Transcription
Office of Internal AuditRevenue Cycle – Denials ManagementAuditInternal Audit Report 18:04February 23, 2018
Table of ContentsI. Executive Summary 3Background/Scope and ObjectivesConclusionII. Detailed Observations and Action Plans Matrix Professional Denials Management ObservationsHospital Denials Management ObservationsIII. Appendices 3510101622Appendix A – Risk Classifications and DefinitionsAppendix B – Denial Trending18:04 Revenue Cycle – Denials Management Audit2223Page 2 of 25
Executive SummaryBackgroundRevenue Cycle Operations Process MapDenials management is the process of collecting, tracking,reporting, trending, forecasting, measuring, and managing claimsdenied for payment by insurance payers. An effective denialsmanagement program enables healthcare providers to bettermanage revenue loss; one of their most expensive business risks.Key benefits of an effective program include: identification ofprinciple reasons for revenue loss; efficient processes for denialstracking and appeal; reduced denial volumes; improved cashcollections; improved patient satisfaction; and increasedcommunication and collaboration among internal departments.Denials are typically divided into two categories, technical andclinical, as follows: Technical denials may result from factors such as claimsubmission errors, untimely claim filing, lack of patient eligibilityfor insurance coverage as of the date of service, and unilateraldecisions by the payor.Clinical denials result from payer plan coverage factor includingmedical necessity, patient type, length of stay, specificprocedure, and diagnosis-procedure mismatch issues.The Revenue Cycle Operations team, hospital leadership andclinical department leadership all have responsibilities for thedenials management program at UT Southwestern Medical Center(Medical Center). The denials management activities are dividedinto two groups – hospital and professional.The Revenue Cycle Operations chart above includes, ashighlighted, the steps reviewed during this audit.18:04 Revenue Cycle – Denials Management AuditPage 3 of 25
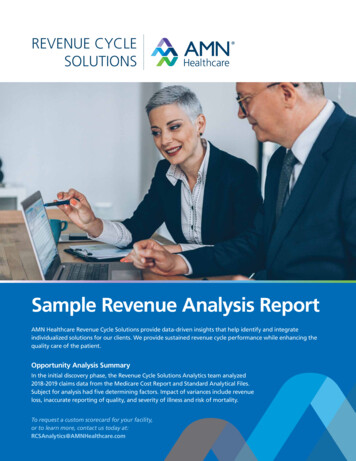
Executive SummaryProfessional Denials ManagementFor departments whose revenue cycle functions are within the centralized Revenue Cycle Operations, clinical denials are managed centrallyby the Revenue Cycle Operations team reporting to the Associate Vice President of Revenue Cycle Operations. Eight clinical departments,are responsible for performing revenue cycle functions within their departments and report to their respective department chairs. Duringcalendar year 2017, professional denials numbered approximately 454,000 (1% of total claims) totaling 80M, which were analyzed andremediated by 115 employees (centralized resources only and does not include decentralized department resources with responsibilities formanaging denials). All professional technical denials are centralized and managed by Revenue Cycle Operations.Hospital Denials ManagementHospital technical denials are managed by the Revenue Cycle Operations team and hospital clinical denials are managed by the DecisionSupport team, which is a hospital department. During calendar year 2017, the hospital denials management teams received approximately94,000 denials (17% of total claims) totaling 900M, which were analyzed and remediated by 50 employees.This graph provides trending information aspercentage of revenue for both hospital andprofessional denial rates during the audit period.Appendix B provides additional information ondenial trending.18:04 Revenue Cycle – Denials Management AuditPage 4 of 25
Executive SummaryScope and ObjectivesThe Office of Internal Audit has completed its Revenue Cycle – Denials Management audit. This is a risk based audit and part of the fiscalyear 2018 Audit Plan.The audit scope period included claim denial activities from January 2017 to December 2017. The review included determining theadequacy and effectiveness of process, oversight, and monitoring controls in place to ensure: Communication of performance metrics and dashboard reports to responsible process owners, Denied claims routed to work queues are resolved and resubmitted in a timely manner, Established denial management strategies and process to identify root causes for improvement, Follow up with clinical and hospital providers to educate and minimize recurrence; and Role-based system access and segregation of duties in processing approved claim adjustments, resubmission and write-off.Audit procedures included interviews with stakeholders, review of policies and procedures and other documentation, substantive testing,and data analytics.We conducted our examination according to guidelines set forth by the Institute of Internal Auditors’ International Standards for theProfessional Practice of Internal Auditing.ConclusionOverall, processes are in place to manage denials throughout the Medical Center, however opportunities exist to improve performance,ensuring denials are analyzed and remediated in a timely manner to reduce the risk of loss of collections. Additional escalation steps areneeded to ensure decentralized departments are held accountable for timely denials management processing. Many of the action plansdeveloped from the previous audit performed in 2014 related to data integrity and reporting were noted during this audit as being in place andfunctioning.Revenue Cycle Operations leadership is developing a project plan to streamline the denials management process so the resources workingdenials transactions in work queues can focus their efforts on denials that can be analyzed and resubmitted to payors to improve MedicalCenter collections rather than efforts on denials categorized as informational only and will not result in additional collections to the MedicalCenter.18:04 Revenue Cycle – Denials Management AuditPage 5 of 25
Executive SummaryIncluded in the table below is a summary of the observations noted, along with the respective disposition of these observations within theMedical Center internal audit risk definition and classification process. See Appendix A for Risk Rating Classifications and Definitions.Priority (0)High (1)Medium (2)Low (0)Total (3)The key improvement opportunities risk-ranked as High and Medium are summarized below.Professional Denials ManagementOpportunities exist for improved monitoring procedures to be in place to ensure timely analysis and resolution for denials transactionsin active work queues. In addition, employee refresher training is needed to ensure employees understand expectations for timelyanalysis, documentation requirements and timely resolution of denial accounts. Additional escalation steps are needed to ensuredecentralized departments are held accountable for timely denials management processing. Evaluation and updating of Epic workqueue change management procedures is needed to prevent accounts from being placed into inactive work queues and thereby notbeing addressed, increasing the risk of loss of collections.#1 Improve Timeliness of Review for Denial Work Queues - Accounts in denial work queues are not consistently cleared in an timely manner, resulting in delays in resubmitting claims to payers which increased the risk of loss of revenue.#2 Improve Work Queue Change Management Procedures - Incomplete Epic change management procedures resulted in then erroneous reactivation of four work queues that had been previously deactivated and caused confusion for the Revenue Cycle Operationsteam and inefficiencies in routing denied charges.#3 Update Security Access to the Hospital Billing System - Revenue Cycle Operations personnel working professional denialsn have greater than minimum necessary access to the Epic Hospital Billing system when read only access is necessary.18:04 Revenue Cycle – Denials Management AuditPage 6 of 25
Executive SummaryPriority (0)High (1)Medium (2)Low (0)Total (3)Hospital Denials ManagementSimilar to professional denials, opportunities exist for monitoring procedures to be in place to ensure timely analysis and resolution ofall denials in active work queues. Timeliness of review for denial accounts should be improved by updating monitoring procedures toidentify accounts that remain in work queues without analysis and providing refresher training to employees to ensure they understandexpectations for timely analysis. Additional escalation steps are needed to ensure hospital clinical departments are held accountablefor timely denials management processing. In addition, defining responsibility for reviewing claims in the pre-billing hold category willensure claims are resubmitted for billing in a timely manner.#4 Improve Timeliness of Review for Denial Work Queues – Accounts in denial work queues are not consistently cleared in an timely manner, resulting in delays in resubmitting claims to payers which increases the risk of loss of revenue.#5 Improve Claim Processing Monitoring for the Denial Account Watch List - Denied accounts accumulating in the Denialn Account Watch List are not consistently monitored resulting in denied claims not timely addressed.#6 Update Epic Security Access for Hospital Clinical Denials Team - The Hospital clinical denials team has greater thann minimum necessary access to the Epic Professional Billing system when only read access is necessary.Management has plans to address the issues identified in the report and in some cases have already implemented corrective actions. Theseresponses, along with additional details for the key improvement opportunities listed above are listed in the Detailed Observations and ActionPlans Matrix (Matrix) section of this report.18:04 Revenue Cycle – Denials Management AuditPage 7 of 25
Executive SummaryWe would like to take the opportunity to thank the departments and individuals included in this audit for the courtesies extended to us and fortheir cooperation during our review.Sincerely,Valla F. Wilson, Associate Vice President for Internal Audit, Chief Audit ExecutiveAudit Team:Lori Muncy, Senior Internal AuditorGabriel Samuel, Senior Internal AuditorSunna Farooq, Internal AuditorJeff Kromer, Director, IT & Specialty Audit ServicesMelinda Lokey, Director of Internal Audit18:04 Revenue Cycle – Denials Management AuditPage 8 of 25
Executive Summarycc: Kate Conklin, Associate Vice President, Institutional Compliance & Chief Compliance OfficerMarisa Calder, Director, Front End Medical/Surgical Billing, Medical Group Billing Operations AdministrationArnim Dontes, Executive Vice President, Business AffairsKathryn Flores, Assistant Vice President and Chief Information Officer, University HospitalsSuresh Gunasekaran, Vice President and Chief of Operations for the UT Southwestern Health SystemLeslie Henderson, Assistant Director, Medical/Surgical Follow up, Medical Group Billing Operations AdministrationLisa High, Assistant Director Medical/Surgical Follow up, Medical Group Billing Operations AdministrationKelly Kloeckler, Associate Vice President, Revenue Cycle OperationsTim Leary, Assistant Director, HSIR Technical ServicesMark Meyer, Chief Financial Officer, University HospitalsMarc Milstein, Vice President and Chief Information OfficerMack Mitchell, M.D., Vice President, Medical AffairsTerry Neal, Director, Decision SupportLaShunda Murray, Manager, Patient Financial Services Revenue Cycle Operations, Patient Financial ServicesVinod Nair, Director, Revenue Cycle and Business SystemsJeffrey Petrie, Manager, Patient Financial Services Revenue Cycle Operations, Patient FinancialDennis Pfeifer, Assistant Vice President and Chief Technology Officer, Health SystemBrian Rasmus, Associate Vice President of Finance, Practice PlanMark Rauschuber, Associate Vice President and Chief Information Officer, Health SystemKrystal Richardson, Director, Revenue Cycle OperationsHaynie Sandle, Director Information Quality, Academic and Administrative Information ResourcesMichael Serber, Vice President, Financial AffairsJoshua Spencer, Associate Vice President and Chief Information Security OfficerThomas Spencer, Assistant Vice President, Information Resources Operations and ComplianceBrent Townsend, Director, Front End Medical/Surgical Billing, Medical Group Billing Operations AdministrationJohn Warner, M.D., Executive Vice President, Health System Affairs18:04 Revenue Cycle – Denials Management AuditPage 9 of 25
Detailed Observations and Action Plans MatrixObservationRecommendationManagement ResponseProfessional Denials Management Observations18:04 Revenue Cycle – Denials Management AuditPage 10 of 25
Detailed Observations and Action Plans MatrixObservationRecommendationManagement ResponseRisk Rating: High n1. Improve Timeliness of Review forProfessional Billing Denial Work QueuesAccounts in denial work queues are notconsistently cleared in a timely manner,resulting in delays in resubmitting claims topayers and increasing the risk of loss ofrevenue.As of December 31, 2017, 69% of the claimsamounts in the denial follow up work queueswere more than 90 days old. The followingcommon opportunities were identified ascontributing to delays in resolving denials andresubmitting claims to payors:-Monitoring tools are not consistentlyutilized by Supervisors to ensure workqueue accounts are analyzed andappropriate follow up procedures areperformed timely.1. Define supervisor monitoringexpectations for open denial accountsand work queues expectations.Management Action Plans:1. A project is being developed to streamlinethe denials management process toremove denials that are categorized asinformational only and will not result inadditional collections to the Medical Center.This will allow denial managementemployees to focus their efforts on denialsthat can be analyzed and resubmitted topayors to improve Medical Centercollections.Doing this will reduce the number of itemsin work queues so that supervisors canmonitor denials in accordance to standardoperating procedures (SOPs).Action Plan Owners:Associate Vice President, Revenue CycleOperationsDirector, Front End Medical/SurgicalBilling, Medical Group Billing OperationsAdministrationDirector, Revenue Cycle and BusinessSystemsTarget Completion Dates:Project plan completed by April 30th toinclude steps for implementation.18:04 Revenue Cycle – Denials Management AuditPage 11 of 25
Detailed Observations and Action Plans MatrixObservation--Escalation procedures are not clearlydefined to hold decentralized departmentaccountable for timely response fordenials transactions routed to beaddressed. When denials that arerequiring additional information fromdepartments are not addressed timely, itresults in write-offs. For example, adecentralized department had sixaccounts totaling 82,000 in denialsrequiring additional information that werenot submitted in a timely manner andrequired write off.Recommendation2. Develop escalation procedures andcoordinate with clinical departmentpersonnel for accountability to ensuredenials related requests for informationare completed in a timely manner.Management Response2. Develop SOP to communicate to billingmanagers when departments are notmeeting key goals (including denials), meetwith Department Administrator/Chair andescalate to Medical Group and HealthAffairs leadership as needed.Action Plan Owners:Associate Vice President, Revenue CycleOperationsDirector, Front End Medical/SurgicalBilling, Medical Group Billing OperationsAdministrationDenial analysis notes were not completedor did not provide details on next steps,which required additional review anddevelopment of plan to address denials.Target Completion Dates:Completed3. Define additional expectations fordenials teams for appropriate follow upactions including documentationrequirements and provide refreshertraining.3. Training will be updated and all follow-upteam members will be required to gothrough mandatory training programs.Action Plan Owners:Director, Front End Medical/SurgicalBilling, Medical Group Billing OperationsAdministrationTarget Completion Dates:Initial review post training to be completedby September 30, 2018 and ongoing18:04 Revenue Cycle – Denials Management AuditPage 12 of 25
Detailed Observations and Action Plans MatrixObservationRecommendation4. Perform periodic quality assurancereviews of open and closed denialrecords to ensure procedures arefollowed, expectations are met andidentify ongoing opportunities forrefresher training.Management Response4. Centralized department QA will be sharedwith team members to improve analysisand documentation.Action Plan Owners:Director, Front End Medical/SurgicalBilling, Medical Group Billing OperationsAdministrationTarget Completion Dates:July 31, 20185. Medical Group leadership shoulddevelop a plan to ensure qualityassurance functions are in place tomonitor and review decentralizeddepartment work queues.5. The Practice Plan CFO and AVP ofRevenue Cycle Operations will develop aplan to allocate a QA function to monitorand review decentralized department workqueues.Action Plan Owners:Associate Vice President of Finance,Practice PlanAssociate Vice President, Revenue CycleOperationsTarget Completion Dates:May 31, 201818:04 Revenue Cycle – Denials Management AuditPage 13 of 25
Detailed Observations and Action Plans MatrixObservationRecommendationManagement ResponseRisk Rating: Medium n2. Improve Work Queue Routing ChangeManagement ProceduresIncomplete Epic change managementprocedures (which would normally ensurechanges are tested, moved into the Productionenvironment and validated to ensure workingas intended) resulted in the erroneousreactivation of four work queues that had beenpreviously deactivated. This did not result inlost revenue, but caused confusion andinefficiencies for Revenue Cycle Operationsstaff, who did not realize these work queueshad been reactivated and contained deniedcharges forwarded by a clinical department tobe written off.Evaluate the error that occurred andimplement improvements to Epic changemanagement procedures to ensureinactivated follow-up work queues are noterroneously re-activated.Management Action Plans:Change management procedures will beupdated such that deactivated work queuerecords are blocked from future Data Couriermigration using the Epic Content Managementtool. In addition, going forward, work queuedeactivation changes will be classified as“Standard Changes,” which require qualityreview by HSIR Technical Services team priorto migration to the production environment.Action Plan Owners:Director, Revenue Cycle and BusinessSystemsAssistant Director, HSIR Technical ServicesTarget Completion Dates:April 30, 201818:04 Revenue Cycle – Denials Management AuditPage 14 of 25
Detailed Observations and Action Plans MatrixObservationRecommendationManagement ResponseRisk Rating: Medium n3. Update Security Access to the Epic HospitalBilling SystemRevenue Cycle Operations personnel workingprofessional denials have greater thanminimum necessary access to the EpicHospital Billing system when read only accessis necessary. The annual Epic security reviewprocess did not identify this as a necessaryadjustment.1. Update security access permissions forRevenue Cycle Operations personnelworking professional denials to allowonly read access to the Epic HospitalBilling system.Management Action Plans:1. We will review and update user templatesfor Revenue Cycle Operations personnelHospital Billing users as recommended.Action Plan Owners:Director, Revenue Cycle and BusinessSystemsTarget Completion Dates:Incomplete security access review can result ingreater than minimum necessary access toperform job duties.April 30, 20182. Coordinate with the Service Now team tomodify the Institutional Access Request(IAR) form if necessary to add any newroles created.2. If a change is needed to the IAR form, theServiceNow team will review the changewithin 30 days and then implement thechange within 60 days.Action Plan Owners:Director, Revenue Cycle and BusinessSystemsDirector Information Quality, Academic andAdministrative Information ResourcesTarget Completion Dates:July 31, 201818:04 Revenue Cycle – Denials Management AuditPage 15 of 25
Detailed Observations and Action Plans MatrixObservationRecommendationManagement ResponseHospital Denials Management Observations18:04 Revenue Cycle – Denials Management AuditPage 16 of 25
Detailed Observations and Action Plans MatrixObservationRisk Rating: High n4. Improve Timeliness of Review for HospitalDenial Work QueuesRecommendationManagement Action Plans:1. Define supervisor monitoringexpectations for open denial accountsand work queue expectations.Accounts in denial work queues are notconsistently cleared in a timely manner,resulting in delays in resubmitting claims topayers which increases the risk of loss ofrevenue.As of December 31, 2017, 50M (48%) of theaccounts in the work queues were aged over90 days. The following common opportunitieswere identified as contributing to delays inresubmitting claims to payors:--Management Response1. A project is being developed to streamlinethe denials management process toremove denials that are categorized asinformational only and will not result inadditional collections to the Medical Center.This will allow denial managementemployees to focus their efforts on denialsthat can be analyzed and resubmitted topayors to improve Medical Centercollections.Action Plan Owners:Associate Vice President, Revenue CycleOperationsMonitoring tools are not consistentlyutilized by supervisors to ensure workqueue accounts are analyzed andappropriate follow up procedures areperformed timelyChief Financial Officer, UniversityHospitalsDirector, Revenue Cycle OperationsDirector, Decision SupportDenial analysis notes were not completedor did not provide details on next steps,which required additional review anddevelopment of plan to address denial.Director, Revenue Cycle and BusinessSystemsTarget Completion Dates:Delays in analyzing denied accounts andinconsistent monitoring of work queue activitiesincreases the risk of loss of revenue.Project plan completed by April 30th toinclude steps for implementation.2. Develop escalation procedures andcoordinate with clinical departmentpersonnel for accountability for ensuringdenials related requests for informationare completed in a timely manner.Management Action Plans:2. Develop SOPs for metrics that are notmeeting goal and provide to Hospitalleadership for communication to thehospital department clinical leaders.18:04 Revenue Cycle – Denials Management AuditPage 17 of 25
Detailed Observations and Action Plans MatrixObservationRecommendationManagement Responsea. Metrics will be provided by theRevenue Cycle Operations teamand Hospital CFO and HospitalCOO will facilitate communicationswith hospital department clinicalleaders.Action Plan Owners:Associate Vice President, Revenue CycleOperationsChief Financial Officer, UniversityHospitalsDirector, Revenue Cycle OperationsTarget Completion Dates:CompletedManagement Action Plans:3. Define additional expectations fordenials teams for appropriate follow upactions including documentationrequirements and provide refreshertraining.3. Current training will be updated andadditional training will be provided to staffonce the project noted above is completed.Action Plan Owners:Associate Vice President, Revenue CycleOperationsDirector, Revenue Cycle OperationsDirector, Decision SupportTarget Completion Dates:Completed18:04 Revenue Cycle – Denials Management AuditPage 18 of 25
Detailed Observations and Action Plans MatrixObservationRecommendation4. Perform periodic quality assurancereviews of open and closed denialrecords to ensure procedures arefollowed, expectations are met andidentify ongoing opportunities forrefresher training.Management ResponseManagement Action Plans:4. Results of quality assurance reviews will bereviewed with team members as a part ofongoing training efforts.Action Plan Owners:Associate Vice President, Revenue CycleOperationsDirector, Revenue Cycle OperationsDirector, Decision SupportTarget Completion Dates:July 31, 2018Initial review post training to be completedby September 30, 2018 and ongoing18:04 Revenue Cycle – Denials Management AuditPage 19 of 25
Detailed Observations and Action Plans MatrixObservationRecommendationManagement ResponseRisk Rating: Medium n5. Improve Claim Processing Monitoring forthe Denial Account Watch ListNine hundred denial accounts that had beenanalyzed, corrected and submitted for rebillingto the payor did not map to a work queue andaccumulated in the “Denial Account Watch List”which is not consistently monitored. As a result,these claims were not rebilled in a timelymanner.Untimely monitoring of denied accounts in theWatch List increases the risk of loss ofrevenue.1. Update denial routing instructions toeliminate accounts that cannot bemapped to an existing work queue.2. Develop monitoring procedures toensure claims placed in the Watch Listare reviewed and cleared in a timelymanner.Management Action Plans:1. The project noted in #1 above will updatethe denial routing instructions.2. Information Resources in coordination withRevenue Cycle Supervisors will monitor thewatch list daily and will work any items onthis list within 24 hours.Action Plan Owners:Director, Revenue Cycle OperationsDirector, Decision SupportTarget Completion Dates:1. Project plan completed by April 30th toinclude steps for implementation2. Completed and Ongoing18:04 Revenue Cycle – Denials Management AuditPage 20 of 25
Detailed Observations and Action Plans MatrixObservationRecommendationManagement ResponseRisk Rating: Medium n6. Update Epic Security Access for HospitalClinical Denials TeamThe Hospital Clinical Denials team has greaterthan minimum necessary access to the EpicProfessional Billing system when read onlyaccess is necessary. The annual Epic securityreview process did not identify this as anecessary adjustment.1. Update security access permissions forthe all Hospital Billing system users withthe exception of the Specialty Billingteam to allow read only access to theProfessional Billing system. SpecialtyBilling should retain their update accessto the Professional Billing system.Management Action Plans:1. We will review and update user templatesfor all Hospital Billing users asrecommended.Action Plan Owners:Director, Revenue Cycle and BusinessSystemsTarget Completion Dates:Incomplete security access review can result ingreater than minimum necessary access toperform job duties.April 30, 20182. Coordinate with the Service Now team tomodify the Institutional Access Request(IAR) form if necessary to add any newroles created.2. If a change is needed to the IAR form, theServiceNow team will review the changewithin 30 days and then implement thechange within 60 days.Action Plan Owners:Director, Revenue Cycle and BusinessSystemsDirector Information Quality, Academic andAdministrative Information ResourcesTarget Completion Dates:July 31, 201818:04 Revenue Cycle – Denials Management AuditPage 21 of 25
Appendix A – Risk Classifications and DefinitionsAs you review each observation within the Detailed Observations and Action Plans Matrix of this report, please note that we have included a colorcoded depiction as to the perceived degree of risk represented by each of the observations identified during our review. The following chart isintended to provide information with respect to the applicable definitions and terms utilized as part of our risk ranking process:Degree of Risk and Priority of ActionRisk Definition- The degreeof risk that exists basedupontheidentifieddeficiency combined withthe subsequent priority ofaction to be undertaken bymanagement.PriorityAn issue identified by Internal Audit that, if not addressed immediately, has a highprobability to directly impact achievement of a strategic or important operationalobjective of a UT institution or the UT System as a whole.HighA finding identified by Internal Audit that is considered to have a high probabilityof adverse effects to the UT institution either as a whole or to a significantcollege/school/unit level. As such, immediate action is required by managementin order to address the noted concern and reduce risks to the organization.MediumA finding identified by Internal Audit that is considered to have a mediumprobability of adverse effects to the UT institution either as a whole or to acollege/school/unit level. As such, action is needed by management in order toaddress the noted concern and reduce the risk to a more desirable level.LowA finding identified by Internal Audit that is considered to have minimal probabilityof adverse effects to the UT institution either as a whole or to a college/school/unitlevel. As such, action should be taken by management to address the notedconcern and reduce risks to the organization.It is important to note that considerable professional judgment is required in determining the overall ratings presented on the subsequent pages ofthis report. Accordingly, others could evaluate the results differently and draw different conclusions. It is also important to note that this reportprovides management with information about the condition of risks and internal controls at one point in time. Future changes in environmentalfactors and actions by personnel may significantly and adversely impact these risks and controls in ways that this report did not and cannotanticipate.18:04 Revenue Cycle – Denials Management AuditPage 22 of 25
Appendix B – Denials TrendingThe following graphs provide top denial categories for both Hospital and Professional accounts. The underlying root causes for these categories arereviewed and shared with department personnel to provide feedback and education and improve denial rates going forward.Total Hospital denials in calendar 2017were 900M. The Top 5 categories are:Contract RelatedAdditional Information RequiredEligibilityCodingPast Filing Deadline58%21%17%2%2%Total Profes
18:04 Revenue Cycle - Denials Management Audit Page 4 of 25 Professional Denials Management For departments whose revenue cycle functions are within the centralized Revenue Cycle Operations, clinical denials are managed centrally by the Revenue Cycle Operations team reporting to the Associate Vice President of Revenue Cycle Operations.