Transcription
The PPO PlanSchedule of BenefitsFaculty, Staff, and Technical ServicePrepared exclusively for:Employer:Contract number:The Pennsylvania State University285717Contract effective date:Plan effective date:Plan issue date:January 1, 2020January 1, 2020October 4, 2018These benefits are not insured with Aetna but will be paid from the Employer's funds.Aetna will provide certain administrative services under the Aetna medical benefitsplan.1Proprietary
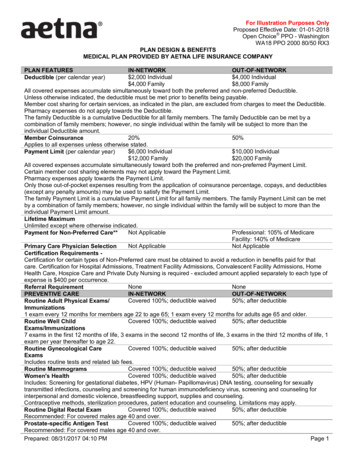
Schedule of benefitsThis schedule of benefits lists the deductibles and copayments/payment percentage, if any that apply to theservices you receive under this plan. You should review this schedule to become familiar with your deductiblesand copayments/payment percentage and any limits that apply to the services.How to read your schedule of benefits----When we say:- “In-network coverage”, we mean you get care from a network provider.- “Out-of-network coverage”, we mean you can get care from providers who are not network providers.The deductibles and copayments/payment percentage listed in the schedule of benefits below reflect thedeductibles and copayment/payment percentage amounts under your plan.Any payment percentage listed in the schedule of benefits reflects the plan payment percentage. This isthe amount the Plan pays. You are responsible to pay any deductibles, copayments, and the remainingpayment percentage.You are responsible for full payment of any health care services you receive that are not a covered benefit.This plan has maximums for specific covered benefits. For example, these could be visit, day or dollarmaximums. They are combined maximums between network providers and out-of-network providersunless we state otherwise.At the end of this schedule you will find detailed explanations about your:- Deductible- Maximum coinsurance out-of-pocket limits- Overall Maximum out-of-pocket limitsImportant note:All covered benefits are subject to the Calendar Year deductible and copayment/payment percentage unlessotherwise noted in the schedule of benefits below.We are here to answer any questions. Contact Member Services by logging onto your Aetna Navigator securemember website at www.aetna.com or at the toll-free number on your ID card.This schedule of benefits replaces any schedule of benefits previously in effect under your plan of benefits.Keep this schedule of benefits with your booklet.2Proprietary
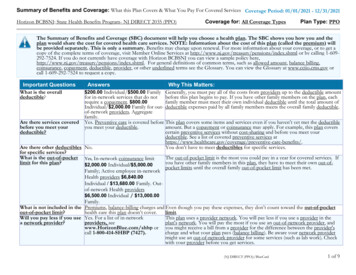
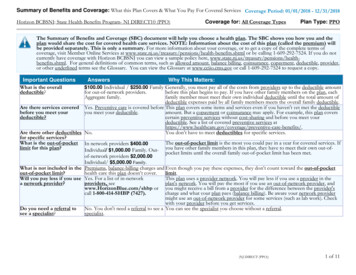
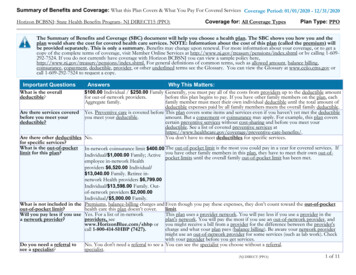
The PPO PlanFaculty and Staff Salary Band 1 – Under 45,000Schedule of BenefitsPrepared exclusively for:Employer:Contract number:Control number:Contract effective date:Plan effective date:Plan issue date:The Pennsylvania State University285717285717Schedule of Benefits 1AJanuary 1, 2018January 1, 2018December 21, 2017These benefits are not insured with Aetna but will be paid from the Employer's funds.Aetna will provide certain administrative services under the Aetna medical benefitsplan.Plan featuresDeductible/MaximumsIn-network coverage*Out-of-network coverage*DeductibleYou have to meet your Calendar Year deductible before this plan pays for benefits.Individual 250 per Calendar Year 500 per Calendar YearFamily 500 per Calendar Year 1,000 per Calendar YearDeductible waiverThe Calendar Year in-network deductible is waived for all of the following eligible health services: Preventive care and wellness Family planning services - female contraceptivesMaximum out-of-pocket limitsMaximum Coinsurance out-of-pocket limit per Calendar Year.Individual 1,250 per Calendar Year 2,500 per Calendar YearFamily 5,000 per Calendar Year 2,500 per Calendar YearOverall Maximum out-of-pocket limit per Calendar Year (including deductibles, copayments andcoinsurance).Individual 7,150 per Calendar YearNot ApplicableFamily 14,300 per Calendar YearNot Applicable*See How to read your schedule of benefits at the beginning of this schedule of benefits3Proprietary
The PPO PlanFaculty and Staff Salary Band 2 - 45,001 - 60,000Schedule of BenefitsPrepared exclusively for:Employer:Contract number:Control number:Contract effective date:Plan effective date:Plan issue date:The Pennsylvania State University285717285717Schedule of Benefits 1BJanuary 1, 2018January 1, 2018December 21, 2017These benefits are not insured with Aetna but will be paid from the Employer's funds.Aetna will provide certain administrative services under the Aetna medical benefitsplan.Plan featuresDeductible/MaximumsIn-network coverage*Out-of-network coverage*DeductibleYou have to meet your Calendar Year deductible before this plan pays for benefits.Individual 375 per Calendar Year 750 per Calendar YearFamily 750 per Calendar Year 1,500 per Calendar YearDeductible waiverThe Calendar Year in-network deductible is waived for all of the following eligible health services: Preventive care and wellness Family planning services - female contraceptivesMaximum out-of-pocket limitsMaximum Coinsurance out-of-pocket limit per Calendar Year.Individual 1,250 per Calendar Year 2,500 per Calendar YearFamily 5,000 per Calendar Year 2,500 per Calendar YearOverall Maximum out-of-pocket limit per Calendar Year (including deductibles, copayments andcoinsurance).Individual 7,150 per Calendar YearNot ApplicableFamily 14,300 per Calendar YearNot Applicable*See How to read your schedule of benefits at the beginning of this schedule of benefits4Proprietary
The PPO PlanFaculty and Staff Salary Band 3 – 60,001 - 90,000Schedule of BenefitsPrepared exclusively for:Employer:Contract number:Control number:Contract effective date:Plan effective date:Plan issue date:The Pennsylvania State University285717285717Schedule of Benefits 1CJanuary 1, 2018January 1, 2018December 21, 2017These benefits are not insured with Aetna but will be paid from the Employer's funds.Aetna will provide certain administrative services under the Aetna medical benefitsplan.Plan featuresDeductible/MaximumsIn-network coverage*Out-of-network coverage*DeductibleYou have to meet your Calendar Year deductible before this plan pays for benefits.Individual 500 per Calendar Year 1,000 per Calendar YearFamily 1,000 per Calendar Year 2,000 per Calendar YearDeductible waiverThe Calendar Year in-network deductible is waived for all of the following eligible health services: Preventive care and wellness Family planning services - female contraceptivesMaximum out-of-pocket limitsMaximum Coinsurance out-of-pocket limit per Calendar Year.Individual 1,250 per Calendar Year 2,500 per Calendar YearFamily 5,000 per Calendar Year 2,500 per Calendar YearOverall Maximum out-of-pocket limit per Calendar Year (including deductibles, copayments andcoinsurance).Individual 7,150 per Calendar YearNot ApplicableFamily 14,300 per Calendar YearNot Applicable*See How to read your schedule of benefits at the beginning of this schedule of benefits5Proprietary
The PPO PlanFaculty and Staff Salary Band 4 – 90,000 and overSchedule of BenefitsPrepared exclusively for:Employer:Contract number:Control number:Contract effective date:Plan effective date:Plan issue date:The Pennsylvania State University285717285717Schedule of Benefits 1DJanuary 1, 2018January 1, 2018December 21, 2017These benefits are not insured with Aetna but will be paid from the Employer's funds.Aetna will provide certain administrative services under the Aetna medical benefitsplan.Plan featuresDeductible/MaximumsIn-network coverage*Out-of-network coverage*DeductibleYou have to meet your Calendar Year deductible before this plan pays for benefits.Individual 625 per Calendar Year 1,250 per Calendar YearFamily 1,250 per Calendar Year 2,500 per Calendar YearDeductible waiverThe Calendar Year in-network deductible is waived for all of the following eligible health services: Preventive care and wellness Family planning services - female contraceptivesMaximum out-of-pocket limitsMaximum Coinsurance out-of-pocket limit per Calendar Year.Individual 1,250 per Calendar Year 2,500 per Calendar YearFamily 5,000 per Calendar Year 2,500 per Calendar YearOverall Maximum out-of-pocket limit per Calendar Year (including deductibles, copayments andcoinsurance).Individual 7,150 per Calendar YearNot ApplicableFamily 14,300 per Calendar YearNot Applicable*See How to read your schedule of benefits at the beginning of this schedule of benefits6Proprietary
The PPO PlanTechnical ServiceSchedule of BenefitsPrepared exclusively for:Employer:Contract number:Control number:Contract effective date:Plan effective date:Plan issue date:The Pennsylvania State University285717285737Schedule of Benefits 1AJanuary 1, 2018January 1, 2018December 21, 2017These benefits are not insured with Aetna but will be paid from the Employer's funds.Aetna will provide certain administrative services under the Aetna medical benefitsplan.Plan featuresDeductible/MaximumsIn-network coverage*Out-of-network coverage*DeductibleYou have to meet your Calendar Year deductible before this plan pays for benefits.Individual 250 per Calendar Year 500 per Calendar YearFamily 500 per Calendar Year 1,000 per Calendar YearDeductible waiverThe Calendar Year in-network deductible is waived for all of the following eligible health services: Preventive care and wellness Family planning services - female contraceptivesMaximum out-of-pocket limitsMaximum Coinsurance out-of-pocket limit per Calendar Year.Individual 1,000 per Calendar Year 2,000 per Calendar YearFamily 4,000 per Calendar Year 2,000 per Calendar YearOverall Maximum out-of-pocket limit per Calendar Year (including deductibles, copayments andcoinsurance).Individual 7,150 per Calendar YearNot ApplicableFamily 14,300 per Calendar YearNot Applicable*See How to read your schedule of benefits at the beginning of this schedule of benefits7Proprietary
The PPO PlanPre-65 Retiree PPO PlanSchedule of BenefitsPrepared exclusively for:Employer:Contract number:Control number:Contract effective date:Plan effective date:Plan issue date:The Pennsylvania State University285717285717Schedule of Benefits 1EJanuary 1, 2018January 1, 2018December 21, 2017These benefits are not insured with Aetna but will be paid from the Employer's funds.Aetna will provide certain administrative services under the Aetna medical benefitsplan.Plan featuresDeductible/MaximumsIn-network coverage*Out-of-network coverage*DeductibleYou have to meet your Calendar Year deductible before this plan pays for benefits.Individual 375 per Calendar Year 750 per Calendar YearFamily 750 per Calendar Year 1,500 per Calendar YearDeductible waiverThe Calendar Year in-network deductible is waived for all of the following eligible health services: Preventive care and wellness Family planning services - female contraceptivesMaximum out-of-pocket limitsMaximum Coinsurance out-of-pocket limit per Calendar Year.Individual 1,250 per Calendar Year 2,500 per Calendar YearFamily 5,000 per Calendar Year 2,500 per Calendar YearOverall Maximum out-of-pocket limit per Calendar Year (including deductibles, copayments andcoinsurance).Individual 7,150 per Calendar YearNot ApplicableFamily 14,300 per Calendar YearNot Applicable*See How to read your schedule of benefits at the beginning of this schedule of benefits8Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Preventive care and wellnessRoutine physical examsPerformed at aphysician’s, PCP officeCovered personsthrough age 21:Covered persons age 22and over but less than65: Maximum visits perCalendar YearCovered persons age 65and over: Maximumvisits per Calendar Year100% per visit70% (of the recognized charge) per visitNo deductible appliesSubject to any age and visit limitsprovided for in the comprehensiveguidelines supported by the AmericanAcademy of Pediatrics/BrightFutures/Health Resources and ServicesAdministration guidelines for childrenand adolescents.Subject to any age and visit limitsprovided for in the comprehensiveguidelines supported by the AmericanAcademy of Pediatrics/BrightFutures/Health Resources and ServicesAdministration guidelines for childrenand adolescents.For details, contact your physician orMember Services by logging onto yourAetna Navigator secure memberwebsite at www.aetna.com or callingthe number on your ID card.1 visitFor details, contact your physician orMember Services by logging onto yourAetna Navigator secure memberwebsite at www.aetna.com or callingthe number on your ID card.1 visit1 visit1 visitPreventive care immunizationsPerformed in a facility orat a physician’s office100% per visit70% (of the recognized charge) per visitNo deductible appliesSubject to any age limits provided for inthe comprehensive guidelinessupported by Advisory Committee onImmunization Practices of the Centersfor Disease Control and Prevention.Subject to any age limits provided for inthe comprehensive guidelinessupported by Advisory Committee onImmunization Practices of the Centersfor Disease Control and Prevention.For details, contact your physician orMember Services by logging onto yourAetna Navigator secure memberwebsite at www.aetna.com or callingthe number on your ID card.For details, contact your physician orMember Services by logging onto yourAetna Navigator secure memberwebsite at www.aetna.com or callingthe number on your ID card.*See How to read your schedule of benefits at the beginning of this schedule of benefits9Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Well woman preventive visitsroutine gynecological exams (including pap smears)Performed at aphysician’s, PCP,obstetrician (OB),gynecologist (GYN) orOB/GYN officeMaximumsMaximum visits perCalendar Year100% per visit70% (of the recognized charge) per visitNo deductible appliesNo deductible appliesSubject to any age limits provided for inthe comprehensive guidelinessupported by the Health Resources andServices Administration.1 visitSubject to any age limits provided for inthe comprehensive guidelinessupported by the Health Resources andServices Administration.1 visitPreventive screening and counseling servicesOffice visits Obesity and/orhealthy dietcounseling Misuse of alcoholand/or drugs Use of tobaccoproducts Sexually transmittedinfection counseling Genetic riskcounseling for breastand ovarian cancer100% per visit70% (of the recognized charge) per visitNo deductible appliesObesity and/or healthy diet counseling maximums:Maximum visits per 12months26 visits (however, of these, only 1026 visits (however, of these, only 10visits will be allowed under the plan for visits will be allowed under the plan forhealthy diet counseling provided inhealthy diet counseling provided in(This maximum appliesconnection with Hyperlipidemia (highconnection with Hyperlipidemia (highonly to covered persons cholesterol) and other known riskcholesterol) and other known riskage 22 and older.)factors for cardiovascular and dietfactors for cardiovascular and dietrelated chronic disease)*related chronic disease)**Note: In figuring the maximum visits, each session of up to 60 minutes is equal to one visit.Misuse of alcohol and/or drugs maximums:Maximum visits per 125 visits*5 visits*months*Note: In figuring the maximum visits, each session of up to 60 minutes is equal to one visit.*See How to read your schedule of benefits at the beginning of this schedule of benefits10Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Use of tobacco products maximums:Maximum visits per 128 visits*8 visits*months*Note: In figuring the maximum visits, each session of up to 60 minutes is equal to one visit.Sexually transmitted infection counseling maximums:Maximum visits per 122 visits*2 visits*months*Note: In figuring the maximum visits, each session of up to 30 minutes is equal to one visit.Genetic risk counseling for breast and ovarian cancer maximums:Genetic risk counselingfor breast and ovariancancerNot subject to any age or frequencylimitationsNot subject to any age or frequencylimitationsRoutine cancer screenings(applies whether performed at a physician’s, PCP, specialist office or facility)Routine cancerscreeningsMaximums100% per visit70% (of the recognized charge) per visitNo deductible appliesSubject to any age, family history, andfrequency guidelines as set forth in themost current: Evidence-based items that have ineffect a rating of A or B in the currentrecommendations of the UnitedStates Preventive Services TaskForce; and The comprehensive guidelinessupported by the Health Resourcesand Services Administration.Subject to any age, family history, andfrequency guidelines as set forth in themost current: Evidence-based items that have ineffect a rating of A or B in the currentrecommendations of the UnitedStates Preventive Services TaskForce; and The comprehensive guidelinessupported by the Health Resourcesand Services Administration.For details, contact your physician orMember Services by logging onto yourAetna Navigator secure memberwebsite at www.aetna.com or callingthe number on your ID card.1 screening every 12 months*For details, contact your physician orMember Services by logging onto yourAetna Navigator secure memberwebsite at www.aetna.com or callingthe number on your ID card.1 screening every 12 months*Lung cancer screeningmaximums*Important note:Any lung cancer screenings that exceed the lung cancer screening maximum above are covered under theOutpatient diagnostic testing section.*See How to read your schedule of benefits at the beginning of this schedule of benefits11Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Prenatal care services (provided by an obstetrician (OB), gynecologist (GYN), and/orOB/GYN)Preventive care servicesonly100% per visit70% (of the recognized charge) per visitNo deductible appliesNo deductible appliesImportant note:You should review the Maternity and related newborn care sections. They will give you more information oncoverage levels for maternity care under this plan.Comprehensive lactation support and counseling servicesLactation counseling100% per visit70% (of the recognized charge) per visitservices – facility oroffice visitsNo deductible appliesLactation counseling6 visits*6 visits*services maximum visitsper 12 months either ina group or individualsetting*Important note:Any visits that exceed the lactation counseling services maximum are covered under physician services officevisits.Breast feeding durable medical equipmentBreast pump suppliesand accessories100% per item70% (of the recognized charge) peritemNo deductible appliesImportant note:See the Breast feeding durable medical equipment section of the booklet for limitations on breast pump andsupplies.Family planning services – female contraceptivesCounseling servicesFemale contraceptivecounseling servicesoffice visitContraceptivecounseling servicesmaximum visits per 12months either in a groupor individual setting*Important note:100% per visit70% (of the recognized charge) per visitNo deductible applies2 visits*2 visits**See How to read your schedule of benefits at the beginning of this schedule of benefits12Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Any visits that exceed the contraceptive counseling services maximum are covered under physician servicesoffice visits.DevicesFemale contraceptivedevice provided,administered, orremoved, by a physicianduring an office visit100% per item70% (of the recognized charge) peritemNo deductible appliesFemale voluntary sterilizationInpatient100% per admissionOutpatientNo deductible applies100% per visit70% (of the recognized charge) peradmission70% (of the recognized charge) per visitNo deductible appliesPhysicians and other health professionalsPhysicians and specialists office visits (non-surgical)Physician servicesTechnical Service Office visits (nonsurgical) non preventivecareFaculty and Staff Office visits (nonsurgical) non preventivecare 10 then the plan pays 100% (of thebalance of the negotiated charge) pervisit thereafterNo deductible applies 20 then the plan pays 100% (of thebalance of the negotiated charge) pervisit thereafter70% (of the recognized charge) per visit70% (of the recognized charge) per visitNo deductible appliesComplex imagingservices, lab work andradiological servicesperformed during aphysician’s office visit90% (of the negotiatedcharge) per visit after deductible70% (of the recognized charge) per visitafter deductibleAllergy injections*See How to read your schedule of benefits at the beginning of this schedule of benefits13Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Performed at aphysician’s or specialistoffice when you do notsee the physician90% (of the negotiated charge) per visitafter deductible70% (of the recognized charge) per visitafter deductible*See How to read your schedule of benefits at the beginning of this schedule of benefits14Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Allergy testing, treatment and injectionsPerformed at aphysician’s, PCP orspecialist office90% (of the negotiated charge) per visitafter deductible70% (of the recognized charge) per visitafter deductibleImmunizations that are not considered Preventive CareImmunizations that arenot consideredPreventive CareCovered according to the type ofbenefit and the place where the serviceis received.Covered according to the type ofbenefit and the place where the serviceis received.Specialist office visitsTechnical Service Office visits (nonsurgical) 20 then the plan pays 100% (of thebalance of the negotiated charge) pervisit thereafterFaculty and Staff Office visits (nonsurgical)No deductible applies 30 then the plan pays 100% (of thebalance of the negotiated charge) pervisit thereafter70% (of the recognized charge) per visit70% (of the recognized charge) per visitNo deductible appliesComplex imagingservices, lab work andradiological servicesperformed during aspecialist office visit90% (of the negotiated charge) per visitafter deductible70% (of the recognized charge) per visitafter deductiblePhysician surgical servicesPhysicians and specialists office visitsPerformed at a90% (of the negotiated charge) per visitphysician’s, PCP officeafter deductiblePerformed at a90% (of the negotiated charge) per visitspecialist’s officeafter deductible70% (of the recognized charge) per visitafter deductible70% (of the recognized charge) per visitafter deductible*See How to read your schedule of benefits at the beginning of this schedule of benefits15Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Alternatives to physician office visitsWalk-in clinic visitsPreventive Care ServicesImmunizations100% per visit70% (of the recognized charge) per visitNo deductible appliesSubject to any age limits provided for inthe comprehensive guidelinessupported by Advisory Committee onImmunization Practices of the Centersfor Disease Control and Prevention.Subject to any age limits provided for inthe comprehensive guidelinessupported by Advisory Committee onImmunization Practices of the Centersfor Disease Control and Prevention.For details, contact your physician orMember Services by logging onto yourAetna Navigator secure memberwebsite at www.aetna.com or callingthe number on your ID card.For details, contact your physician orMember Services by logging onto yourAetna Navigator secure memberwebsite at www.aetna.com or callingthe number on your ID card.All non-preventive care services for which cost sharing is not shown aboveTechnical Service All other servicesFaculty and Staff All other services 20 then the plan pays 100% (of thebalance of the negotiated charge) pervisit thereafterNo deductible applies 30 then the plan pays 100% (of thebalance of the negotiated charge) pervisit thereafter70% (of the recognized charge) per visit70% (of the recognized charge) per visitNo deductible appliesHospital and other facility careHospital careInpatient hospital90% (of the negotiated charge) peradmission after deductible70% (of the recognized charge) peradmission after deductibleAlternatives to hospital staysOutpatient surgery and physician surgical services90% (of the negotiated charge) per visitafter deductible70% (of the recognized charge) per visitafter deductibleHome health care*See How to read your schedule of benefits at the beginning of this schedule of benefits16Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Outpatient90% (of the negotiated charge) per visitafter deductible12070% (of the recognized charge) per visitafter deductible12090% (of the negotiated charge) peradmission after deductibleUnlimited70% (of the recognized charge) peradmission after deductibleUnlimited90% (of the negotiated charge) per visitafter deductible70% (of the recognized charge) per visitafter deductibleMaximum visits perCalendar YearHospice careInpatient facilityMaximum days perlifetimeHospice careOutpatientOutpatient private duty nursingOutpatient private dutynursingMaximum visits/shiftsper Calendar Year90% (of the negotiated charge) per visitafter deductible70 shifts70% (of the recognized charge) per visitafter deductible70 shiftsUp to eight hours equal one shiftUp to eight hours equal one shiftSkilled nursing facilityInpatient facilityMaximum days perCalendar Year90% (of the negotiated charge) peradmission after deductible10070% (of the recognized charge) peradmission after deductible100 100 then the plan pays 100% (of thebalance of the negotiated charge) pervisit –Waive if admittedPaid the same as in-network coverageEmergency servicesHospital emergencyroomNo deductible appliesNon-emergency care ina hospital emergencyroomNot coveredNot covered*See How to read your schedule of benefits at the beginning of this schedule of benefits17Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Important Note: As out-of-network providers do not have a contract with us the provider may not accept payment ofyour cost share, (deductible, copayment and payment percentage), as payment in full. You mayreceive a bill for the difference between the amount billed by the provider and the amount paid bythis plan. If the provider bills you for an amount above your cost share, you are not responsible forpaying that amount. You should send the bill to the address listed on the back of your ID card, and wewill resolve any payment dispute with the provider over that amount. Make sure the member's IDnumber is on the bill. A separate hospital emergency room copayment/payment percentage will apply for each visit to anemergency room. If you are admitted to a hospital as an inpatient right after a visit to an emergencyroom, your emergency room copayment/payment percentage will be waived and your inpatientcopayment/payment percentage will apply.Urgent careTechnical Service Urgent medical care (ata non-hospital freestanding facility)Faculty and Staff Urgent medical care (ata non-hospital freestanding facility) 20 then the plan pays 100% (of thebalance of the negotiated chargethereafter)No deductible applies 30 then the plan pays 100% (of thebalance of the negotiated chargethereafter)70% (of the recognized charge) per visit70% (of the recognized charge) per visitNo deductible appliesNon-urgent use ofurgent care provider (ata non-hospital freestanding facility)Not coveredNot coveredA separate urgent care copayment/payment percentage will apply for each visit to an urgent care provider.Autism spectrum disorderAutism spectrumdisorder treatmentApplied behavioranalysisCovered according to the type ofbenefit.Covered according to the type ofbenefit and the place where theservice is received.Covered according to the type of benefit.Covered according to the type of benefitand the place where the service isreceived.All other coverage for diagnosis and treatment, including behavioral therapy, will continue to be provided thesame as any other illness under this plan.Birthing centerInpatient90% (of the negotiated charge) peradmission after deductible70% (of the recognized charge) peradmission after deductible*See How to read your schedule of benefits at the beginning of this schedule of benefits18Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Diabetic equipment, supplies and educationDiabetic equipment,supplies and educationCovered according to the type ofbenefit and the place where the serviceis received. See Diabetic SupplyGuidelines for full coverage details.Covered according to the type ofbenefit and the place where the serviceis received. See Diabetic SupplyGuidelines for full coverage details.*See How to read your schedule of benefits at the beginning of this schedule of benefits19Proprietary
Eligible healthservicesIn-network coverage*Out-of-network coverage*Family planning services - otherVoluntary sterilization for malesOutpatient90% (of the negotiated charge) per visitafter deductible70% (of the recognized charge) per visitafter deductibleMaternity and related newborn careInpatient90% (of the negotiated charge) peradmission after deductible70% (of the recognized charge) peradmission after deductibleDelivery services and postpartum care servicesPerformed in a facility orat a physician's office90% (of the negotiated charge) per visitafter deductible70% (of the recognized charge) per visitafter deductibleOther prenatal careservicesCovered according to the type ofbenefit and the place where the serviceis received.Covered according to the type ofbenefit and the place where the serviceis received.Mental health treatment - inpatientInpatient mental healthtreatment90% (of the negotiated charge) peradmission after deductible70% (of the recognized charge) peradmission after deductibleMental health treatment - outpatientTechnical Service Outpatient mentalhealth treatment visitsto a physician orbehavioral healthprovider 10 then the plan pays 100% (of thebalance of the negotiated charge) pervisit thereafterFaculty and Staff Outpatient mentalhealth treatment visitsto a physician orbehavioral hea
Employer: The Pennsylvania State University Contract number: 285717 Control number: 285717 Schedule of Benefits 1C Contract effective date: January 1, 2018 Plan effective date: January 1, 2018 Plan issue date: December 21, 2017 These benefits are not insured with Aetna but will be paid from the Employer's funds.