation and implant procedures.13 According toour experience, surgery should be performed in patientswith incurable chronic sinusitis; large maxillary sinuscysts or polyps; and suspected fungal sinusitis beforedental implantation. Patients with mucosal thickening,polyps, or nasal septal deviation should be kept underfurther observation. According to our previous study,cysts or polyps with a height exceeding half the heightof the maxillary sinus should be treated before dentalimplant surgery.10 The reasoning for this is that theaverage height of the maxillary sinus is 33 mm and theostium of the maxillary sinus will not be obstructed withan additional height of 10 mm, which usually is necessary for sinus augmentation21,22 as long as the height ofthe thickened mucosa or polyp is less than one-half thatof the maxillary sinus. We applied this protocol in ourstudy and encountered no case of chronic rhinosinusitisafter dental implant surgery.Figure 4 shows the final paradigm based on theresults of our study. If the findings of preoperative CTare normal, we can consider that the incidence of postoperative chronic rhinosinusitis will be very low and decideon treatment accordingly. After treatment, the patientsshould be closely monitored. If fluid collection, whichmostly represents acute sinusitis, is observed, patientscan receive medical treatment and follow-up evaluations.If there is mucosal thickening or a small polyp or cyst inthe maxillary sinus, patients should be monitored. If alarge cyst or polyp is present, the outcomes of preventivesurgery should be explained to the patient to aid in making a decision regarding their treatment. Finally, if thereis opacification of the sinus, which mostly representschronic sinusitis; or calcification spots and/or scleroticchanges in the sinus wall, which mostly represent fungalsinusitis, patients should be advised to undergo functional endoscopic sinus surgery to increase the survivalrate of dental implants and to decrease the possibility ofpostimplantation complications.In terms of the choice of treatment for patientswith dental implant-related chronic rhinosinusitis, endoscopic sinus surgery should be the first choice of surgerybecause of the good prognosis and low morbidity.10 Over60% patients with dental implant-related chronic rhinosinusitis with preserved dental implants did not exhibitrecurrence. Therefore, we believe that dental implantscan be preserved unless they are mobile or severelyinfected, or if the patient develops recurrent sinusitis.However, the sinus mucosa above the dental implantsmust be kept intact during endoscopic sinus surgery.10The role of the otolaryngologist should not only belimited to the treatment of complications, such as rhinosinusitis, after dental implantation but also shouldinclude evaluation and preventative steps before theimplantation. Pignataro et al. also suggested that an otolaryngologist should be a primary figure in the approachto any sinus lift procedure, which should comprise threesteps to ensure success of the surgery: a preventativediagnostic step, a preventative therapeutic step, and aLaryngoscope 00: Month 20176diagnostic therapeutic step.23 Our evaluation paradigmled to zero incidence of chronic rhinosinusitis after dental implantation, thus providing a good medicolegalassurance for both patients and dentists.CONCLUSIONWe determined a paradigm for evaluating the maxillary sinus before dental implant surgery with or withoutsinus augmentation. Our findings suggest that craniofacialCT before dental implantation is crucial not only to determine the height of the alveolar bone and the necessity ofsinus lift procedures but also to evaluate the sinonasalcondition. Relative to that in a healthy population, the riskof dental implant-related chronic rhinosinusitis is not highin patients with cysts, polyps, or mucosal thickening in themaxillary sinus; these patients can undergo dental implantsurgery and sinus augmentation with close postoperativemonitoring of the sinus. Preventative endoscopic sinus surgery before dental implantation only should be suggestedto patients with incurable chronic rhinosinusitis, fungalsinusitis, and large polyps or cysts.BIBLIOGRAPHY1. Tatum H Jr. Maxillary and sinus implant reconstructions. Dent Clin NorthAm 1986;30:207–229.2. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 1980;38:613–616.3. Kim YK, Hwang JY, Yun PY. Relationship between prognosis of dentalimplants and maxillary sinusitis associated with the sinus elevation procedure. Int J Oral Maxillofac Implants 2013;28:178–183.4. Manor Y, Mardinger O, Bietlitum I, et al. Late signs and symptoms ofmaxillary sinusitis after sinus augmentation. Oral Surg Oral Med OralPathol Oral Radiol Endod 2010;110:e1–e4.5. Zimbler MS, Lebowitz RA, Glickman R, Brecht LE, Jacobs JB. Antral augmentation, osseointegration, and sinusitis: the otolaryngologist’s perspective. Am J Rhinol 1998;12:311–316.6. Lopatin AS, Sysolyatin SP, Sysolyatin PG, Melnikov MN. Chronic maxillary sinusitis of dental origin: is external surgical approach mandatory?Laryngoscope 2002;112:1056–1059.7. Kim JW, Lee CH, Kwon TK, Kim DK. Endoscopic removal of a dentalimplant through a middle meatal antrostomy. Br J Oral MaxillofacSurg 2007;45:408–409.8. Timmenga NM, Raghoebar GM, van Weissenbruch R, Vissink A. Maxillarysinusitis after augmentation of the maxillary sinus floor: a report of 2cases. J Oral Maxillofac Surg 2001;59:200–204.9. Hunter WL IV, Bradrick JP, Houser SM, Patel JB, Sawady J. Maxillarysinusitis resulting from ostium plugging by dislodged bone graft: casereport. J Oral Maxillofac Surg 2009;67:1495–1498.10. Chen YW, Huang CC, Chang PH, et al. The characteristics and new treatment paradigm of dental implant-related chronic rhinosinusitis. Am JRhinol Allergy 2013;27:237–244.11. Vogiatzi T, Kloukos D, Scarfe WC, Bornstein MM. Incidence of anatomicalvariations and disease of the maxillary sinuses as identified by conebeam computed tomography: a systemic review. Int J Oral MaxillofacImplants 2014;29:1301–1314.12. Fan QQ, Chen L, Xu S, Han XP, Liu ZH. The changes of maxillary sinusmembrane thickness after maxillary sinus floor elevation surgery. ChinJ Stomatol 2015;50:531–535.13. Torretta S, Mantovani M, Testori T, Cappadona M, Pignataro L. Importance of ENT assessment in stratifying candidates for sinus floor elevation: a prospective clinical study. Clin Oral Impl Res 2013;24:57–62.14. Kayabasoglu G, Nacar A, Altundag A, Cayonu M, Muhtarogullari M,Cingi C. A retrospective analysis of the relationship between rhinosinusitis and sinus lift dental implantation. Head Face Med 2014;10:53.15. Cho-Lee GY, Naval-Gias L, Castrejon-Castrejon S, et al. A 12-year retrospective analytic study of the implant survival rate in 177 consecutivemaxillary sinus augmentation procedures. Int J Oral MaxillofacImplants 2010;25:1019–1027.16. Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol 2004;75:511–516.17. Becker ST, Terheyden H, Steinriede A, Behrens E, Springer I, Wiltfang J.Prospective observation of 41 perforations of the Schneiderian membrane during sinus floor elevation. Clin Oral Impl Res 2008;19:1285–1289.Chen et al.: Pre-Dental Implantation Sinus Evaluation
18. Timmenga NM, Raghoebar GM, Boering G, van Weissenbruch R. Maxillary sinus function after sinus lifts for the insertion of dental implants.J Oral Maxillofac Surg 1997;55:936–939.19. Moreno Vazquez JC, Gonzalez de Rivera AS, Gil HS, Mifsut RS. Complication rate in 200 consecutive sinus lift procedures: guidelines for prevention and treatment. J Oral Maxillofac Surg 2014;72:892–901.20. Anavi Y, Allon DM, Avishai G, Calderon S. Complications of maxillarysinus augmentations in a selective series of patients. Oral Surg OralMed Oral Pathol Oral Radiol Endod 2008;106:34–38.Laryngoscope 00: Month 201721. Karmody CS, Carter B, Vincent ME. Developmental anomalies of the maxillary sinus. Trans Sect Otolaryngol Am Acad Opthalmol Otolaryngol1977;84:ORL-723–728.22. Misch CE. Maxillary sinus augmentation for endosteal implants:organized alternative treatment plans. J Oral Implantol 1987;4:49–58.23. Pignataro L, Mantovani M, Torretta S, Felisati G, Sambataro G. ENTassessment in the integrated management of candidate for (maxillary)sinus lift. Acta Otorhinolaryngol Ital 2008;28:110–119.Chen et al.: Pre-Dental Implantation Sinus Evaluation7
implant placement in the maxilla has not been widely implemented due to close proximity of the maxillary sinus and complications arising from surgery. The sinus lift technique introduced by Tatum1 and Boyle and James2 resolved this problem. After introduction of the sinus lift procedure, Tatum described the lateral window