Transcription
Partnership 2017January QuarterlyMeetingJanuary 24, 2017Dial in: 1-800-369-3308Participant passcode: 3636845 2017 ECRI INSTITUTEAgenda: January 24, 2017I.II.III.IV.V.VI.WelcomePatient Identification Safe PracticesPartnership News2017 workgroupsDiscussionPresentations from Collaborating Organizations: CHIME,AHIMA, and NIST1
A Big Thank You to the Patient ID WorkgroupThanking the Patient Identification Workgroup Hardeep Singh, MD, MPH, Workgroup Chair, Michael E. DeBakeyVeterans Affairs Medical CenterJason Adelman, MD, MS, Chief Patient Safety Officer &Associate Chief Quality Officer, New York-PresbyterianHospital/Columbia University Medical CenterGraham Atkinson, DPhil, Vice President for Research and Policy,Jayne Koskinas Ted Giovanis Foundation for Health and PolicyLinda G. Brady, CAE, Chief Executive Officer, Association forHealthcare Documentation Integrity (AHDI)Samantha Chao, MPH, Pew Charitable TrustsGerry Castro, PhD, MPH, Project Director, Patient SafetyInitiatives, Joint Commission on Accreditation of HealthcareAllen Chen, MD, PhD, MHS, Associate Professor Oncology,Associate Professor Pediatrics, Armstrong Institute for PatientSafety and Quality, The Johns Hopkins HospitalHarry Corey, McKesson CorporationBrian Crawford, EpicJustin Cross, MD, Medical Informatics Fellow, Office of theNational Coordinator for Health ITSharon Fiveash, Baptist Memorial Health Care PSOTrisha Flanagan, RN, MSN, Senior Manager, Patient Safety,athenahealthDebbie Fox, McKesson CorporationAngela Franklin, JD, Senior Officer, Drugs and Medical Devices,The Pew Charitable Trusts Terhilda Garrido, MPH, VP Health Information TechnologyTransformation & Analytics, Kaiser PermanenteAndrew Gettinger, MD, Chief Medical Information Officer, Office ofthe National Coordinator for Health IT, Office of Programs &Engagement, Office of Clinical Quality & SafetyTed Giovanis, FHFMA, MBA, President, Jayne Koskinas Ted GiovanisFoundationLynn Thomas Gordon, MBA, RHIA, CAE, FACHE, FAHIMA , ChiefExecutive Officer, American Health Information ManagementAssociation (AHIMA)Helen Haskell, Mothers Against Medical ErrorsWilliam Isenberg, MD, PhD, Vice President Patient Safety, SutterHealthCaroline Jonker, Executive Director, McKesson CorporationLesley Kadlec, American Health Information ManagementAssociation (AHIMA)Leslie Kringstein, Interim Vice President of Public Policy of Collegeof Healthcare Information Management Executives (CHIME)Nana Kunlertkit, The Johns Hopkins HospitalPamela Lane, American Health Information ManagementAssociation (AHIMA)Christoph U. Lehman, MD, FAAP, FACMI, Professor, Pediatrics andBiomedical Informatics, Monroe Carell Jr. Children’s Hospital atVanderbilt University Medical CenterSusan Lucci, RHIA, CHPS, CHDS, Consultant/Chief Privacy Officer,Just Associates, Inc.2
Thanking the Patient Identification Workgroup Trish Lugtu, CPHIMS, ConstellationJohn D. McGreevey III, MD, FACP, Assistant Professor of ClinicalMedicine, Associate CMIO, University of Pennsylvania Health SystemLettie Murr, McKesson CorporationMary Beth Navarra-Sirio, RN, MBA, Vice President RegulatoryStrategy, McKessonLori A. Paine, RN, MS, DrPH(c), Director, Patient Safety, The JohnsHopkins Hospital and Armstrong Institute for Patient Safety andQuality, Johns Hopkins MedicineSusan Paparella, RN, MSN, Vice President, Institute for SafeMedication Practices (ISMP)Kalyan Pasupathy, PhD, Mayo Clinic, Center for the Science of HealthCareLauren Riplinger, American Health Information ManagementAssociation (AHIMA)Josh Rising, MD, MPH, Director, The Pew Charitable TrustsJim Russell, RPh, EpicJeanie Scott, MS, CPHIMS, Director, Informatics Patient Safety,Veterans Health AdministrationMark Segal, PhD, Vice President, Government and Industry Affairs, GEHealthcare ITDebora Simmons, PhD, RN, CCNS, FAAN, The University of TexasHealth Science Center at Houston, School of Biomedical InformaticsJeff Smith, AMIAMaria Stolz-Epple, The Johns Hopkins HospitalAllen J. Vaida, PharmD, FASHP, Executive Vice President, Institute forSafe Medication PracticesDiana Warner, MS, RHIA, CHPS, FAHIMA, Director, HIM PracticeExcellence, American Health Information Management Association Diane L. Watson, MA BSN RN-BC, Manager Clinical InformationSystems, St Louis Children’s HospitalAdam Wiseman, Regulatory Analyst, AllscriptsFeliciano “Pele” Yu, Jr., MD, MSHI, MSPH, FHIMSS, ChiefMedical Information Officer, St. Louis Children’s Hospital;Medical Director, Washington University Pediatric ComputingFacility; Associate Professor, Department of Pediatrics,Washington University School of MedicineECRI Institute staff: Ronni Solomon, JD, Executive Vice President and GeneralCounsel William Marella, MBA, MMI, Executive Director, PSO Operationsand Analytics, Ellen Deutsch, MD, MS, FAAP, FACS, CPPS, Medical Director Robert Giannini, NHA, CHTS-IM/CP, Patient Safety Analyst andConsultant Amy Goldberg-Alberts, MBA, FASHRM, CPHRM ExecutiveDirector, Partnership Solutions Patient Safety, Risk, and Quality Jeremy J. Michel, MD, MHS, Health Technology Assessment,ECRI-Penn AHRQ Evidence Based Practice Center (EPC) Lorraine Possanza, DPM, JD, MBE, FACFOAM, FAPWCA, SeniorPatient Safety, Risk, and Quality Analyst Amy Tsou, MD, MSc, Senior Research Analyst, HealthTechnology Assessment, ECRI-Penn AHRQ Evidence BasedPractice Center (EPC) Stephanie Uses, PharmD, MJ, JD, Patient Safety Analyst Cindy Wallace, CPHRM, Senior Risk Management AnalystSafe Practices for the Use of Health IT inPatient Identification--Attributes (I) Electronic fields containing patientidentification data should consistently usestandard identifier conventions. (D) Use a confirmation process to help matchthe patient and the documentation. (E) Use standard attributes and attributeformats in all transactions to improvematching. (N) Use a standard display of patientattributes across the various systems.3
Safe Practices for the Use of Health IT inPatient Identification--Technology (T) Include distinguishing informationenhancing identification on screens, printouts,and those areas that require interventions. (I) Integrate new technologies to facilitate andenhance identification. (F) Implement monitoring systems to readilydetect identification errors. (Y) Include high-specificity active alerts andnotifications to facilitate proper identification.Safe Practices for Patient ID CommunicationPlan: Who, What, When, Where, and How WHO we want to reach: Healthcare organizations and providers, leaders, managers, andclinical users Vendors Physician practices—hospital affiliated and non-hospital affiliated Patient Safety Organizations Professional societies/associations Policymakers Patient/consumer representatives Others4
Safe Practices for Patient ID CommunicationPlan: WHAT is the message we want to convey? Importance of the safe use of technology for patient identification Recommendations are informed by the evidence Recommendations were formulated using a multi-stakeholderprocess Toolkit resources will help with implementation of the patientidentification safe practices Implementation is the key to successSafe Practices for Patient ID CommunicationPlan: WHEN, WHERE and HOW to disseminate the message Press releases Social media Webinars Newsletters and trade association magazines Policy meetings Vendors’ and collaborating organizations’ member/customermeetings and communication materials Website postingsECRI will provide communication tools and assistance andthe materials will be available on a public website5
Partnership NewsPolling Question: HIMSS17 Will you will be at HIMSS17? Yes, I am planning on attending HIMSS17 No Unsure6
News Of Interest for the Partnership 21st Century Cures Act December 13, 2016 Health IT developers treated as providers for PSO purposesRecent publications Applied Clinical Informatics article, Safe Practices for Copy and Paste in the EHR: Systematic Review, Recommendations, and Novel Model forHealth IT Collaboration, ISTIR 8166-Examing the Copy and Paste Function in the Use of HealthRecords DOI: https://doi.org/10.6028/NIST.IR.8166Upcoming publications Partnership Proceedings—in-person meeting Partnership Patient ID Safe Practices toolkitPartnership 2017 Workgroups and ProjectsDeveloping and MaintainingClosing the Loopa HIT Safety Program2017WorkgroupsDiagnostic TestsNIST UsabilityImplementationProject PlanningReferralsVendors and ProvidersAmbulatory CareAcute CareOthers7
Polling Question: Workgroup Participation Are you interested in participating in a workgroup? Yes, the developing and maintaining a HIT safety program group Yes, the closing the loop group Yes, the implementation project Yes, more than one workgroup Not at this timeWorkgroup Participation—If you Missed thePolling Question E-mail hit@ecri.org indicating your choice of workgroup Note your interest in your participation or in working onimplementation of safe practices8
Open the Phone Lines forDiscussion Comments on workgroup topicsData GatheringIdentification of HIT’s ContributionImplementation ModelsPartnership Discussion: In Preparation for aHIT Safety Program Workgroup How do you know if health IT has caused or contributedto adverse event or near misses in your organization?What are the other important pieces in the picture?9
Polling Question: Adverse Events, Hazards andHIT Do you have a process to identify if HIT contributed to anadverse event or a hazard? Yes, we have identified a method to figure this out Yes, but it is case by case NoPartnership Discussion: Tackling ImplementationWhat tools are most useful in facilitating implementationof the safe practices? How do we best tackle implementation of safe practicerecommendations? development of "use cases" determination of what organizations to conducttesting monitoring progress and/or issues that arise 10
Polling Question: Implementation Would you be interested in participating in implementingsafe practice recommendations? Yes, Partnership’s copy and paste recommendations Yes, Partnership’s patient identification recommendations Yes, SAFER guides Not at this timeParticipant Discussion: Gathering Data toDerive Information Are there other ways to extract data from the EHR thatwould provide additional insights into safety? Presently collected information Information collected in the background Are there other sources of information that thePartnership should be evaluating?11
Polling Question: Data Gathering Do you presently identify and collect safety informationdirectly from your EHR? Yes, we have identified and routinely collect Yes, we are in the process of identifying NoUpdates from Collaborating Organizations12
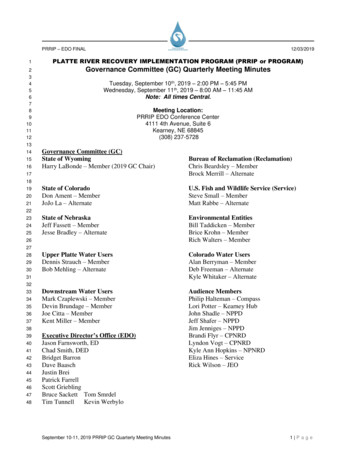
Partnership for Health IT Patient Safety UpdateJanuary 24, 2017Barb SivekVP, Business ServicesCHIMEChallenge Status 371 registered competitors Submission deadline – March 1, 2017 44 Use case scenarios and performance results Submission questions (6) – Enrollment & Identification, Security & FraudManagement, Privacy, Scalability, Adoptability, Implementation Images and video of Enrollment and Identification Statement on intellectual property rights Prototype development plan Supplemental information13
Challenge Timeline 3/1 – Final submissions due 3/10 - Judges receive submissions (3-week review cycle) 3/30 – Finalists determined, and notified to submit prototypes 4/30– Prototype submission deadline 5/1 - 5/30 – Prototype testing phase 6/1 – Finalist demonstration for Judges 6/14 – Winner announcedStakeholder InputHow can the Partnership for Health IT Patient Safety help?What characteristics/functions/elements should a patient ID solution contain tomake it successful from a Health IT safety perspective?14
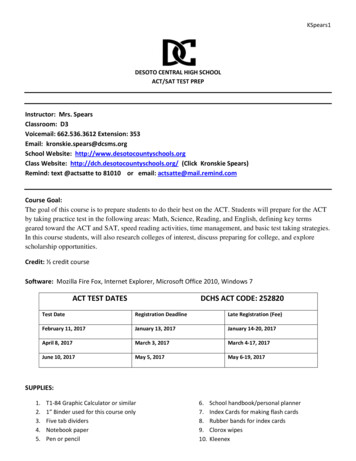
ECRI: Partnership for Health IT Patient SafetyWebinar, January 24, 2017AHIMA Use Case:Patient RegistrationAHIMA Standards Task Force PresentationReporter: Diana Warner, AHIMADirector, StandardsDiana.warner@ahima.org 2017AHIMA Task Force MembersNameKathleen AddisonLinda Bailey-WoodsKevin BaldwinSally BikosChristine CainSusan ClarkAlane CombsGreg DavisVicki DelgadoCarlyn DoyleOkmena EwoteraiCathly FliteRobert GianniniElisa GortonDarice GrzybowskiPhoebe HaglundRegina HarrisonAaron HaskettDeShawna Hill-BurnsBeth HornSandra HuyckSatyendra KaithRobin KeeneyTracy Matarazzo JacobsTheresa JonesPamela LailSharon LewisKatherine LuskSusan LucciJennifer ManahanMarcia MatthiasTabitha McDanielAffiliationAlberta Health ServicesPlante MoranUCLASt. Catherine HospitalValley West Community HospitaleHealthcare ConsultingCoastal HealthcareNorth Mississippi Medical CenterKindred Hospital AlbuquerqueMultnomah Department County of AssetsMontefiore Medical CenterTemple UniversityECRISt. Vincent's Medical CenterH.I. Mentors, LLCIntermountain HealthcareDepartment of Veteran AffairsData & Coding Compliance ConsultantAdvocate Trinity HospitalChapa-De Indian Health ServicesBeaumont Health SystemKaplan Higher Education GroupVHC, IncNIH/CC/MRdResurrection UniversityNovant HealthCalifornia Health Information AssociationChildren’s Medical SystemJust AssociatesVia Christi ClinicSouthern Illinois HealthcareMcKesson 201715
AHIMA Task Force MembersNameSharon MeyerNicole MillerMichelle MitcheffTami MontroyShamara MurryRobert NallMemory NdangaNeysa NoreenSandra NunnBonnie OrmondTerri PhillipsLarissa SteinMick TalleyChristine TaylorJennifer TealLori McNeil TolleySharon MeyerMegan MunnsNeysa NoreenSandra NunnBill ReisbickDeane StillarChristine TaylorDeAnn TuckerChristine WattsTraci WaughValerie WilsonLee WiseDonna YoungAffiliationMinistry HealthMiller And Miller AssociatesPowell Valley HealthcareDrexel UniversityBethany MethodistVeteran’s AdministrationRutgers UniversityChildren's Hospitals and Clinics of MinnesotaKAM ConsultingCarteret General HospitalHSHS St. Anthony’s Memorial HospitalUniversity of Colorado HealthUniversity-BankUniversity of Washington MedicineDepartment of Veteran AffairsBoston Children's HospitalMinistry Health CareJust AssociatesChildren's Hospitals and Clinics of MinnesotaKAMC ConsultingPacific Rim Medical Risk, LLCAlberta Health ServicesUniversity of Washington MedicineOwensboro HealthThe University of Chicago MedicineNorth Valley HospitalHCA Information Technology & Services, Inc.Summit Medical CenterMemorial Hospital of CarbondaleDr. Anna OrlovaHarry RhodesDiana WarnerAHIMA StaffSenior Director, StandardsDirector, National StandardsDirector, Standards 2017ProblemPatient Registration content is not standardized acrossorganizations and information systems vendors today.Getting Patient Registration right means: Information is correct, complete and timely Demographic entries are cross-validated throughout alldocumentation Documentation is complete Patient matching is enabled Documentation on the right patient is available to the rightclinician (MD or RN) at the right time of the careIn 2016 AHIMA developed Patient Registration Use Case that serves thebasis for Patient Registration Content Profile standard to bedeveloped by AHIMA at the Integrating the Healthcare Enterprise (IHE) 201716
AHIMA Patient Registration Use CaseScope:AHIMA Patient Registration Use Case identified 17 scenariosfor patient registration across the 3 types of settings1. Emergency department visit2. In-patient setting visit (hospitals, clinics and other)3. Out-patient setting visitFocus in 2016: Emergency department visit setting 2017AHIMA Patient Registration Use CaseScope: Emergency department visit settingAHIMA Patient Registration Use Case identified 17 scenariosfor patient registration across the 3 types of settings1. Emergency department visit scenarios: Registration of walk-in/patient presentation in ED Registration initiated/conducted by clinicians2. In-patient setting visit (hospitals, clinics and other)3. Out-patient setting visit 201717
AHIMA Patient Registration Use Case:Actors, Workflow and Data Flow 2017AHIMA Patient Registration Use Case:Information Collected– Patient Registration Information Patient, Visit, Physician Demographics Reason for visit Consents (visit, information sharing)– Insurance information– Payment informationCollectedbyBusinessActor– Notification of Record Availability– Acknowledgement of Receipt– Audit Record: Who, When, Why, WhatCollectedbyTechnicalActor 201718
AHIMA Patient Registration Use Case:Sample Content to be StandardizedPatient/Guardian demographics Name DoB AddressVisit demographics Enterprise MRN Date/Time of encounter Reason for visitCare Team demographics NameRolePIDDeparment/serviceInsurance information Type of PayorInsurance IDCoverageCo-pay 2017AHIMA Patient Registration Use Case:Standards Needed– IHE PIX/PDQ - Patient Identity CrossReferencing/Patient Demographic Query– IHE XDW - Cross Document Workflow– HL7 Version 2.x Patient Administration– HL7 C-CDA - Consolidated Clinical DocumentArchitecture– HL7 FHIR - Fast Healthcare Interoperability Resources– X12 Administrative Transactions– Others, such as SNOMED, LOINC, etc 201719
AHIMA - IHE Patient RegistrationContent Profile New IHE content profile with core sections thatdescribe data elements and associated CDAformats for standardized patient registrationacross EHRs and other infotmation systems component observation classCode "OBS"moodCode "EVN" templateIdroot "2.16.840.1.113883.10.20.1.31"/ id root "8b3fa370-67a5-11dbbd13-0800200c9a66"/ code code "33765-9"codeSystem "2.16.840.1.113883.6.1"displayName "WBC"/ statusCode code "completed"/ effectiveTimevalue "200003231430"/ value xsi:type "PQ" value "6.7"unit "10 3/ul"/ 2017NISTExamining Copy and PasteFunction in the Use ofElectronic Health Records20
Examining the ‘Copy and Paste’ Function in the Use ofElectronic Health RecordsLana LowryNIST HIT Usability Leadllowry@nist.govHuman Factors RecommendationsHuman Factors Recommendations to support The Partnership Recommendation AProvide a mechanism to make copy and paste material easily EHR systems must be designed to enhance the visibility of the information beingselected for copy and paste to prevent users from inadvertently copying only part ofidentifiablethe information that was intended to be pasted which could minimize the possibilityof incomplete reuse of information that could lead to morbid/mortal errors.Areas where copy and paste should be locked The ‘copy and paste’ function should absolutely not be allowed when entering anyinformation into a blood bank information system due to the extreme risk involvedin blood transfusion. Copy of demographic information should never be allowed, but needs to beautopopulated in all the interfaces within a patient’s chart. Dates should absolutely never be copied and pasted.21
Human Factors RecommendationsHuman Factors Recommendation to support The Partnership Recommendation BEnsure that the provenance of copy and paste User interface has to display the “chain of custody” of theinformation associated with the use of copy and paste.material is readily availableHowever, this information should not be displayed bydefault, and only be shown on user demand to avoid thepossibility of overwhelming clinical users and contribute toerrors of commission (taking an incorrect action). A concept for reconciling that the copied information wasread consciously and edited by the clinical provider wouldpromote the attribution of the source of the information.Human Factors RecommendationsAdditional Human Factors Recommendations for critical areas identified in the studyVital signs The following properties are recommended when documenting vital signs throughcharting done by the clinical user or by real time feed to the EHR system from digitaldevices: Time stamp when measured. How it was measured (nurse manually takes BP, arterial linecaptures BP at a single time) Time stamp when documented in the EHR. Time stamp when it is signed (locked). Time stamp when it is revised. Time stamp when retrieved.Allergies There should be clear “chain of custody” when copying and pasting information related toSurgical notesThe design of the EHR must ensure that all of the information pertaining to surgical notes isallergies.provided with the ‘copy and paste’ functionality which helps the reuse of information by theclinical staff in the “exact” and precise context of the surgical notes. Variability may exist dueto patient-specific findings and/or specific situations that might arise unexpectedly during theprocedure which must be accommodated by EHRs by means of provisions for efficient editing.22
Human Factors RecommendationsAdditional Human Factors Recommendations for critical areas identified in the studyMedication entryWhen medication entry is done in free text form, the ‘copy and paste’ function could be thesuperior method of entry as compared to typing. Copying and pasting a medication with thedosing is much safer compared to the use of a drop down menu since there are known errorsrelated to wrong selections and jumping menus in the use of drop down menus. The ‘copy andpaste’ function should always be associated with a clear “chain of custody”. As a general rule, theuse of copy and paste should be discouraged in new orders to reinforce the fact of conscious dataentry.Discharge summaryWhen used during patient discharge, the copy and paste of reused information should reflect the“chain of custody” for the clinical provider indicating that it is indeed copied from a past event.Copying and pasting information from differentWhen copying and pasting information into an EHR from a different patient’s chart is allowed, thedepartments and another patient’s EHREHR system must keep the clinician oriented as to which patient’s record they are accessing at anygiven point in the process. There should be a clear “chain of custody” indicating the exact sourceof the copied and pasted information while protecting the privacy and confidentiality of the sourcepatient. Enable user to easily transition from the current chart with unrestricted access to inputinformation to another chart by a deliberate action (i.e., identification / activation of the patientchart), by the user.NISTIR 8166: Examining the ‘Copy and Paste’ Function in the Use of ElectronicHealth RecordsLink: 166.pdf23
Next Steps and RemindersRemindersWatch for upcoming publications E-mail hit@ecri.org with your workgroup preference or yourorganization’s interest in implementing safe practices Keep alert for upcoming workgroup schedules See you at HIMSS17 Partnership Meeting- Tuesday, February 21, 2:30 PM Room W234 Journey to Patient Safety: Where We’ve Been and How Health IT Can Help Wednesday, February 22, 2017 — 11:30AM EST - 12:30PM ESTOrange County Convention CenterW320, Chapin TheaterSession ID: 18024
Partnership Expert Advisory Panel David W. Bates, MD, MSc, Brigham and Women’s HospitalKathleen Blake, MD, MPH, American Medical AssociationPascale Carayon, PhD, University of Wisconsin-Madison College of EngineeringTejal Gandhi, MD, MPH, National Patient Safety FoundationChris Lehmann, MD, Vanderbilt University Medical CenterPeter J. Pronovost, MD, PhD, The Johns Hopkins University School of MedicineJeanie Scott, MS,VHA Office of Informatics and Analytics/Health InformaticsPatricia P. Sengstack, DNP, RN-BC, CPHIMS, Bon Secours Health System, Inc.Hardeep Singh, MD, MPH, Michael E. DeBakey VA Medical Center and BaylorCollege of MedicineDean Sittig, PhD, The University of Texas Health Science Center at Houston,School of Biomedical InformaticsPaul Tang, MD, MS, IBM Watson HealthWorking Together: 2017 EC RI I N S TI TU TE25
Questions? Contact hit@ecri.org26
1 2017 ECRI INSTITUTE Partnership 2017 January Quarterly Meeting January 24, 2017 Dial in: 1-800-369-3308 Participant passcode: 3636845 Agenda: January 24, 2017